两种胃肠吻合方式对胃癌Roux-en-Y重建效果影响
2020-11-16刘明哲马贵亮齐宏
刘明哲 马贵亮 齐宏

[摘要] 目的 对比分析胃后壁吻合和胃大弯侧残角吻合两种胃肠吻合方式对腹腔镜远端胃癌根治术Roux-en-Y重建效果影响。方法 收集2015年6月—2018年9月在本院普外科行腹腔镜远端胃癌根治术并行Roux-en-Y重建病人234例临床资料,按胃肠吻合位置不同分为胃后壁吻合组(观察组,n=93)、胃大弯侧残角吻合组(对照组,n=141),随访1年,比较两组病人临床及随访资料。结果 两组病人手术相关指标比较差异无统计学意义(Z=-1.87~-0.32,P>0.05),吻合口漏发生率、抗碱性反流能力等差异无统计学意义(χ2=0.00~0.70,P>0.05)。对照组胃瘫发生率与观察组比较差异无统计学意义(χ2=2.98,P>0.05)。对照组胃瘫严重程度高于观察组,差异有统计学意义(Z=-2.02,P<0.05)。结论 远端胃癌根治术Roux-en-Y重建时,行胃后壁吻合虽不能减少胃瘫发生,但对减轻胃瘫的严重程度有明显优势。
[关键词] 腹腔镜检查;胃切除术;吻合术,Roux-en-Y;胃肠吻合术
[中图分类号] R656.6+1 [文献标志码] A [文章编号] 2096-5532(2020)06-0696-04
doi:10.11712/jms.2096-5532.2020.56.134 [开放科学(资源服务)标识码(OSID)]
[网络出版] https://kns.cnki.net/kcms/detail/37.1517.R.20200706.1658.002.html;
[ABSTRACT] Objective To investigate the effect of posterior gastric wall anastomosis versus gastric greater curvature residual angle anastomosis on Roux-en-Y reconstruction after laparoscopic radical gastrectomy for distal gastric cancer. MethodsClinical data were collected from 234 patients who underwent laparoscopic radical gastrectomy and Roux-en-Y reconstruction in Department of General Surgery in our hospital from June 2015 to September 2018, and according to the site of gastrointestinal anastomosis, the patients were divided into posterior gastric wall anastomosis group (observation group with 93 patients) and gastric greater curvature residual angle anastomosis group (control group with 141 patients). All patients were followed up for 1 year, and the clinical and follow-up data were compared between the two groups. Results There were no significant differences in the operation-related indices between the two groups (Z=-1.87--0.32,P>0.05), and there were also no significant differences in the incidence rate of anastomotic leakage and the ability to resist alkaline reflux (χ2=0.00-0.70,P>0.05). There was no significant difference in the incidence rate of gastroparesis between the two groups (χ2=2.98,P>0.05), and the control group had significantly higher severity of gastroparesis than the observation group (Z=-2.02,P<0.05). Conclusion In Roux-en-Y reconstruction after laparoscopic radical gastrectomy for distal gastric cancer, posterior gastric wall anastomosis can not reduce the development of gastroparesis and has obvious advantages in reducing the severity of gastroparesis.
[KEY WORDS] laparoscopy; gastrectomy; anastomosis, Roux-en-Y; gastroenterostomy
胃癌好發于胃窦、幽门处,标准的根治性手术是其主要治疗手段[1-2]。腹腔镜用于治疗局部进展期胃癌的安全性和近、远期疗效逐渐被众多高质量多中心临床RCT研究所肯定[3-5]。在众多胃癌根治术消化道重建方式中,Roux-en-Y重建因具有良好的抗碱性反流、受肿瘤位置影响小等优势[6-7],成为本科室腹腔镜远端胃癌根治术后最主要的消化道重建方式。又因胃肠吻合位置差异分为胃后壁吻合及胃大弯侧残角吻合两种。目前,国内比较不同胃肠吻合位置对Roux-en-Y重建效果影响的研究甚少。本文回顾性分析我院普外科行腹腔镜远端胃癌根治术并行Roux-en-Y重建病人的临床资料,对比分析胃后壁吻合和胃大弯侧残角吻合两种胃肠吻合方式对腹腔镜远端胃癌根治术Roux-en-Y重建的影响。
1 资料与方法
1.1 一般资料
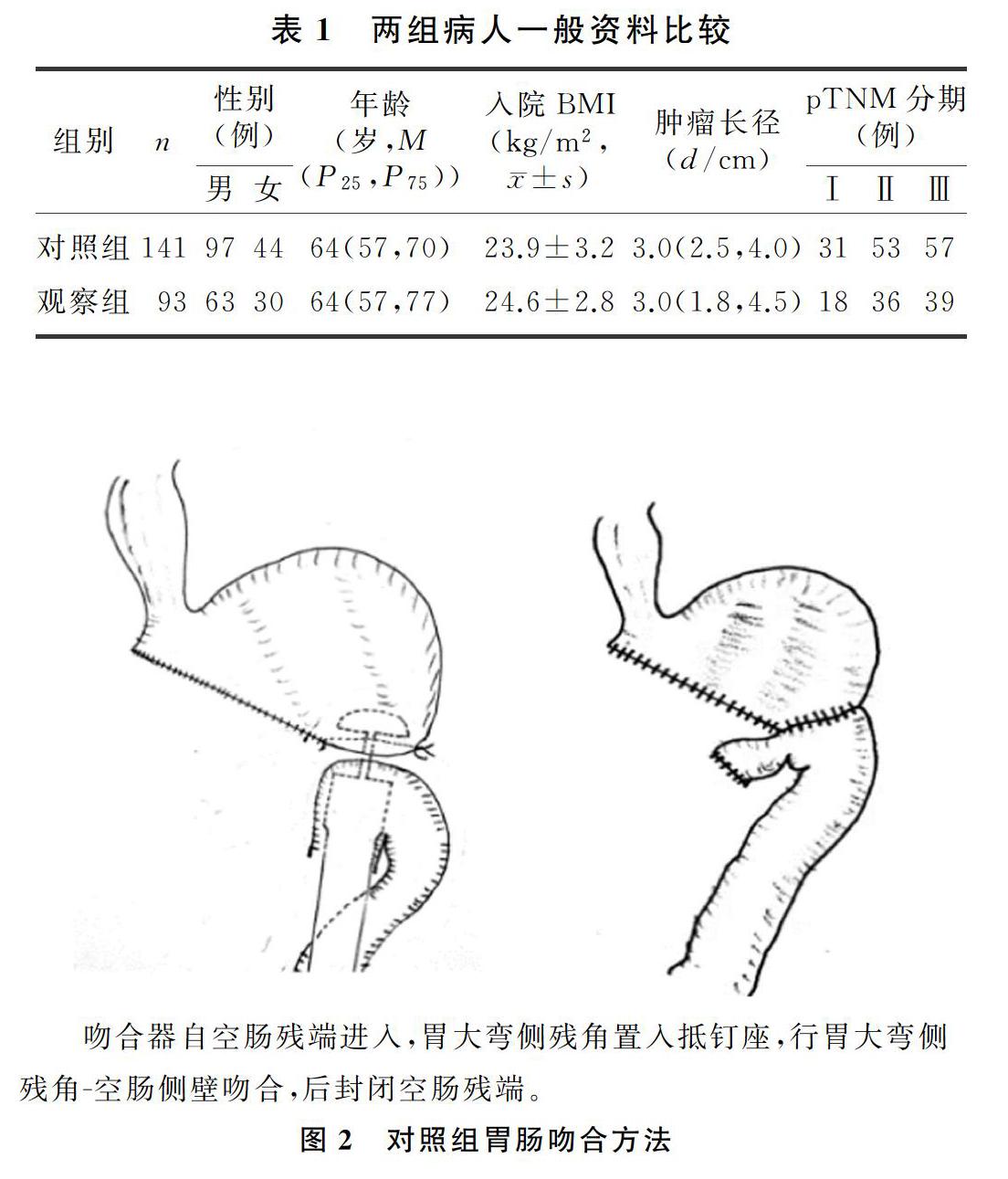
回顾性分析2015年6月—2018年9月在本院普外科行腹腔镜远端胃癌根治术病人临床资料。纳入标准:①术前诊断为胃窦、幽门处癌,并行腹腔镜远端胃癌根治术,未联合脏器切除;②行Roux-en-Y消化道重建;③不合并其他恶性肿瘤。排除标准:①急诊手术;②未达到D2根治;③术后随访资料不完整(未在术后1年复查胃镜、血生化检查、胸腹部CT等)。共入组病人234例,根据胃肠吻合位置将病人分为观察组(胃后壁吻合,n=91)、对照组(胃大弯侧残角吻合,n=143),两组病人的性别、年龄、入院时体质量指数(BMI)、肿瘤长径、肿瘤pTNM分期(第 8 版AJCC 胃癌分期)等一般資料比较差异无统计学意义(P>0.05)。见表1。
1.2 手术方法
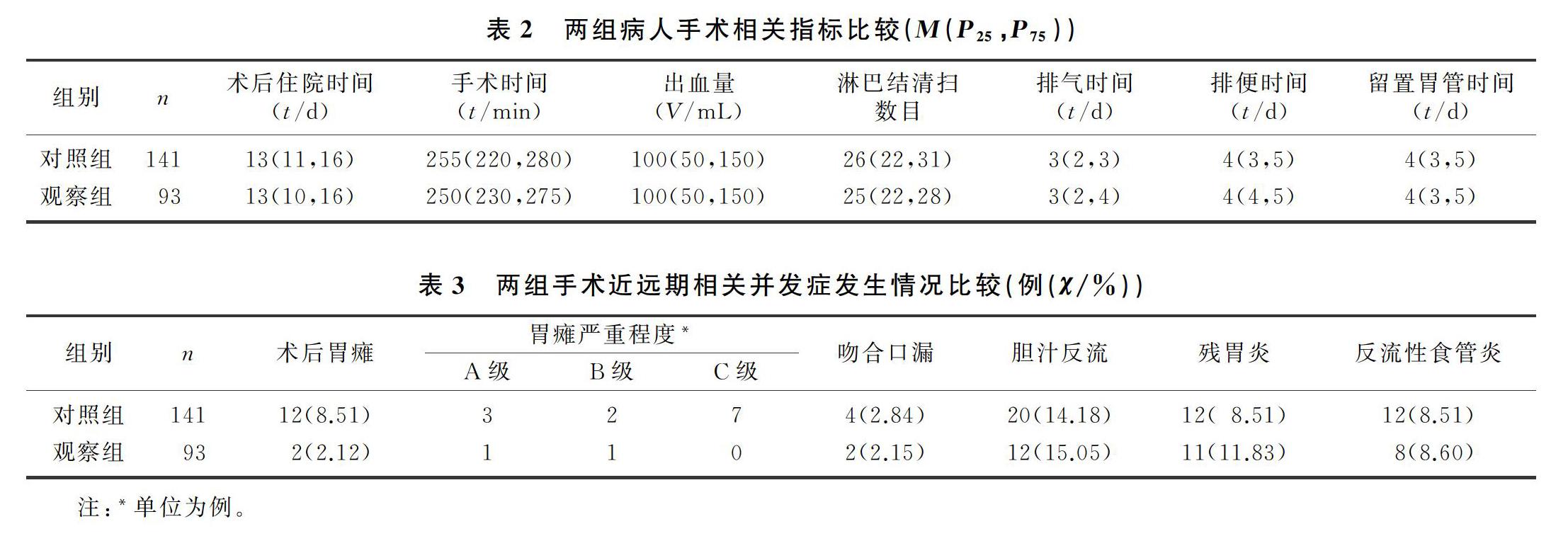
所有入组病人均按日本胃癌学会(JGCA)《胃癌治疗指南》第4版进行了腹腔镜远端胃癌根治术+D2淋巴结清扫术。两组病人除胃肠吻合部位不同外,其余操作一致。自Treiz韧带起始部15~20 cm离断空肠。观察组:自残胃置入管状吻合器钉杆,自胃后壁距离残端2~3 cm处穿出,行残胃-远端空肠吻合(图1);对照组:切开胃大弯侧残角置入吻合器抵钉座,远端空肠置入管状吻合器钉枪,行残胃-远端空肠端侧吻合(图2)。消化道重建: 距离胃肠吻合口40 cm处切开远端空肠,使用管状吻合器自空肠近端行空肠端-侧吻合。胃肠吻合采用直径29 mm管状吻合器进行吻合,空肠-空肠端侧吻合均采用24 mm管状吻合器吻合。
1.3 观察指标
观察两组病人的手术时间、淋巴结切除数目、术中出血量、术后首次排气时间、排便时间、术后胃管留置时间、术后住院时间等手术相关指标,以及吻合口漏、术后胃瘫、胃瘫严重程度分级、胆汁反流、残胃炎、反流性食管炎等手术近远期相关并发症的情况。胃瘫诊断标准:存在胃潴留症状,但是经一项或多项检查无胃流出道机械梗阻;持续10 d行胃减压,每天≥800 mL;无明显酸碱、水电解质紊乱;无引起胃瘫的基础疾病;无应用影响平滑肌收缩药物史[8]。胃瘫程度分级参照胰腺术后胃瘫分级方法[9],按术后留置胃管时间的长短将胃瘫严重程度分为A、B、C等3级。A级:诊断胃瘫,在14 d内可以拔除胃管并正常饮食;B级:术后14~21 d拔除胃管并恢复正常饮食;C级:术后21 d内未能拔除胃管并恢复稳定饮食。胆汁反流、残胃炎、反流性食管炎等根据术后1年复查胃镜检查结果进行诊断。
1.4 统计学分析
采用SPSS 24.0软件进行统计学分析。正态分布计量资料数据用±s表示,数据组间比较采用t检验;不符合正态分布的计量资料用中位数和四分位距表示,组间比较使用非参数检验。计数资料用百分比表示,数据间比较采用Pearson卡方检验或连续校正的卡方检验;有序变量比较采用秩和检验。P<0.05表示差异有统计学意义。
2 结 果
两组手术时间、淋巴结切除数目、术中出血量、术后首次排气时间、排便时间、术后胃管留置时间、术后住院时间等比较差异均无统计学意义(P>0.05)。两组病人的吻合口漏发生率、胆汁反流发生率、残胃炎发生率、反流性食管炎发生率等差异无统计学意义(P>0.05);对照组的胃瘫发生率(8.51%)与观察组(2.12%)比较差异亦无显著性(χ2=2.98,P>0.05);但两组胃瘫严重程度比较差异有显著意义(Z=2.02,P<0.05),见表2、3。
3 讨 论
远端胃手术破坏了消化道的连续性,术后重建至关重要。消化道重建的方式以BillrothⅠ式、BillrothⅡ式、Roux-en-Y式重建为主,各有优劣[10]。其中Roux-en-Y重建被认为是降低胆汁反流、残胃炎、反流性食管炎发生率的最佳选择[11-14]。既往研究中,国内学者多关注根治术后消化道重建方式对病人的影响。但是,消化道重建中的细节也可能带来不同的手术效果。
国外有研究显示,在Roux-en-Y重建中胃肠吻合位置可能会影响吻合口后端的流出道角度,流出道迂曲则会阻碍胃的排空,而流出道越竖直,越有利于胃中食物在重力作用下的排空[15]。而食物的刺激将进一步促进胃肠功能的恢复。KHAN等[16]对胰十二指肠切除术胃-空肠重建的研究显示,将胃-空肠吻合口穿过横结肠系膜置于结肠下区来避开术区,有效地减低了胃瘫的发生率及严重程度,考虑可能与减少局部炎症刺激,减轻吻合口水肿有关。局部炎症的直接刺激,会引起吻合口水肿,进而抑制胃的功能[17]。
就Roux-en-Y重建而言,胃-空肠吻合位置不同会导致吻合口的血供、吻合后流出道通畅程度、胃底与食管夹角的不同,进而可能会对病人术后胃肠功能恢复、围术期并发症的发生、抗碱性反流能力等产生影响;其对胃壁组织及神经的损伤程度也可能不同,胃的起搏区域位于胃体大弯侧,破坏起搏区域会引起慢波节律紊乱或消失[18],进而影响胃的运动。
本文的研究结果显示,腹腔镜远端胃癌根治术Roux-en-Y重建时,胃后壁吻合和胃大弯侧残角吻合的术中出血量、手术时间、淋巴结清扫数目、术后首次排气时间、排便时间、术后胃管留置时间、术后住院时间等差异均无统计学意义,两组病人胆汁反流、残胃炎、反流性食管炎的发生率差异亦无统计学意义。既往研究发现,远端胃癌根治术Roux-en-Y重建术后1年时的胆汁反流发生率2.8%~9.0%,残胃炎发生率28.0%~59.7%,反流性食管炎的发生率6.0%~14.0%[19-21]。本研究结果与其一致,提示胃后壁吻合对抗反流效果影响不大。对照组的胃瘫发生率(8.51%)是观察组(2.12%)的4倍,但两组差异无统计学意义;对照组胃瘫严重程度显著高于观察组。究其原因如下。①对胃体起搏区域及吻合处血供损伤小。行胃后壁吻合时,吻合口位于距离残端约2 cm处,距胃起搏区域相对较远,对胃体的起搏区域影响相对较小。而且避免了在同一位置的多次切割,对血供的影响相对较小,有利于减低吻合口漏发生率[22],也方便从胃残端观察吻合口有无出血情况[23]。②可能会减少吻合口附近炎症直接刺激。既往研究认为,根治术中可能会伤及胰腺被膜引起局部无菌性炎症,直接刺激吻合口会引起吻合口水肿,进而抑制胃肠活动。而行胃后壁吻合较胃大弯侧残角吻合更加远离术区,或许可以减少局部炎症对吻合口的刺激,有利于胃生理功能的恢复。③胃后壁吻合可能有更大的机会获得较为竖直的流出道,进而降低了胃瘫发生率及严重程度。具体情况需进一步前瞻性研究来验证。
综上所述,在腹腔镜远端胃癌根治术Roux-en-Y重建时,胃后壁吻合虽不能降低胃瘫发生率,但对减轻胃瘫的严重程度有明显优势。
[参考文献]
[1] 胡俊杰,熊治国. 胃癌远端胃切除术后消化道重建手术方式选择的再思考[J]. 临床外科杂志, 2019(5):376-378.
[2] SO J B, RAO J, WONG A S, et al. Roux-en-Y or billroth Ⅱ reconstruction after radical distal gastrectomy for gastric can-cer: a multicenter randomized controlled trial[J]. Annals of Surgery, 2018,267(2):236-242.
[3] YU J, HUANG C M, SUN Y H, et al. Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer:the CLASS-01 randomized clinical trial[J]. JAMA, 2019,321(20):1983-1992.
[4] LEE H J, HYUNG W J, YANG H K, et al.Short-term outcomes of a multicenter randomized controlled trial comparing laparoscopic distal gastrectomy with D2 lymphadenectomy to open distal gastrectomy for locally advanced gastric cancer (KLASS-02-RCT)[J]. Annals of Surgery, 2019,270(6):983-991.
[5] WANG Z Z, XING J D, CAI J, et al. Short-term surgical outcomes of laparoscopy-assisted versus open D2 distal gastrectomy for locally advanced gastric cancer in North China: a multicenter randomized controlled trial[J]. Surgical Endoscopy, 2019,33(1):33-45.
[6] CAI Z L, ZHOU Y, WANG C X, et al. Optimal reconstruction methods after distal gastrectomy for gastric cancer: a systematic review and network meta-analysis[J]. Medicine, 2018,97(20):e10823.
[7] MA Y P, LI F, ZHOU X, et al. Four reconstruction methods after laparoscopic distal gastrectomy: a systematic review and network meta-analysis[J]. Medicine, 2019,98(51):e18381.
[8] 秦新裕,劉凤林. 术后胃瘫的诊断与治疗[J]. 中华消化杂志, 2005,25(7):441-442.
[9] WENTE M N, BASSI C, DERVENIS C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested de-finition by the International Study Group of Pancreatic Surgery (ISGPS)[J]. Surgery, 2007,142(5):761-768.
[10] REN Z, WANG W X. Comparison of billroth Ⅰ, billroth Ⅱ, and Roux-en-Y reconstruction after totally laparoscopic distal gastrectomy: a randomized controlled study[J]. Advances in Therapy, 2019,36(11):2997-3006.
[11] BARR A C, LAK K L, HELM M C, et al. Linear vs circular-stapled gastrojejunostomy in Roux-en-Y gastric bypass[J]. Surgical Endoscopy, 2019,33(12):4098-4101.
[12] KIM M S, KWON Y, PARK E P, et al. Revisiting laparoscopic reconstruction for billroth 1 versus billroth 2 versus Roux-en-Y after distal gastrectomy: a systematic review and meta-analysis in the modern era[J]. World Journal of Surgery, 2019,43(6):1581-1593.
[13] YANG D, HE L, TONG W H, et al. Randomized controlled trial of uncut Roux-en-Y vs Billroth Ⅱ reconstruction after distal gastrectomy for gastric cancer: which technique is better for avoiding biliary reflux and gastritis[J]? World Journal of Gastroenterology, 2017,23(34):6350-6356.
[14] YANG K, ZHANG W H, LIU K, et al. Comparison of quality of life between Billroth-Ⅰ and Roux-en-Y anastomosis after distal gastrectomy for gastric cancer: a randomized controlled trial[J]. Scientific Reports, 2017,7(1):11245.
[15] MASUI T, KUBORA T, NAKANISHI Y, et al. The flow angle beneath the gastrojejunostomy predicts delayed gastric emptying in Roux-en-Y reconstruction after distal gastrectomy[J]. Gastric Cancer, 2012,15(3):281-286.
[16] KHAN A S, WILLIAMS G, WOOLSEY C, et al. Flange gastroenterostomy results in reduction in delayed gastric emptying after standard pancreaticoduodenectomy: a prospective cohort study[J]. Journal of the American College of Surgeons, 2017,225(4):498-507.
[17] 李世宽,周岩冰,于冠君. 远端胃大部切除术后胃排空延迟低发生率分析[J]. 青岛大学医学院学报, 2003,39(3):263-264,267.
[18] 李广华,叶锦宁,王昭,等. 术后胃瘫的治疗进展[J]. 消化肿瘤杂志(电子版), 2018,10(3):134-139.
[19] HE L R, ZHAO Y J. Is Roux-en-Y or Billroth-Ⅱ reconstruction the preferred choice for gastric cancer patients undergoing distal gastrectomy when Billroth Ⅰ reconstruction is not applicable? A meta-analysis[J]. Medicine, 2019,98(48):e17093. DOI:10.1097/MD.0000000000017093.
[20] HIRAO M, TAKIGUCHI S, IMAMURA H, et al. Comparison of Billroth Ⅰ and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer:one-year postoperative effects assessed by a multi-institutional RCT[J]. Annals of Surgical Oncology, 2013,20(5):1591-1597.
[21] OKUNO K, NAKAGAWA M, KOJIMA K, et al. Long-term functional outcomes of Roux-en-Y versus Billroth Ⅰ reconstructions after laparoscopic distal gastrectomy for gastric cancer: a propensity-score matching analysis[J]. Surg Endosc, 2018,32(11):4465-4471.
[22] 苏向前,周传永,杨宏. 新技术在胃癌手术应用中的并发症及其防治[J]. 中華胃肠外科杂志, 2017,20(2):148-151.
[23] 李浙民,李子禹. 胃癌全腹腔镜下消化道重建现状[J]. 国际外科学杂志, 2016,43(5):289-292.
(本文编辑 黄建乡)
