多层螺旋CT在急性脂垂炎的临床价值
2020-09-15李大鹏夏顺明徐萍熊中奎张小胜
李大鹏 夏顺明 徐萍 熊中奎 张小胜
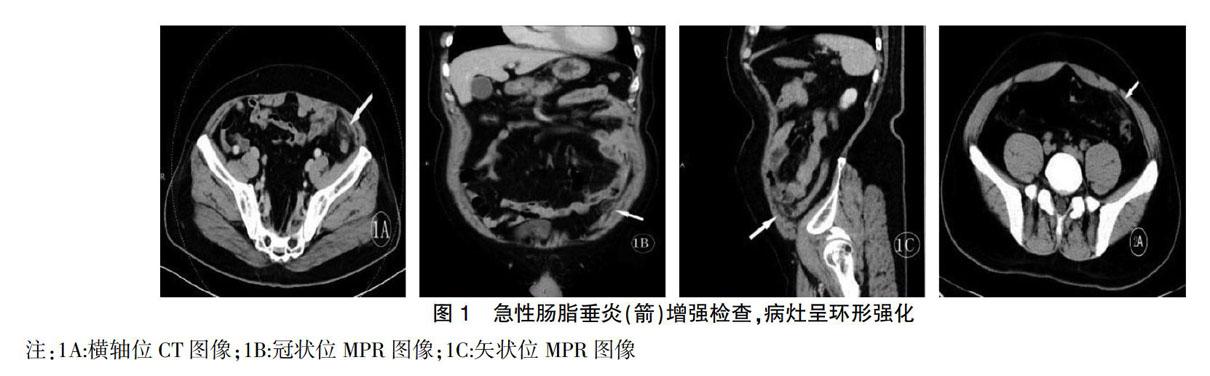


[摘要] 目的 探討多层螺旋CT(MSCT)在急性肠脂垂炎(Acute epiploic appendagitis,AEA)的临床诊断价值及对该病发病机制的探索。 方法 收集本院2014年7月~2018年12月急性肠脂垂炎患者资料22例,完善相关的人体学指标,并按照中国成年人体质指数分为4组(轻体重、健康体重、超重、肥胖),所有患者行中下腹CT扫描,观察病灶的部位、形态、密度、大小、边缘及邻近脂肪组织等表现。 结果 本组22例患者病灶均位于结肠前外侧壁,9例位于盲肠,7例位于乙状结肠与降结肠交界处,4例位于降结肠,1例位于乙状结肠,1例位于结肠肝曲,所有病例均表现为典型的“环征”,中央卵圆形脂肪密度,边缘环形软组织密度,周围脂肪密度增高;通过临床资料分析,本病好发于青壮年,男性多于女性,随着BMI指数增加,发病率有上升趋势。 结论 急性肠脂垂炎在MSCT上表现为典型的“环征”,结合相关的临床资料,如年龄、性别、体重,能够达到方便、快捷的诊断。
[关键词] 急性肠脂垂炎;多平面重建;CT;腹部
[中图分类号] R57;R5 [文献标识码] B [文章编号] 1673-9701(2020)21-0131-04
Clinical value of multi-slice spiral computed tomography (CT) in acute lipositis
LI Dapeng1 XIA Shunming1 XU Ping1 XIONG Zhongkui2 ZHANG Xiaosheng3
1.Imaging Department, the Second Affiliated Hospital of Nanjing Medical University, Nanjing 210028, China; 2.Radiotherapy Department, Shaoxing Second Hospital in Zhejiang Province, Shaoxing 312000, China; 3.Radiology Department, Jiangsu Province Hospital on Integration of Chinese and Western Medicine, Nanjing 210028, China
[Abstract] Objective To investigate the clinical diagnostic value of multi-slice spiral CT(MSCT) in acute epiploic appendagitis(AEA) and explore the pathogenesis of the disease. Methods The data of 22 patients with AEA from July 2014 to December 2018 in our hospital were collected to improve relevant anthropometric indexes. According to the body mass index(BMI) of Chinese adults, the patients were divided into 4 groups(lightweight, healthy weight, overweight, obesity). All patients underwent CT scans of the lower and middle abdomen to observe the location, shape, density, size, edge and adjacent adipose tissue of the lesions. Results The focus of 22 patients in this group was located in the anterior lateral wall of the colon, 9 cases in cecum, 7 cases at the junction of sigmoid colon and descending colon, 4 cases in descending colon, 1 case in sigmoid colon and 1 case in hepatic flexure of the colon. All cases showed typical ‘ring sign, with central oval fat density, marginal annular soft tissue density and increased peripheral fat density. According to the analysis of clinical data, the disease was more frequent in young adults and more common in men than in women. With the increase in BMI, the incidence rate had an upward trend. Conclusion AEA is a typical ‘ring sign on MSCT. Combined with relevant clinical data, such as age, sex and weight, it achieves convenient and rapid diagnosis.
3.2 急性肠脂垂炎(AEA)的CT表现
正常脂肪垂因其密度与周围肠系膜组织相同,CT扫描难以发现,只有在发生炎症或有腹水环绕时才能在CT图像上显示[8]。急性肠脂垂炎(AEA)CT表现为直径小于5 cm(典型0.8~2.7 cm)的卵圆形脂肪密度团块,中间密度较低,CT值在-40~-75 HU之间,边缘密度较高,为坏死组织,即形成“环征”,增强后常呈环形强化,邻近周围脂肪间隙模糊,密度增高,呈火焰样,为周围炎性病变;局部腹膜组织可因充血水肿或继发感染渗出而发生增厚,相邻结肠壁可稍增厚。Ergelen Rabia等[9]报道有54%的患者,病灶中央见线状高密度,这一征象可能为血栓形成或纤维隔膜。Giannis Dimitrios等[10]认为经常还可见到“中心点征”,即卵圆形病灶中间见点片状或线条状稍高密度影,为坏死、中央动静脉充盈缺损或血栓形成,同时研究还发现,高密度环可出现在肠脂垂炎的所有病例中,仅有42.9%的病例病灶中央出现线状或点状高密度影,也就是说没有点、线状高密度影也不能排除肠脂垂炎的诊断。本组22例CT表现均为结肠前缘卵圆形脂肪密度影,边缘高密度,周围可见渗出影,也就是“环征”,“环征”是典型的影像学表现,对于诊断急性肠脂垂炎有非常重要的价值,本组22例中未出现文献描述的病灶中央线样高密度征象及“中心点征”的表现,笔者认为可能是样本量小的原因。
3.3 急性肠脂垂炎(AEA)的鉴别诊断
3.3.1 急性阑尾炎 急性阑尾炎是临床上常见的急腹症,临床表现为转移性右下腹痛,右下腹麦氏点压痛,反跳痛等,部分患者可以出现恶心、呕吐等胃肠道症状及发热、白细胞升高,CT表现为阑尾直径增粗(>6 mm),主要由于阑尾腔内积液扩张,壁增厚(>2 mm),周围包绕阑尾的脂肪间隙呈片絮状密度增高,阑尾腔内经常可见粪石影,原因是粪石嵌顿阻塞而引起阑尾积液扩张,尤其是青少年患者[11],与急性肠脂垂炎的鉴别诊断非常重要,因两者治疗方案截然不同,所以对于临床上怀疑急性阑尾炎的患者,术前进行多层螺旋CT检查是很有必要的。本组实验中有2例临床以急性阑尾炎拟行手术治疗收住院,经CT检查后诊断为急性肠脂垂炎,因此在临床上要格外细心加以鉴别,避免给患者带来不必要的手术损伤。
3.3.2 网膜梗死 极似急性肠脂垂炎,常有持续几天的腹痛临床特点,多数局限在右上或下腹,15%发生于儿童,因为其有大量的侧支循环,很少引起小肠或大肠梗死,CT表现为单个较大不同密度的网膜肿块,没有强化,多无连续的高密度环,常大于5 cm,靠近但不接触结肠和盲肠[12]。
3.3.3 急性憩室炎 年龄较急性肠脂垂炎更大些,常有恶心、呕吐、发热、WBC增高和反跳痛,多有弥漫性下腹痛;CT表现结肠憩室囊袋样突出,周围可见片絮状渗出及索条影,邻近结肠壁可水肿增厚,也可发生穿孔而出现肠外积气或积液,甚至系膜脓肿或结肠外脓肿形成[13]。急性憩室炎感染可引起继发性肠脂垂炎,增加了CT诊断的难度、肠管外积气,长节段的增厚的结肠壁不是急性肠脂垂炎的CT征象,而是急性憩室炎的征象[14]。
3.3.4 硬化性肠系膜脂膜炎 好发于60~70岁,男性多见,有腹痛、发热、恶心、呕吐、腹泻、体重减轻等症状,多数患者有自愈性并且预后良好[15],其主要征象包括雾状肠系膜征、脂肪环征、肿块假包膜、软组织小结节及囊性变5种征象[16]。硬化性肠系膜炎,病灶大,多数起源于小肠系膜,不临近结肠壁;而肠脂垂炎7病灶小,邻近结肠,不累及小肠系膜。另外硬化性肠系膜脂膜炎尤其是退缩性肠系膜炎还需要和肿瘤相鉴别。
总之,随着人们生活的日益提高,超体重及肥胖的人群增加,在日常临床工作中发现,急性肠脂垂炎发病率有上升的趋势,所以影像科医生必须掌握急性肠脂垂炎的CT表现并结合相关的临床资料,如年龄、性别、体重,方便、快捷、精准的诊断该病并不困难,从而避免了滥用抗生素及不必要的手术治疗。
[参考文献]
[1] Seo,JW. Acute epiploic appendagitis of the vermiform appendix:Typical computed tomographic image with pathologic correlation[J]. Advances in Computed Tomography,2017,6(4),21-27.
[2] 楊海鸥,韩丽萍,林丽红,等. 原发性肠脂垂炎的MSCT特征表现[J]. 中国CT和MRI杂志,2018,16(2):38-40.
[3] 翟建春,石安斌,杨秋云,等. 肠系膜脂膜炎的临床症状、CT影像特点及病理分析[J].中国CT和MRI杂志,2017,15(3):115-117.
[4] 吴志涛. 原发性肠脂垂炎的CT诊断及临床治疗研究[J].实用医学影像杂志,2019,20(1):70-72.
[5] Almuhanna AF,Alghamdi ZM,Alshammari E. Acute epiploic appendagitis:A rare cause of acute abdomen and a diagnostic dilemma[J]. J Fam Community Med,2016, 23(1):48-50.
[6] 陈茂豪,梁彩妮,陈晓龙,等. 多排螺旋CT诊断原发性肠脂垂炎的临床价值分析[J]. 医学影像学杂志,2017, 27(6):1193-1195.
[7] Elizabeth A Chu,Evan Kaminer. Epiploic appendagitis:A rare cause of acute abdomen[J]. Radiology Case Reports,2018,13(3):599-601.
[8] 蔡顺达,吴湘萍. 原发性肠脂垂炎多排螺旋CT检查特征及临床价值[J]. 临床医药文献电子杂志,2018,5(86):1-2.
[9] Ergelen Rabia,Asadov Ruslan,zdemir Burcu,et al. Computed tomography findings of primary epiploic appendagitis as an easily misdiagnosed entity:Case series and review of literature[J]. Ulusal Travma Ve Acil Cerrahi Dergisi=Turkish Journal of Trauma & Emergency Surgery:TJTES,2017,23(6):489-494.
[10] Giannis Dimitrios,Matenoglou Evangelia,Sidiropoulou Maria S,et al. Epiploic appendagitis: pathogenesis,Clinical findings and imaging clues of a misdiagnosed mimicker[J]. Annals of Translational Medicine,2019,7(24):814-821.
[11] 楊家辉,毛巨江,崔冬冰,等. 多层螺旋CT对急性阑尾炎及其并发症的诊断价值[J].贵州医科大学学报,2017,42(11):1349-1352.
[12] McCusker R,Gent R,Goh DW. Diagnosis and management of omental infarction in children:Our 10 year experience with ultrasound[J]. Journal of Pediatric Surgery,2018,53(7):1360-1364.
[13] 朱新影,赵文娟,杜娟,等. 急性结肠憩室炎132例临床特点分析[J]. 中国内镜杂志,2019,25(7):30-33.
[14] Choi Youn I,Woo Hyun Sun,Chung Jun-Won,et al. Primary epiploic appendagitis: Compared with diverticulitis and focused on obesity and recurrence[J]. Intestinal Research,2019,17(4):554-560.
[15] 蒋青伟,王凤丹,王文泽,等. 肠系膜脂膜炎12例临床特征分析[J]. 中华内科杂志,2017,56(2):112-115.
[16] 王礼同,蔡玉建. 肠系膜脂膜炎的多排螺旋CT检查影像学特征[J]. 中华消化外科杂志,2017,16(6):624-628.
(收稿日期:2020-05-08)
