全泪道置管下泪道灌洗术对泪道阻塞性疾病患者眼表症状及复发率的影响研究
2020-11-09姚培好
姚培好

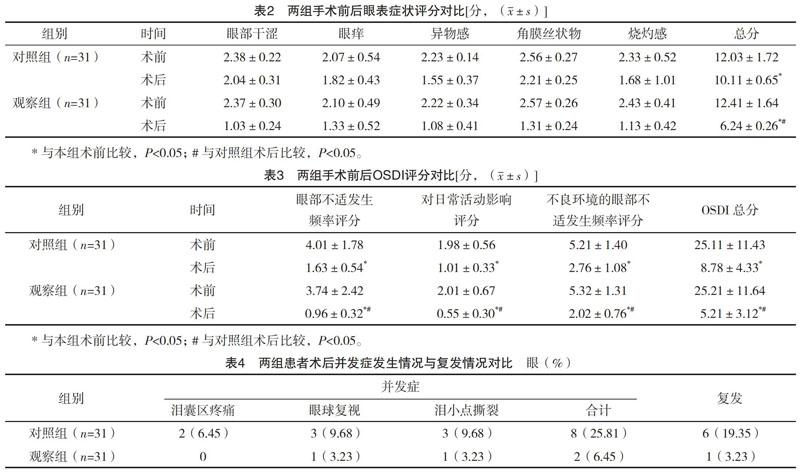
【摘要】 目的:研究全淚道置管下泪道灌洗术对泪道阻塞性疾病患者眼表症状及复发率的影响。方法:选取本院2017年5月-2019年5月收治的泪道阻塞性疾病患者50例62眼,根据治疗方法不同将其分为对照组24例31眼和观察组26例31眼。对照组给予传统泪道置管术治疗,观察组给予全泪道置管下泪道灌洗术治疗。对比两组术后临床疗效、眼表症状评分、眼表疾病指数量表(OSDI)评分及各参数评分、术中出血量、住院时间及复发率、并发症发生率。结果:术后,对照组临床总有效率80.65%,明显低于观察组96.77%(P<0.05);术后,两组患者眼部症状总分均低于术前,且观察组明显低于对照组(P<0.05);术后,两组患者OSDI总评分及眼部不适发生频率评分、对日常活动影响评分、不良环境的眼部不适发生频率评分均明显低于术前,且观察组均低于对照组(P<0.05);观察组术中出血量少于对照组,住院时间短于对照组(P<0.05);观察组的并发症发生率与复发率均低于对照组(P<0.05)。结论:全泪道置管下泪道灌洗术治疗泪道阻塞性疾病,可有效提高患者的治疗效果,改善眼部症状,降低并发症及再次手术的风险,值得临床推广应用。
【关键词】 泪道置管术 泪道灌洗术 泪道阻塞性疾病
[Abstract] Objective: To study the effect of lacrimal duct lavage under whole lacrimal duct catheterization on ocular surface symptoms and recurrence rate in patients with lacrimal duct obstruction. Method: From May 2017 to May 2019, 50 patients 62 eyes with lacrimal duct obstruction were selected, according to different treatment methods, they were randomly divided into control group (24 cases, 31 eyes) and observation group (26 cases, 31 eyes). The control group was treated with traditional lacrimal duct catheterization, the observation group was treated with whole lacrimal duct catheterization and lavage. The clinical effect, ocular surface symptom score, ocular surface disease index (OSDI) score, parameters score, intraoperative hemorrhage, length of stay, recurrence rate and complication rate were compared between the two groups. Result: After surgery, the total clinical response rate of the control group was 80.65%, which was significantly lower than 96.77% of the observation group (P<0.05). After surgery, the total score of ocular symptoms in both groups was lower than that before surgery, and the observation group was significantly lower than that of the control group (P<0.05). After surgery, the OSDI total score, the influence score on daily activities, eye discomfort frequency score, and eye discomfort frequency score of adverse environment in both groups were significantly lower than those before surgery, and the observation group were lower than those of the control group (P<0.05). The amount of intraoperative blood loss in the observation group was less than that in the control group, and the length of hospital stay was shorter than that in the control group (P<0.05). The complication rate and recurrence rate of the observation group were lower than those of the control group (P<0.05). Conclusion: The treatment of lacrimal duct obstruction by total lacrimal duct lavage can effectively improve the therapeutic effect of patients with lacrimal duct obstruction, improve ocular symptoms, reduce the risk of complications and reoperation, and is worthy of clinical application.
[Keys words] Lacrimal duct catheterization Lacrimal duct lavage Lacrimal duct obstructive disease
First-authors address: The Second Peoples Hospital of Gaozhou City, Gaozhou 525200, China
doi:10.3969/j.issn.1674-4985.2020.20.004
泪道阻塞性疾病是指由于各种原因所致泪液排除系统疾病引起泪溢或流脓[1]。目前国内外在泪道阻塞及泪道狭窄等眼科疾病的治疗方法不多,目前临床上最多见的是全泪道置管及鼻泪道置管的治疗方法,术后都是由上下泪点冲洗方式,进行冲洗,但常出现冲洗不充分,引起患者不适和复发率高的问题[2-3]。2014年本院首创自行设计可灌洗型全泪道研发,并成功实行全泪道置管下泪道灌洗术,现在经过100多例临床技术效果验证,使以上不足问题得到很好的解决,大大提高了疗效。本研究旨在探讨全泪道置管下泪道灌洗术治疗泪道阻塞性疾病的效果,现报道如下。
1 资料与方法
1.1 一般资料 选取2017年5月-2019年5月本院收治的泪道阻塞性疾病患者中50例62眼。纳入标准:(1)皆出现泪溢或流脓现象者;(2)以泪囊为中心蔓延至眼睑,出现红、肿、胀等情况者;(3)患者无言语障碍,可正常交流者。排除标准:(1)患有先天性眼部疾病者;(2)眼部遭受严重创伤或眼部周围出现皮肤破损者;(3)近期出现过眼部过敏史者;(4)患有急性结膜炎或泪囊炎者。根据治疗方法不同将其分为对照组(24例31眼)和观察组(26例31眼)。患者及家属对此次研究内容均知情同意。本院医学伦理委员会审核并通过本研究。
1.2 治疗方法 给予全部患者术前抗感染治疗,行副鼻窦CT检查及泪道冲洗,于术前15 min给予肾上腺素和利多卡因棉签填塞下鼻道,以扩大下鼻道、收缩下鼻甲、减少术中出血。患者取仰卧位,放置无菌铺巾,常规消毒眼部周围皮肤。
1.2.1 对照组 给予传统全泪道试管置管术,扩张上或下泪小点,黏膜表面麻醉,将带有硬膜外麻醉泪道硅胶导管的探针经泪道置入下鼻道,从泪道沟进入下鼻道,钩出鼻腔内的导丝,随即拔除探针,牵出导丝,同时将硅胶导管经下泪小点、泪小管、泪囊及鼻泪管从鼻腔导出,固定于前额,使用冲洗液冲洗,冲洗液不经过泪道置管管腔[4]。
1.2.2 观察组 在传统全泪管试管置管术的基础上行泪道灌洗术,将泪道试管更换为本院自制的可灌洗泪道试管,使用自制的加长加粗的泪道探通针、泪道置管探钩,具体手术步骤与对照组相同,冲洗时冲洗液从泪道置管管腔中进入,直接灌入泪囊中,然后分别从上下泪点及下鼻甲出口中冲出。
两组患者皆由相同的手术医生进行操作,术后全身应用抗生素预防感染3~5 d。冲洗液皆使用2 mg地塞米松磷酸钠注射液(生产厂家:北京双鹤药业股份有限公司,批准文号:国药准字H11020538,规格:1 mL︰2 mg)+4万单位硫酸庆大霉素注射液(生产厂家:武汉爱民制药有限公司,国药准字H42020096,规格1 mL︰4万单位)+4 mL 0.9%氯化钠注射液(生产厂家:必康制药江苏有限公司,批准文号:国药准字H20123045,规格:100 mL︰0.9 g)组成的混合液。前3 d由专业医生每日冲洗1次,出院后由专业的护士在门诊每周灌洗1次,3周后改为每个月灌洗1次,3个月后拔除泪道置管,拔管后随访3~5个月。
1.3 观察指标 (1)拔除泪道置管后对比两组手术疗效。泪道冲洗畅通没有阻力,泪囊脓肿消失,无溢泪溢脓情况为痊愈;泪道冲洗通畅有少许阻力,泪囊脓肿消退,无溢脓有溢泪情况为好转;泪道冲洗受阻,冲洗液返流为无效。总有效=痊愈+好转[5]。(2)对比两组术前术后眼表症状评分。按照眼部干涩、眼痒、异物感、角膜丝状物、烧灼感等症状进行评分,分为4个标准,0分为无、1分为轻度、2分为中度、3分为重度,计算总分,分数越高症状越严重[6]。(3)比較两组治疗前后眼表疾病指数量表(OSDI)评分及各参数评分。OSDI量表共12道问题,相对应的每题分数是0~4分,无须全部作答,最终依照患者回答的题数和每题的分数计算,总分=所有得分的总和×25/回答问题的数目,总分范围为0~100分。相关参数中眼部不适发生频率评分为0~20分,眼部不适对日常活动影响评分为0~16分,不良环境的眼部不适发生频率评分为0~12分[7-8]。(4)对比两组患者术中出血量、住院时间及拔除泪道置管后3~5个月内患者复发情况、并发症发生情况。
1.4 统计学处理 采用SPSS 21.0统计学软件对数据分析,计量资料用(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用字2检验。以P<0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较 对照组男12例15眼,女12例16眼;年龄30~65岁,平均(27.45±2.14)岁;患病时间0.5~8.0年,平均(4.37±1.67)年;其中单纯泪总管阻塞患者7例8眼,泪小管阻塞患者8例10眼,鼻泪管阻塞患者9例13眼。观察组男12例16眼,女14例15眼;年龄32~70岁,平均(28.04±1.43)岁;患病时间1~7年,平均(4.40±1.27)年;其中单纯泪总管阻塞患者7例9眼,泪小管阻塞患者9例10眼,鼻泪管阻塞患者10例12眼。两组患者一般资料比较,差异均无统计学意义(P>0.05),具有可比性。
2.2 两组手术疗效对比 术后,对照组临床总有效率为80.65%,低于观察组的96.77%,差异有统计学意义(字2=4.026,P=0.045),见表1。
[11]姜茂华.泪道引流管联合盐酸洛美沙星凝胶泪道内注射治疗泪道阻塞的疗效观察[J].重庆医学,2016,45(22):3129-3130.
[12]陈艳琼,蔡丽逢,刘晓俊,等.影响婴幼儿泪囊炎泪道冲洗探通疗效的相关因素分析及护理对策[J].中国实用护理杂志,2019,35(2):108-114.
[13] Mukhtar S A,Jamil A Z,Ali Z.Efficacy of External Dacryocystorhinostomy (DCR) with and without Mitomycin-C in Chronic Dacryocystitis[J].Ophthal Plast Recons,2014,24(10):732-735.
[14]钱江.泪道内镜与Nd-YAG泪道激光机对泪道阻塞性疾病的疗效对比分析[J].医学综述,2014,20(24):4599-4600.
[15]王华.改良的泪道引流管置管术治疗泪道阻塞性疾病的临床效果[J].江苏医药,2016,42(13):1504-1505.
[16] Liao R B,Zhang S H,Li N.Comparative study of two kinds of lacrimal drainage tubes for lacrimal duct obstruction[J].IES,2017,17(5):998-1001.
[17]叶健章,阮远飞,袁煜宗.改良泪道引流管置管术治疗泪道阻塞性疾病的临床效果[J].深圳中西医结合杂志,2018,28(6):186-188.
[18]李春.内窥镜辅助联合硅胶管置入治疗泪道阻塞性疾病护理及体会[C]//中国转化医学和整合医学学术交流会(上海站),2015:204-205.
[19]袁东兵.泪道置管术治疗泪道阻塞或狭窄的临床疗效及并发症处理分析[J].中外医疗,2017,7(30):76-77.
[20]周少博,谭娟,郭宇燕,等.新型泪道置管术治疗成人泪道阻塞疗效观察[J].中国实用眼科杂志,2017,35(7):704-707.
(收稿日期:2019-12-05) (本文編辑:张爽)
