Yiqi Huoxue Decoction in the treatment of Qi and yin deficiency and stasis type diabetic nephropathy in stage Ⅲ and its effect on VEGF and TGF-β1
2020-09-18ZhengFengLiYanLiHuangFengZhangLiangXiaoMinWuQiaoChenHuiZhang
Zheng-Feng Li, Yan-Li Huang, Feng Zhang, Liang Xiao, Min Wu, Qiao Chen, Hui Zhang
1.Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine,Nanchang, Jiangxi 330006
2.Jiangxi Institute of Occupational Disease Control,Nanchang, Jiangxi 330006
3.Jiangxi University of Traditional Chinese Medicine,Nanchang, Jiangxi 330004
Keywords:Diabetic nephropathy stage ⅢYiqi Huoxue Decoction Qi and Yin deficiency stasis VEGF TGF-β1
ABSTRACT Objective: To observe the efficacy of Yiqi Huoxue Decoction in the treatment of patients with diabetic nephropathy (DN) stage Ⅲ with qi and yin deficiency and stasis and its effects on vascular endothelial growth factor (VEGF) and transforming growth factor-β (TGF-β1). Methods: Sixty patients with stage DN of Qi-yin deficiency and stasis type DN who were treated in the Endocrinology Department of the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine from September 2018 to December 2019 were selected as the research subjects.The remainder method was used to divide them into 30 cases in the observation group and 30 cases in the control group. Patients in both groups were referred to the guidelines and expert consensus for general treatment of DN (hypogl- ycemic,antihypertensive,lipid-lowering,etc.).The control group was given pancreatic kallikrein enteric-coated tablets orally once,120U,3 times a day,and the observation group was given The traditional Chinese medicine Yiqi Huoxue Decoction was taken orally,one dose daily,twice a day in the morning and evening;the two groups intervened continuously for 8 weeks.Detect blood FPG,PBG,HbA1c,β2-MG,BUN,SCr,VEGF,TGF-β1,and urine mALB and UACR levels before and after treatment, and calculate eGFR before and after treatment in both groups; observe changes in TCM syndrome scores in the two groups,Compare its clinical efficacy. Results: After 8 weeks of treatment,the total clinical effective rate of patients in the observation group was 93.3%,which was significantly different from the control group of 76.6% (P<0.05);the TCM syndrome scores in the observation group were significantly lower than those before treatment and in the control group (P<0.05); The levels of FPG,HbA1c,PPG,mALB,β2-MG,UACR, VEGF,and TGF-β1 in the observation group were significantly lower than those in the control group, with significant differences (P<0.05).The levels of SCr and BUN in the observation group were significantly lower. Compared with before treatment, eGFR increased, but there was no signi- ficant difference (P>0.05). Conclusion: Yiqi Huoxue Decoction for the treatment of patients with DN type Ⅲ qi-yin deficiency and stasis type,not only helps to lower blood sugar levels,improve TCM syndromes,but also can reduce early renal damage,reduce urine albumin, and delay kidney function It may be further worsened and has better safety. The mechanism may be related to reducing the levels of VEGF and TGF-β1,thereby delaying the fibrosis of tubulointerstitial scar and inhibi- ting glomerular capillary sclerosis.
1. Introduction
Diabetic nephropathy (DN) Stage Ⅲ is the early stage of DN,and typically manifested by microalbuminuria,, Glomerular filtration rate generally normal[1].If timely and effective intervention and control are not available at this stage, kidney function will be exacerbated, which can cause a significant increase in proteinuria and serum creatinine levels, and eventually form end-stage renal disease,which requires renal replacement therapy [2].Not only reduces the quality of life of patients, increases the psychological burden, increases medical costs,and the gradual decline in renal function also continuously increases the risk of cardiovascular disease and all-cause death [3].There are still many differences in the explanation of the pathogenesis of DN in western medicine and different pathogenesis theories.Therefore,the current treatment can only be based on symptomatic support,the efficacy is often poor, and there are many side effects,and the subjective symptoms of patients are not obvious[4].Traditional Chinese medicine has a long history of preventing and treating diabetes and its related complications,and has irreplaceable advantages.Yiqi Huoxue Decoction is a former leader of the endocrinology Department in the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine. In more than 30 years of clinical practice,it was combined with the pathogenesis and disease character- istics of DN,and has been used in the treatment of early DN patients with satisfactory results.Therefore,the purpose of this study is to explore the effect of Yiqi Huoxue Decoction on the phaseⅢ of DN of Qi and Yin deficiency and blood stasis and its effect on blood VEGF and TGF-β1 on the basis of clinical practice,and try to study the possible mechanism of its treatment for DN stage Ⅲ.
2. Materials and methods
2.1 Basic information
Sixty patients with stage DN of qi-yin deficiency and stasis type DN who were treated in the endocrinology department of the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine from September 2018 to December 2019 were selected as the research subjects. The remainder method was used to divide the control group into 30 cases and observe. Group of 30 patients. In the observation group, there were 13 females and 17 males, aged 42-69 years, with an average (58.67±5.84) years of age, the duration of DM was 5-11 years, the average was (9.83 ±7.65) years, and the duration of DN was 8-22 months, the average (15.54 ±4.23) months. There were 11 females and 19 males in the control group, aged 40-70 years, with an average (57.93±5.15) years of age, with a DM course of 7-12 years, with an average (10.71±6.43) years; DN with a course of 6-21 months, with an average (14.93±4.56) months. The basic data of the two groups were compared (P>0.05).The baseline characteristics were consistent and comparable.
2.2 Diagnostic criteria
2.2.1 Western medicine diagnostic criteria
DM diagnosis refers to the "Guidelines for the Prevention and Treatment of Type 2 Diabetes in China (2017 Edition)" [3], and DN diagnosis refers to the "Expert Consensus for the Prevention and Treatment of Diabetic Nephropathy (2014 Edition)" [5]: DM history of 5 years or more With or without DM retinopathy; within 6 months, two consecutive UACR> 30mg/g or UAER> 20ug/min, or mALB>30mg/24h, or urine ALB quantitative>0.5g/d, while excluding other causes Kidney damage and abnormal renal function. DN Stage Ⅲ diagnosis of Danish Mogensen standards [6]: GFR is generally normal;UAER is 30-300mg /24h for more than 3 consecutive months.
2.2.2 TCM diagnostic criteria
The DN standard of Qi-Yin deficiency and stasis type refers to "Diagnosis,Syndrome Differentiation, and Efficacy Evaluation Standards(Trial Scheme) for Diabetic Nephropathy" [7]: Main Symptoms: Burnout,fatigue, low voice, limb Weakness, shortness of breath, dry mouth,dry throat, spontaneous sweating, night sweats,upset and insomnia,five upset fever;secondary card:dizziness or dizziness, chest tightness,palpitation,premature ejaculation,pale or dark complexion, wrong skin,wrong limbs or Pain;Tongue: dark red tongue and thin body,thin or yellow tongue coating;Pulse:Shen pulse is thin or weak.Satisfying 3 main cards,or 2 main cards +2 sub-cards,can be identified as DN of Qi and Yin deficiency and stasis type.
2.3 Inclusion criteria
①meet the above diagnostic or dialectical conditions; ②40-70 years of age, regardless of gender;③ approved by the hospital ethics committee.
2.4 Exclusion criteria
①TCM dialectics does not belong to the type of qi-yin deficiency and stasis;②patients with type 1 diabetes or other autoimmune diabetes with unclear type;③abnormal renal function occurs earlier than diabetes and other causes of renal impairment ④Those who are allergic to pancreatic kininogenase and any component in Yiqi Huoxue Decoction;⑤Those who have acute complications such as DKA, HHS;⑥Those who have severe liver,lung,and heart dysfunction;⑦Pregnant women and lactating patients;⑧Those who do not have full autonomy to cooperate with syndrome scores and treatment.
2.5 Treatment methods
Both groups of patients were referred to the guidelines and expert consensus [5] for routine comprehensive treatment, including strengthening related knowledge and education,high-quality protein diet and diabetes diet,appropriate exercise,weight loss,oral medication or insulin injection to control sugar,high blood pressure Patients with oral antihypertensive drugs,those with abnormal lipidmetabolism were lipid-regulated by statins,and patients with vascular disease and aspirin antiplatelet aggregation.The control group was given pancreatic kallikrein enteric-coated tablets (Changzhou Qianhong Biochemical Pharmaceutical Co.,Ltd,120u*24tablets, Sinopharm H19993089) on the basis of conventional treatment,orally,120U once,3 times a day;the observation group was Traditional Chinese medicine Yiqi Huoxue Decoction (Astragalus 20g,Codonopsis 20g,Polygonatum 20g,Saffiower 10g,Chuanxiong 10g,Atractylodes 10g, Habitat 10g,Pueraria 10g,Zhizhi Ren 30g,Dilong 10g,Morinda officinalis 10g) Take orally,add or subtract with the card, if you have edema, add Poria, Achyranthes bidentata, and Alisma diarrhea;if you have constipation,add Rhubarb;take 1 dose daily,soak each Chinese medicine with about 400ml of water,and cook for 2 times,mix Take about 200ml of juice and take it two times in the morning and evening; the above Chinese medicines are all from the small package pharmacy of the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine (Jiangxi Province Traditional Chinese Medicine Hospital) to ensure the consistency of the manufacturer and the batch number. Patients in both groups were treated continuously for 8 weeks.
Table 1 Comparison of Syndrome Scores of Qi-Yin Deficiency Syndrome and Stasis Syndrome (±s,points)

Table 1 Comparison of Syndrome Scores of Qi-Yin Deficiency Syndrome and Stasis Syndrome (±s,points)
Note: Compared with the control group, *P<0.05
Groups N Before treatment After treatment Observation group 30 28.52±7.81 10.22±4.79*Control group 30 29.17±6.59 20.43±6.57

Table 2 Clinical efficacy of the two groups (%)
Table 3 Comparison of FBG, PBG, HbA1C between the two groups(±s)
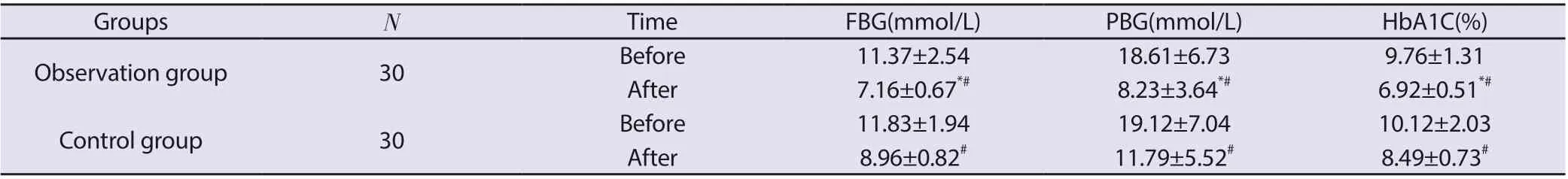
Table 3 Comparison of FBG, PBG, HbA1C between the two groups(±s)
Note: Compared with the control group, * P<0.05; compared with before treatment, #P<0.05.
Groups N Time FBG(mmol/L) PBG(mmol/L) HbA1C(%)Observation group 30 Before 11.37±2.54 18.61±6.73 9.76±1.31 After 7.16±0.67*# 8.23±3.64*# 6.92±0.51*#Control group 30 Before 11.83±1.94 19.12±7.04 10.12±2.03 After 8.96±0.82# 11.79±5.52# 8.49±0.73#
Table 4 Comparison of mALB, β2-MG and UACR between the two groups (±s)
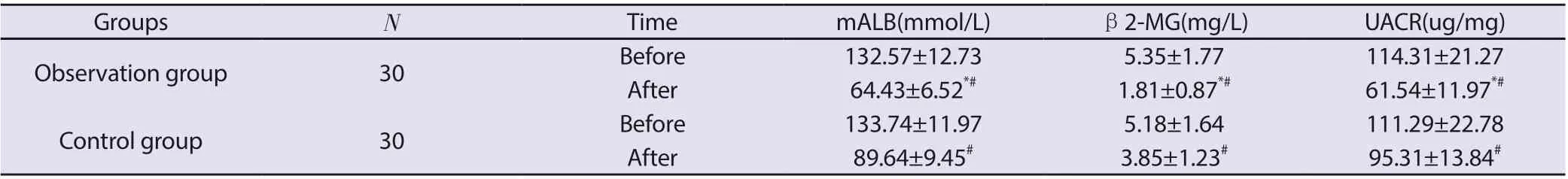
Table 4 Comparison of mALB, β2-MG and UACR between the two groups (±s)
Note: Compared with the control group, *P <0.05; compared with before treatment, #P<0.05.
Groups N Time mALB(mmol/L) β2-MG(mg/L) UACR(ug/mg)Observation group 30 Before 132.57±12.73 5.35±1.77 114.31±21.27 After 64.43±6.52*# 1.81±0.87*# 61.54±11.97*#Control group 30 Before 133.74±11.97 5.18±1.64 111.29±22.78 After 89.64±9.45# 3.85±1.23# 95.31±13.84#
2.6 Observation indicators
①Efficacy indicators: Before treatment and after 8 weeks of treatment,the fasting venous blood of the patient was taken, and the automatic biochemical analyzer was used to detect glycated hemoglobin (HbA1C)and fasting blood glucose(FBG).The patients were taken after normal eating 2 Hourly venous blood,the same method was used to detect blood glucose (PBG) at 2 hours after meals;ELISA was used to determine serum β2 microglobulin (β2-MG),vascular endothelial growth factor (VEGF)[8],transforming growth factor-β(TGF- β1)levels[9];take 10 mL of fresh morning urine from patients,measure urinary microalbumin (mALB)levels by ELISA,determine urinary creatinine content by colorime- try,and find the urinary albumin to creatinine ratio(UACR).②Safety indicators:The application of automatic biochemical analyzers such as blood creatinine(SCr)and urea nitrogen (BUN),and the use of MDRD formula to calculate eGFR to evaluate the renal function of patients;all the above tests were performed in accordance with the uniformity of the Biochemical Laboratory of the Affiliated Hospital of Jiangxi University of Traditional Chinese Medicine Requirements and standards implemen- tation. ③TCM syndrome scores[10],the two groups of patients are scored according to the main and secondary symptoms of DN of Qi and Yin deficiency and stasis type,and the main syndromes are counted from none,light, moderate and severe,0,2,4,and 6 respectively points; sub-cards are scored as0,1,2,and 3 respectively according to none,light,moderate,and severe; tongue pulses are greatly affected by personal subjective feelings and are not included in the scope of TCM syndromes.
2.7 Efficacy evaluation
Refer to the literature [10] according to the degree of improvement of TCM syndrome scores after treatment of patients:first calculate the syndrome improvement rate(m)=(before treatment-after treatment)/before treatment points*0.01.Significant effect:Significant reduction or disappearance of related symptoms,significant improvement in signs, m≥70%; Effective: Significant improvement in related symptoms, signs improvement,m≥30%;Ineffective: No reduction in related symptoms, signs, or even exacerbation,m<30%.
2.8 Statistical methods
SPSS 22.0 was used for statistical analysis.The t-test was used to compare the count data between the two groups with normal distribution,and the comparison was performed using the 2 test; P<0.05 indicated significant significance.
3. Results
3.1 Comparison of Syndrome Points of Qi-Yin Deficiency Clip Stasis Syndrome in Two Groups
Before treatment,the scores of Qi and Yin deficiency and stasis syndrome were higher in both groups, and there was no significant difference between the observation group and the control group (P>0.05). After treatment, the scores of both groups were lower than before. However, the scores of patients in the observation group were significantly lower than those in the control group, with significant differences (P<0.05), in Table 1.
Table 5:Comparison of SCr, BUN, eGFR between the two groups(±s)

Table 5:Comparison of SCr, BUN, eGFR between the two groups(±s)
Note: Compared with the control group, * P <0.05; compared with before treatment, #P<0.05.
Groups N Time SCr(umol/L) BUN(mmol/L) eGFR(ml/min·1.73m3)Observation group 30 Before 114.33±19.56 10.27±1.26 89.75±10.74 After 105.44±13.86 9.86±0.91 91.63±7.84 Control group 30 Before 112.85±18.77 11.36±1.33 90.94±11.53 After 109.79±15.56 10.58±1.15 88.24±7.56
Table 6:Comparison of VEGF and TGF-β1 levels between the two groups(±s)
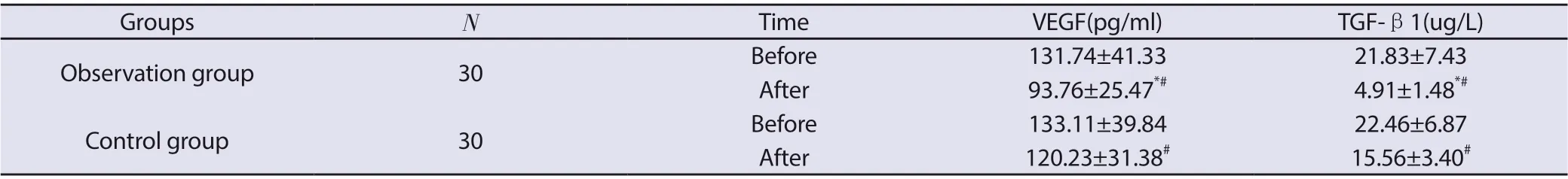
Table 6:Comparison of VEGF and TGF-β1 levels between the two groups(±s)
Note: Compared with the control group, * P <0.05; compared with before treatment, #P<0.05.
Groups N Time VEGF(pg/ml) TGF-β1(ug/L)Observation group 30 Before 131.74±41.33 21.83±7.43 After 93.76±25.47*# 4.91±1.48*#Control group 30 Before 133.11±39.84 22.46±6.87 After 120.23±31.38# 15.56±3.40#
3.2 Comparison of clinical efficacy of TCM between the two groups
After 8 weeks of treatment, the total effective rate in the control group was 76.6%,and the observation group was 93.3%,which was significantly higher than the control group,with a significant difference (P<0.05).in Table 2.
3.3 Comparison of blood glucose related indicators FBG, PBG, HbA1C between the two groups
Before treatment, the levels of FBG,PBG,and HbA1C were higher in the two groups,and there was no significant difference between the groups (P>0.05).After 8 weeks of treatment,the levels of FBG,PBG,and HbA1C in the two groups were lower than before.The previous comparisons had significant differences (P<0.05);however,the levels of FBG,PBG,and HbA1C in the observation group were significantly lower than those in the control group,with significant differences(P<0.05),in Table 3.
3.4 Comparison of early renal function indicators mALB, β2-MG, UACR between the two groups
Before treatment, the levels of mALB,β2-MG,and UACR were higher in the two groups,and there was no significant difference between groups (P>0.05). After 8 weeks of treatment, the levels of mALB,β2-MG,and UACR were higher in the two groups Compared with before treatment, there were significant differences (P<0.05);but the levels of mALB,β2-MG,and UACR in the observation group were significantly lower than those in the control group,with significant differences (P<0.05),as shown in Table 4.
3.5 Comparison of safety indicators SCr,BUN,eGFR between the two groups
Before treatment,the levels of SCr,BUN,and eGFR were higher in the two groups, and there was no significant difference between the groups (P>0.05).After 8 weeks of treatment,the levels of SCr and BUN in the two groups were lower than before and compared with before treatment.There were no significant differences (P>0.05);eGFR in the observation group was slightly higher than before treatment,but the difference was not significant (P>0.05).There was no significant difference in the levels of SCr,BUN,and eGFR in the two groups (P>0.05).in Table 5.
3.6 Comparison of levels of VEGF and TGF-β1 in renal interstitial fibrosis between the two groups
Before treatment, the levels of VEGF and TGF-β1 were higher in the two groups, and there was no significant difference between the groups (P> 0.05).After 8 weeks of treatment, the levels of VEGF and TGF-β1 in the two groups were lower than before.The previous comparisons had significant differences (P<0.05);but the levels of VEGF and TGF-β1 in the observation group were significantly lower than those in the control group, with significant differences (P<0.05),in Table 6.
4. Discussion
The pathogenesis of DN is complicated,At present, it is mainly believed that long-term hyperglycemia, glucose and lipid metabolism disorders, hypertension and other factors in diabetics stimulate the kidney microvascular vessel wall deposits to increase,cause damage to vascular endothelium,and cause renal hemodynamic changes,Inflammation and oxidative stress reactions, advanced glycosylation products, various cytokines and growth factors are activated,the fibrinolytic system is unbalanced,the body appears hypercoagulable, abnormal oxygen radicals are eliminated, and the accumulation of advanced glycosylation products causes Disturbance of renal microcirculation leads to the occurrence of DN [11-12].Its early pathological changes were glomerular hypertrophy, increased permeability and ultrafiltration,and the extracellular matrix of the renal tubules became sclerotic, that is,fibrosis, which eventually caused the deterioration of renal function [13].Pancreatic kininogenase is a vasodilator that mainly improves microcirculation and has multiple pharmacological effects such as reducing the viscosity of whole blood. It is consistent with many pathogenesis of DN,so it is commonly used in the treatment of DN in the clinic[14],its treatment of DN has a good effect, so in this study,pancreatic kininogenase enteric-coated tablets were taken orally as a control study.
DN can be attributed to the "lower consumption" category.The occu- rrence of this disease is mostly caused by patients with inadequate diet or excessive fat and spleen and stomach damage,spleen deficiency, spleen accumulation,and endogenous heat.It can also be caused by emotional disorders,liver Stagnation of qi and stagnation,and heat over time;fiery scorching,stagnation and yin,and yin deficiency and dryness.In addi- tion ,yin deficiency and hotness are most likely to consume gas,and cause anger,and cause qi deficiency and qi and yin deficiency.Qi is the comman- der of blood.The normal operation of blood in the blood vessels depends on the filling and promotion of the human body.However,the maintenance defaults,the blood line is difficult,and the evidence of blood stasis appears over time.And it can take blood,qi deficiency will take blood for dereliction of duty,blood does not return to menstruation,blood spills out of the veins,and damage to the veins is also one of the causes of blood stasis.The kidney is the innate foundation.It contains the elements of yin and yang,and the qi and blood of the human body are damaged.The kidney is sealed,and the kidney qi is deficient.The fine substance leaks out of the urine,and proteinuria appears.At the same time, the kidney is dir- ty,and the kidney is open,and the kidney is deficient.Normalized and accumulated in the body,some patients may show the appearance of edema [15].It can be seen that the disease syndrome is the essence of deficien- cy,which is the deficiency of qi and yin,and the deficiency of stasis and blood stasis.When the specimen is taken into account,the method of strengthening the spleen,strengthening qi,nourishing yin,and activating blood circulation and removing blood stasis is the method.The Yiqi Huoxue Decoction formula fully combines the pathogenesis of DN with traditional Chinese medicine,and refers to the essence of "Shenqi Dihuang Decoction" in the prescription of "Miscellaneous Diseases and Rhizoma",and is set up for the pathogenesis of DN with Qi and Yin deficiency and stasis.The main drug is Codonopsis,which is good at nourishing the spleen,nourishing the qi and nourishing the stomach, and also being able to regenerate.It has the characteristics of "spleen nourishing the spleen and nourishing the stomach but not wet." It is the "first medicine for spleen replenishing qi and strengthening the spleen".It is often used with Codonopsis to strengthen the function of nourishing qi.Astragalus is the medicine for replenishing qi and qi.It is also the medicine for treating qi deficiency and edema.Instead of being dry,traveling around the body can double the power of strengthening the spleen and replenishing qi,while also having a beneficial effect on water and swelling.Shengdihuang enters the kidney meridian to nourish yin and lower fire,nourish yin and nourish jin,and use it together with Codonopsis,Atractylodes and Astragalus to achieve the effect of nourishing qi and nourishing yin.Pueraria root has a pungent taste,is in the lungs and stomach meridian,and is good at nourishing yin and nourishing fluids.Cooperating with the habitat,it can enhance the power of nourishing yin.Chuanxiong and saffiower are for promoting blood circulation and removing blood stasis.It is designed for blood stasis. Huang Jing is a product of qi and yin tonic,which is good at strengthening the spleen and nourishing qi,nourishing yin and nourishing kidney, and taking into account both the disease position and the pathogenesis of the disease at the same time. Zhiren Ren,Morinda officinalis and Wenwen products supplement Yang and Yin,taking the meaning of "Yang in seeking Yin".All the above medicines work together to strengthen the spleen and nourish qi,nourish the kidney and nourish yin, promote blood circulation, and remove stasis.At the same time, modern pharmacological studies have also shown that astragaloside IV can increase the autophagy activity of renal tissue cells in type 2 diabetic nephropathy rats, thereby delaying the progression of DN
[16].Other studies have found that astragalus may affect DN mice by down-regulating the expression of PERK pathway proteins, which can not only reduce their body weight,but also reduce renal function damage [17]. Experimental studies have shown that Shengdi can reduce fasting blood glucose and 24-hour urine protein levels in SD rats,and has a certain preventive effect on diabetic nephropathy [18].Liu Yuanping [19] and others reported that puerarin can significantly improve the levels of oxidative stress factors and inflammatory factors such as serum superoxide dismutase (SOD) and malondialdehyde (MDA) in elderly DN patients.Peng Jing [20] pharmacological research found that saponin can reduce blood creatinine,urea nitrogen levels and the expression of type IV collagen and Wnt4 β-catenin in DN rats,thereby blocking the proliferation and differentiation of renal fibroblasts Inhibits tubulointerstitial scar sclerosis,thereby protecting the structure and function of the kidney. At the same time,Xie Yiqiang [21] and other studies have proved that Yizhi Ren Ti inhibits the synthesis of p27kip protein in kidney tissues of DN mice,and achieves kidney protection.It can be seen that the combined application of the above medicines and the scientific prescription of the medicine not only accord with the pathogenesis of DN of deficiency and stasis of Qi and Yin in traditional Chinese medicine,but also have sufficient evidence in modern pharmacological research,which fits the pathogenesis of DN,and thus can achieve good therapeutic effects.In this study, based on conventional treatment, Yiqi Huoxue Decoction was used to treat patients with stage DN of qi-yin deficiency and stasis DN.The total clinical effective rate was 93.3%, which was significantly different from 76.6% in the control group.Moreover,the symptoms and signs related to the syndrome of qi and yin deficiency and stasis were significantly relieved compared with the control group.At the same time, the levels of FPG, HbA1c, PPG, mALB,β2-MG,and UACR were significantly reduced,which had a positive effect and did not cause SCr,The increase of BUN level and the decrease of eGFR have good safety.This shows that Yiqi Huoxue Decoction not only helps to reduce the blood glucose level of DN stage Ⅲ,but also relieves the subjective symptoms of patients,that is,the clinical symptoms of traditional Chinese medicine. Prevent further deterioration of renal function and promote the recovery of renal function to a certain extent.
VEGF is an important substance that induces angiogenesis,endothelial proliferation,and survival.It is also called vascular permeability factor.Normal levels of VEGF in the body are beneficial to the integrity and effectiveness of blood vessels in maintaining their functions and states.However,under the action of multiple mechanisms with hypergly- cemia as the starting factor,diabetic patients have abnormally elevated VEGF levels in the body,a large amount of VEGF binds to its receptors, and then induces the division,migration and chemotaxis of endothelial cells in various tissues and organs, and inhibits them Apoptosis, promote the formation of new blood vessels,improve vascular permeability, manifested in the kidney as sclerosing changes in the glomerular capillaries and microcell structure of the basement membrane disappeared, renal tubulointerstitial scar sclerosis, and finally formed DN [22].Therefore,the abnormal elevation of VEGF level is closely related to the occurrence and development of DN,and it is positively related to the progression of the disease. Therefore,it can be used as an important indicator to evaluate the degree of renal microcirculation disorder and glomerular lesions [23].TGF-β1 is one of the most studied subtypes in the TGF-β series of factors, which can transform the phenotype of normal fibroblasts and has the highest content in the kidney [24].It is considered as the core mediator of renal fibrosis and plays a very important role in DN interstitial fibrosis.Studies have shown that TGF-β1 is involved in multiple links and mechanisms of DN pathogenesis, and is involved in the regulation of multiple signaling pathways in DN pathogenesis, and can be used as an evaluation index and an important therapeutic target for renal fibrosis [25].Studies have shown that[26],the levels of VEGF and TGF-β1 in the serum of patients with early stage DN are significantly higher than those of patients with simple type 2 diabetes. Correlation analysis shows that there is an independent correlation between the two and early stage DN. Evaluation indicators.The results of this research project show that patients with stage DN Ⅲ are given Yiqi Huoxue Decoction on the basis of basic treatment.The serum levels of VEGF and TGF-β1 in patients are significantly lower than those in the control group, suggesting that this recipe can reduce glomerular sclerosis to a certain extent.And delay tubulointerstitial fibrosis and inhibit continued decline in renal function.
In summary, patients with stage DN of Qi and Yin deficiency and stasis type DN given Yiqi Huoxue Decoction on the basis of conventional treatment not only help to lower blood sugar levels, improve TCM syndromes, but also reduce early renal damage and reduce Urinary microalbumin delays further deterioration of renal function and has good safety. The mechanism may be related to reducing the levels of VEGF and TGF-β1,thereby delaying tubulointerstitial scar sclerosis and inhibiting glomerular capillaries. However,the sample size of this study is relatively small,and renal fibrosis-specific indicators are too small. Further in-depth studies are planned in the later stage to further explore the mechanism of this prescription in treating DN.
杂志排行
Journal of Hainan Medical College的其它文章
- Mechanism of Shenfu Decoction in the treatment of critically ill patients with Coronavirus Disease 2019 (COVID-19) based on network pharmacology
- Investigation and analysis of 14 034 college students on COVID-19 and its countermeasures and suggestions
- Effect of Tetrahydroberberine on improving vascular endothelial cell injury
- The relationship between polymorphisms of P-selectin genes and plasma P-selectin concentration with thrombosis in non-valvular atrial fibrillation of Kazakh ethnicity
- Super-minimal incision kidney transplantation: Report of 6 cases
- A meta-analysis of the safety of clopidogrel and tegrarol in patients with non-ST elevation acute coronary syndrome after PCI in China
