Clinical features and prognosis of patients with novel coronavirus pneumonia complicated with diabetes
2020-09-18YeLongJiYangWuYanLengYiZhangAiNingZhangZhongYuanXia
Ye-Long Ji, Yang Wu, Yan Leng, Yi Zhang, Ai-Ning Zhang, Zhong-Yuan Xia
Department of Anesthesiology, Renmin Hospital of Wuhan University, Wuhan, Hubei 430060
Keywords:COVID-19 Diabetes Clinical features Laboratory examination Prognosis
ABSTRACT Objective: To analyze the clinical characteristics and laboratory examinations of patients with new coronavirus (COVID-19) and compare the effect and prognosis of patients with diabetes mellitus (DM) on COVID-19. Methods: 56 cases of COVID-19 with DM and 85 age-matched admitted patients without DM who were admitted to the People's Hospital of Wuhan University from January 31, 2020 to March 15, 2020 were analyzed through a retrospective cohort study. Patients data were collected through electronic cases, and used SPSS 26.0 and Graphpad Prism 8.0 statistical software to compare changes in various indicators of patients in DM and non-DM groups and to draw the survival curves. Results: Compared with the non-DM group, the DM group has a higher percentage of mechanical ventilation, higher mortality and severe patients, with a higher proportion of initial symptoms of nausea and hypertension (P <0.05). There were no significant differences in the gender, initial symptoms (except nausea), the combined underlying diseases (except hypertension) between the two groups (P <0.05); The white blood cell, centroblast count, CRP, PCT, PT, D-dimer, total bilirubin, Urea, LDH, CK, MB, hs-TnI, CK-MB, NT-proBNP were higher in the DM group (P <0.05), and lymphocytes, single Nuclear cell, CD3, CD4, and CD8 counts were low (P <0.05). There was no statistically significant difference in platelet, IL-6, APTT, ALT, AST, Cr and CD19 counts between the two groups. Conclusion: Compared with COVID-19 patients with non-DM, COVID-19 patients with DM have a higher proportion of mortality and severe cases. Heart function, liver and kidney function, immune function damage and coagulation dysfunction are more obvious. Therefore, the monitoring of such patients should be strengthened, and active treatment should be performed to improve the prognosis.
1. Introduction
After the outbreak of severe acute respiratory syndrome coronavirus (SARS-CoV) in the early 21st century, it is difficult to imagine that coronavirus will spread globally again in less than 20 years. In December 2019, multiple cases of unexplained pneumonia occurred in Wuhan City, Hubei Province, with symptoms of fever, dry cough, and dyspnea, similar to the clinical manifestations of SARS-CoV and Middle East Respiratory Syndrome Coronavirus (MERS-CoV) [1].In January 2020, Chinese scientists successfully isolated the virus by deep sequencing of the lower respiratory tract and named it severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and found that it was related to SARS-CoV It belongs to β-coronavirus and is closely related to MERS-CoV (79% homology with SARS-CoV and 50% homology with MERSCoV)[2,3]. On February 11, 2020, the World Health Organization officially named it 2019 Corona Virus Disease (COVID-2019), and confirmed the global pandemic on March 11 of the same year [4,5]. As of May 13, 2020, the number of infected people in the world has exceeded 4 million, and the number of deaths has exceeded 280,000 [6].
The prevalence of diabetes is increasing year by year and is closely related to infection. Previous studies have found that diabetes will increase the prevalence and mortality of pneumonia [7-9]. Therefore, the relationship between diabetes and COVID-19 is not clear. This study retrospectively analyzed the clinical characteristics, laboratory tests and prognosis of 143 patients with COVID-19, aiming to explore the corresponding changes in patients with diabetes (Diabetes Mellitus, DM), and provide evidence for clinical treatment and improving prognosis.
2. Materials and methods
2.1 Clinical data collection
Collected clinical data of 56 patients with DM with COVID-19 and 85 patients with age-matched non-DM with COVID-19 admitted to the Wuhan University People's Hospital from January 31, 2020 to March 15, 2020. This article is a retrospective study, exempting patients from informed consent.
2.2 Selection criteria
All patients were tested positive for novel coronavirus nucleic acid, and clinically classified patients according to the "New Coronavirus Infected Pneumonia Diagnosis and Treatment Program (Trial Version 7)" issued by the National Health Commission of the People's Republic of China[10]:(1)Mild: Mild clinical symptoms, no radiological manifestations of pneumonia. (2) Ordinary type: It has fever, respiratory tract and other symptoms. Pneumonia can be seen on imaging. Severe (any of the following):①Respiratory distress, respiratory rate ≥≥30 times/min;②Finger oxygen saturation ≤≤93% under resting state;③Oxygenation index [arterial blood oxygen partial pressure (PaO2)/oxygen concentration (FiO2)] ≤≤300 mmHg (1 mmHg=0.133 kPa);(3)Critical (one of the following situations):①Respiratory failure requires mechanical ventilation;②Shock;③Combining other organ failures requires intensive care unit (ICU) monitoring and treatment. According to the patient's previous medical history and blood glucose test, the patients were divided into DM group and non-DM group. According to age, COVID-19 patients with DM (M=66, IQR=14.00) and COVID-19 with non-DM (M=66) , IQR=14.00) matches.
2.3 Methods
The required clinical data are obtained through clinical electronic medical records. The clinical data is divided into:(1)General information: gender, age, past history, initial symptoms;(2)Laboratory test results: complete blood count, C-reactive protein (CRP), procalcitonin (PCT), blood coagulation function, serum biochemical test (liver and kidney function), heart function and myocardial enzyme test (four items of myocardial infarction) And immune cell count;(3)Whether to accept mechanical ventilation and prognosis: mechanical ventilation and the number of deaths. And a survival curve was drawn according to the prognosis.
2.4 Statistical methods
SPSS 26.0 and Graphpad Prism 8.0 software were used for statistical analysis and plotting survival curves. The measurement data conforming to the normal distribution are expressed as mean ± standard deviation (±s),The independent sample t test was used for comparison between the two groups; Non-normally distributed measurement data is expressed by the median (quartile) The rank sum test was used for the comparison between the two groups; the count data was expressed as examples (%), and the chi-square test was used for the comparison between the two groups. Kaplan-Meier method was used for survival analysis, univariate analysis was analyzed by Log rank test, and multivariate analysis was performed by Cox regression model test. P<0.05 was considered statistically significant.
3. Results
3.1 Comparison of basic information between two groups of patients
141 confirmed COVID-19 patients were included, including 56 in the DM group and 85 in the age-matched non-DM group. Among them, gender, most of the initial symptoms (fever, dry cough, fatigue or myalgia, abdominal pain or diarrhea, sore throat, sputum and dyspnea), most of the underlying diseases (cardiovascular disease, cerebrovascular disease , Liver and kidney dysfunction bacteria and malignant tumors) were not statistically significant between the two groups (P>0.05);The incidence of nausea symptoms in the DM group, the proportion of patients with hypertension and severe and severe cases were significantly higher than those in the non-DM group (P<0.05), as it showed in table 1.
3.2 Comparison of laboratory test results between two groups of patients
There was no significant difference in platelet count, APTT, ALT, AST, Cr, and CD19 between the two groups at admission (P>0.05); White blood cells, centroblast count, CRP, PCT, PT, D-dimer, total bilirubin, Urea, LDH, CK, Mb, CK-MB, hs-TnI, NT-proBNP were significantly higher in the DM group compared with non-DM. The counts of lymphocytes, monocytes, CD3, CD4, and CD8 in the non-DM group were significantly higher than those in the DM group (P<0.05), as is shown in table 2.
3.3 Prognosis of two groups of patients
The proportion of mechanical ventilation and mortality in the DM group were significantly higher than those in the non-DM group (P<0.05); The survival curve also showed that the mortality rate of the DM group was significantly greater than that of the non-DM group (P<0.05), as is shown in Table 3 and Figure 1.

Table 1 Basic information of patients on admission
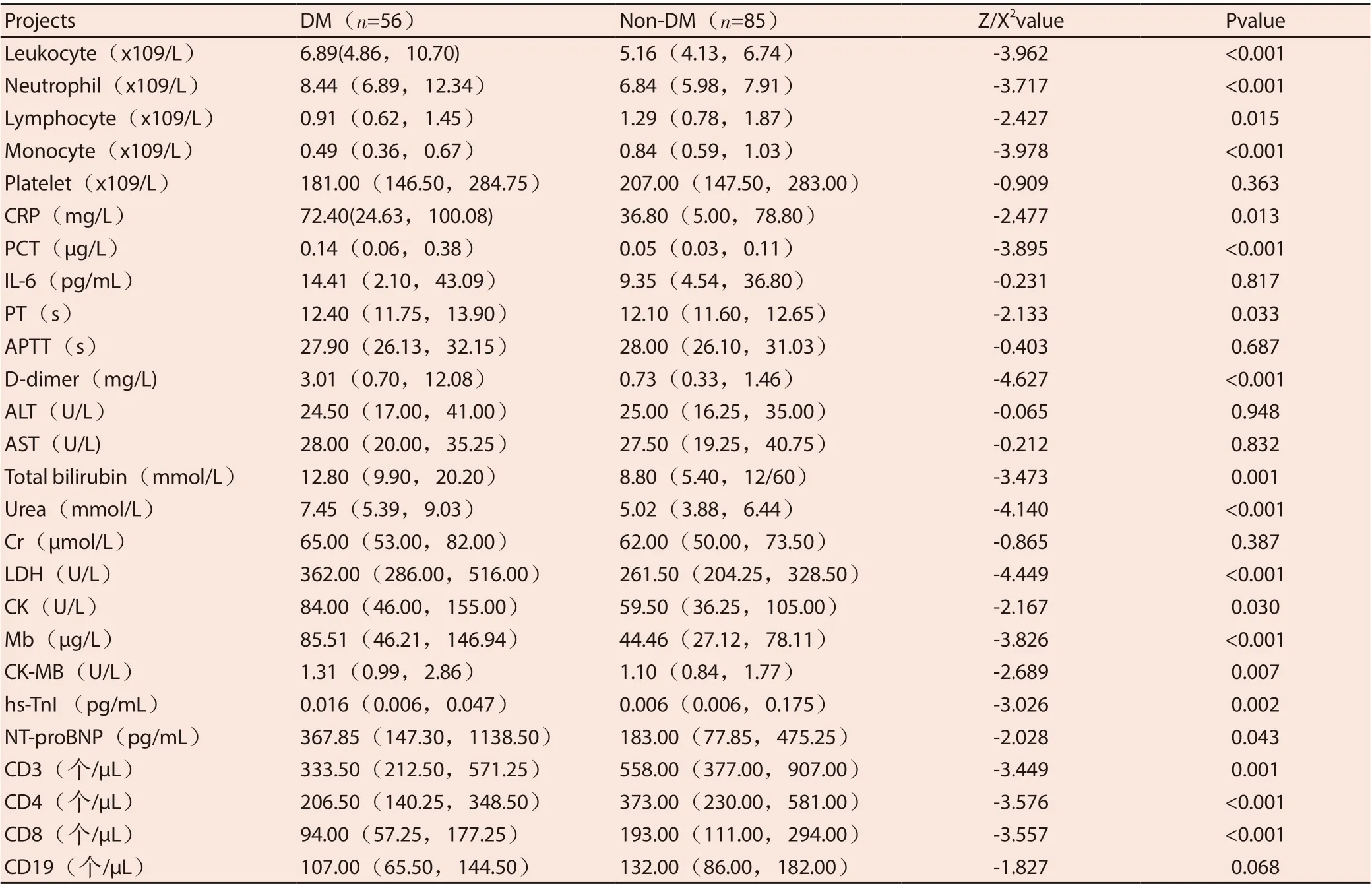
Table 2 Indexes of laboratory tests of patients upon admission [M (Q1, Q3)]
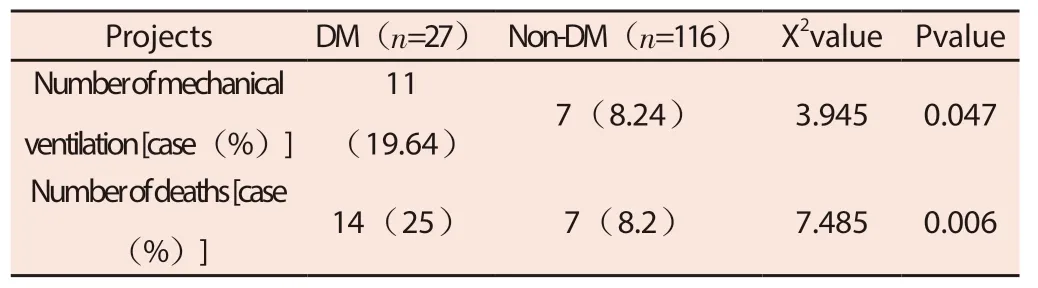
Table 3 Prognosis of two groups of patients
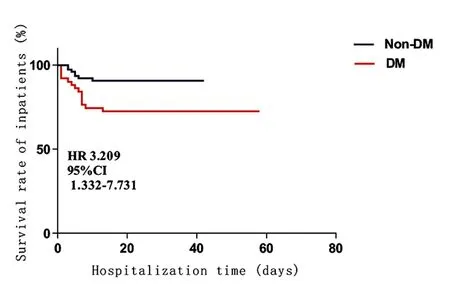
Figure 1 Comparison of survival curves of two groups of patient
4. Discussion
The People's Hospital of Wuhan University, as a designated medical unit for COVID-19 in Wuhan, diagnoses and treats a large number of COVID-19 patients. This study analyzed 56 patients with COVID combined with DM and 85 age-matched patients with COVID without combined DM through a retrospective cohort study, and found:(1)Most patients with COVID combined with DM are severely ill, and they are often accompanied by hypertension (P<0.05);(2)Inflammatory reaction of these patients is more significant, accompanied by a decrease in immune function, and the damage of heart, liver and kidney function is aggravated (P<0.05);(3)Although there is no statistically significant difference between these patients and patients with COVID-19 without DM in combination with cardiovascular disease (P>0.05), but the ratio shows a large change, and COVID-19 with DM patients with mechanical ventilation The proportion and mortality rate are higher (P<0.05), indicating that these patients have poor prognosis and vital signs still need to pay close attention and give corresponding treatment measures to improve their prognosis.
The results of this experiment showed that patients with DMcoated COVID-19 had increased white blood cell counts, central granulocyte count, CRP, and PCT, and decreased lymphocyte, central granulocyte count, CD3, CD4, and CD8 counts, suggesting that the inflammatory response was higher than that of non-DM combined COVID. -19 patients are more significant, and the immune system is greatly suppressed;Although ALT, AST and Cr had no statistical difference between COVID-19 with DM and COVID-19 with non-DM, but Urea, total bilirubin, PT, D-dimer of COVID-19 with DM Significantly increased body level, suggesting that liver and kidney function and blood coagulation function are aggravated; CK, Mb, CK-MB, hs-TnI, NT-proBNP were significantly increased in COVID-19 patients with DM, suggesting increased cardiac function damage.Yan et al.[11] analyzed the clinical data of 193 severe or critical COVID-19 patients and found that the inflammatory response of patients with DM was more severe, and the heart function, liver and kidney function and blood coagulation function were significantly abnormal. Meta analysis by Wang et al.[12] also showed that hypertension, DM, chronic obstructive pulmonary disease, cardiovascular disease, and cerebrovascular disease are independent risk factors for COVID-19 patients. At the same time, this study found that a higher proportion of COVID-19 patients with DM combined with hypertension, indicating that in addition to DM is its independent risk factor, such patients may have hypertension pathology, which aggravates the damage of COVID-19; Although there is no statistical difference between COVID-19 patients with DM and non-DM COVID-19 patients with cardiovascular disease, the proportion is high and DM patients are more susceptible to cardiovascular damage, so such patients may have The pathology of vascular disease has aggravated the damage of COVID-19 [13].
Angiotensin-converting enzyme 2 (ACE2) is a key protein that can maintain normal cardiovascular and renal function by regulating the renin-angiotensin system [14]. The study found that the invasion ability of SARS-CoV-2 mainly enters the host cell through the Spike protein in its structural protein and ACE2 as a receptor [15,16]. At the same time, ACE2 is widely expressed in the respiratory tract, kidney, intestine, immune cells, pancreas, arteries and vein endothelium, which may also explain the origin of the main clinical symptoms of COVID-19 [17]. Since angiotensin-converting enzyme inhibitors and angiotensin receptor blockers are widely used in the treatment of DM, and hypoglycemic drugs such as pioglitazone and liraglutide are also associated with the upregulation of ACE2, it may be that DM aggravates COVID One of the reasons for COVID-19 [18]. However, studies have found that ACE2 can also reduce inflammation and antioxidants, and has been suggested as a potential treatment for inflammatory diseases such as lung disease, cancer, diabetes, and hypertension [19];At the same time, ACE2 also protects the lungs from acute respiratory distress syndrome and resists H5N1 avian influenza infection [20].A The physiological diversity of CE2 may result in differences in the sensitivity of individuals to ACE2. Therefore, ACE2 should be further studied to control its regulation and provide new directions for the prevention and treatment of COVID-19.
Cytokine release syndrome or cytokine storm refers to a systemic inflammatory response guided by infection, drugs or other factors, which is characterized by proinflammatory cytokines (interleukin-6, interleukin-18, interference) in peripheral blood Hormone, tumor necrosis factor, etc.) levels rise sharply [21]. The study found that the generation of cytokine storms in patients with COVID-19 can cause ARDS and multiple organ dysfunction outside the lung, and is an important factor for COVID-19 deterioration and even death [22]. The results of this experiment found that although interleukin-6 did not have a statistical difference between patients with DM combined with COVID-19 and non-DM combined COVID-19, but the difference in peripheral blood levels was huge, the reason may be the sample size partly missing. At the same time, abnormal levels of ACE2 will also lead to dysfunction of the renin-angiotensin system, enhance inflammation and vascular permeability, and the Spike protein of coronavirus will induce the shedding of ACE2 and promote some proinflammatory cytokines (tumor necrosis Factor) [23,24]. Another feature of DM is that it can also trigger excessive proinflammatory cytokine release when the immune response is low [25]. The above reasons may be the reason that patients with DM combined with COVID-19 are more prone to cytokine storm and aggravate the injury than those with non-DM COVID-19. Because some hypoglycemic drugs (glucagon-like peptide 1 receptor agonist, pioglitazone) also show an effect on inflammation, and human dipeptidyl peptidase 4 is also associated with the development of coronavirus inflammation and is associated with insulin reduction and resistance [26-28]. Therefore, the rational application of different treatment methods will also bring better efficacy to COVID-19 patients with DM.
In summary, this study found that COVID-19 patients with DM have a higher mortality rate, more severe and critical illnesses, and greater heart function, liver and kidney function than non-DM COVID-19 patients. The mechanism of coagulation damage may be related to the increase of ACE2 and the generation of inflammatory factor storm. Regarding the treatment method, in the active treatment of the symptoms of COVID-19, the selection of suitable blood glucose lowering drugs and blood purification of inflammatory factors may help to improve the prognosis of COVID-19 patients with DM.
Conflict of interest
All authors have no conflicts of interest
杂志排行
Journal of Hainan Medical College的其它文章
- Mechanism of Shenfu Decoction in the treatment of critically ill patients with Coronavirus Disease 2019 (COVID-19) based on network pharmacology
- Investigation and analysis of 14 034 college students on COVID-19 and its countermeasures and suggestions
- Effect of Tetrahydroberberine on improving vascular endothelial cell injury
- The relationship between polymorphisms of P-selectin genes and plasma P-selectin concentration with thrombosis in non-valvular atrial fibrillation of Kazakh ethnicity
- Super-minimal incision kidney transplantation: Report of 6 cases
- A meta-analysis of the safety of clopidogrel and tegrarol in patients with non-ST elevation acute coronary syndrome after PCI in China
