Mutational analysis of Ras hotspots in patients with urothelial carcinoma of the bladder
2020-09-14
Kiran Tripathi,Minal Garg,Department of Biochemistry,University of Lucknow,Lucknow 226007,India
Apul Goel,Department of Urology,King George Medical University,Lucknow 226003,India
Atin Singhai,Department of Pathology,King George Medical University,Lucknow 226003,India
Abstract
Key words:Coding exons;Oncogenic activation;Polymerase chain reaction - restriction fragment length polymorphism;Point mutations;Ras genes;Urothelial carcinoma of bladder
INTRODUCTION
Urinary bladder cancer is the second most common genitourinary cancer globally and its occurrence has very high gender variability (http://cancerindia.org.in/globocan-2018-india-factsheet/).It is the sixth most common cancer in men and the seventeenth most common cancer in women.The etiology of bladder cancer is very complex.Among many factors,tobacco chewing/smoking and environmental or occupational exposure to a number of carcinogens have been identified as the most important risk factors for bladder cancer[1-3].
Urothelial carcinoma of the bladder (UCB) originates in the cells of the innermost layer of bladder urothelium and accounts for approximately 90% of all bladder cancers.Clinically,two distinct forms of UCB namely,non-muscle invasive bladder cancer (NMIBC in 75%-80% of patients) and muscle invasive bladder cancer (MIBC in 20%-25% of patients) develop along papillary and non-papillary pathways[4].Patients diagnosed with NMIBC can be successfully treated.Nevertheless,these tumors have a higher tendency to recur (50% to 90%) and 15% progress to invasive and metastatic tumors.Morbidity and mortality are associated with the high grade,non-papillary,muscle invasive form of the disease.Molecular studies to characterize the genotypic differences in the pathogenesis of NMIBC and MIBC may improve the diagnostic/prognostic outcome of the disease.
Rat sarcoma viral oncogene homolog (Ras) belongs to the family of small G proteins with intrinsic GTPase activity that governs various cellular signal transduction pathways.Alterations in the expression or functions of (Ras) genes caused by various point mutations within the gene have been established as prognostic factors in the genesis of a constitutively active RAS-mitogen activated protein kinase pathway that leads to cancer.Point mutations within the hotspot regions ofRasgene lead to reduced intrinsic GTPase activity,the protein is locked into a constitutively active state and results in aberrant cell signaling even in the absence of external signals[5].In vitroandin vivostudies on tumor regression upon withdrawal ofRasexpression indicate that mutantRasis a therapeutically useful drug target even in advanced metastasis[6].MutantRasgene has been shown to be associated with drug resistance,enhanced metastasis,poor prognosis and shorter survival of patients[7].
Approximately 30% of human cancers are known to harbor genomic mutations in the three functional isoforms of Ras genes (H-Ras;located at 11p15.5;K-Ras;located at 12p12.1;andN-Ras;located at 1p13.2).The most common mutational hotspots in the codons for amino acid residues 12,13 or 61 are confined to exon 1 or 2 ofH-Ras(G12V,G12S,G12A,G12D,G13D,Q61R);K-Ras(G12D,G12S,G12R,G12A,G12V,G12C,G13D);andN-Ras(G12D,Q61N,Q61L,Q61K).Tissue and organ specificities ofRasgene activation have been reported to vary with mutated codon and type ofRasgene isoform.K-Rasmutations occur frequently in non-small cell lung,colorectal,and pancreatic carcinomas;H-Rasmutations are common in bladder,kidney,and thyroid carcinomas;whileN-Rasmutations have been identified in melanoma,hepatocellular carcinoma,and hematologic malignancies[8,9].
Published studies provide conflicting results regarding the frequency distribution ofRasmutational spectrum in UCB patients[10-14].Out of a total of 11.67% mutations in exon 1 ofK-Ras,maximum mutations were reported at codon 12 in bladder cancer patients[15].Iranian patients with bladder cancer did not exhibit any mutation in the hotspot codons (12,13,and 61)[16].Various studies have examined 45%,46.7% and 39%ofH-Rasmutations in codon 12 in bladder cancer patients[17-19].Due to the reported heterogeneity in the distribution of the most frequent mutations inRasisoforms in bladder cancer specimens,it is necessary to examine the presence/absence of mutations in order to predict disease outcome[10,11].
Speculating the role of mutantRasin bladder tumorigenesis,the present study has been conducted to determine its clinical impact by examining the relationship between clinical histopathological variables in UCB patients and the mutational spectrum.Frequency distribution and prevalence of mutations in the hotspot regions ofH-Rascodon 12 (glycine to valine/serine/alanine/aspartic acid),K-Rascodon 12 (glycine to valine/aspartic acid/serine/arginine/alanine/cysteine),K-Rascodon 13 (glycine to aspartic acid) andN-Rascodon 61 (glutamine to lysine/arginine) were examined by polymerase chain reaction - restriction fragment length polymorphism (PCR-RFLP) in a cohort of 87 North Indian UCB patients and 23 controls with normal bladder mucosa.The results were confirmed by direct DNA sequencing of coding exons 1 and 2 ofH-Ras,K-RasandN-Rasgenes.
MATERIALS AND METHODS
Patients and controls
Patients were enrolled in the Urology OPD at King George’s Medical University(KGMU),Lucknow during 2018-2019.All 87 patients examined had symptoms of hematuria as a major sign followed by urinary frequency or irritative symptoms and were assessed for primary tumor.Patients underwent bimanual examination under anesthesia before and after endoscopic surgery (biopsy or transurethral resection) or histological verification of the absence or presence of tumor.Imaging of the chest,abdominal ultrasound and computed tomography of the abdomen (whenever required) were performed to detect common metastatic sites as well as lymph node involvement.Tumor tissues from 42 NMIBC (stage pTa-pT1) and 45 MIBC (stage pT2-pT4) were obtained after transurethral resection of the bladder tumor.Tissues were collected in RNAlater,snap frozen and stored at -80°C for future use.Clinical data on the UCB patients and pathological classification/records based on pathological TNM staging were provided by the Department of Urology and Department of Pathology,KGMU,Lucknow.After informed consent,normal bladder mucosal tissues were collected from 23 benign prostate hyperplasia (BPH) patients during cold cup biopsy.These patients underwent transurethral resection of the prostate for BPH and had known bladder lesions.Pathologists independently diagnosed and classified bladder tumors according to World Health Organization and International Society of Urologic Pathology 2004 classification system[20].Ethical clearance was obtained from Bioethics Cell,Institutional Ethics Committee,KGMU (reference no.89thECM II A/P8).
DNA extraction
Genomic DNA was extracted from 87 UCB and 23 control bladder mucosal tissues using proteinase K and phenol-chloroform extraction,followed by ethanol precipitation,and was quantified and then stored at -20°C.
PCR-RFLP
PCR was performed to amplify DNA segments which span (1) codon 12 ofH-Rasgene;(2) codon 12 and codon 13 ofK-Rasgene;and (3) codon 61 ofN-Rasgene in 87 UCB and 23 bladder mucosal tissues.The primer sequences used are listed in Table 1.
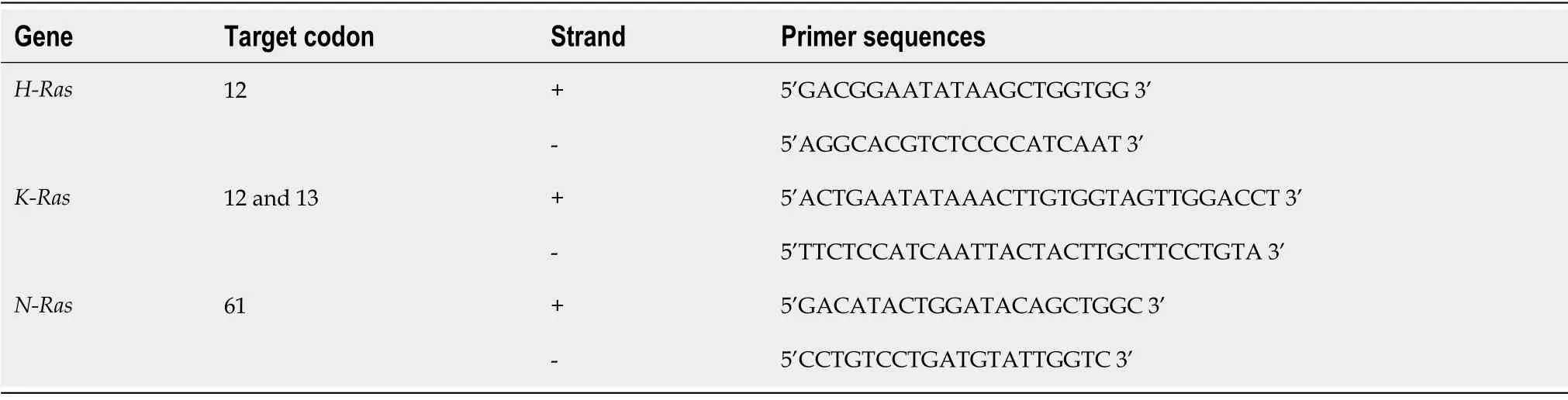
Table1 Primer sequences used for polymerase chain reaction - restriction fragment length polymorphism
PCR was carried out with 200 ng of DNA,10 pmol of primer(s),and Emerald Amp max PCR master mix (TaKaRa,Clontech) using a thermal cycler (T100TM,BioRad,United States).Cycling conditions included initial denaturation at 98°C for 20 s,followed by 30 cycles of [denaturation:98°C for 10 s,annealing:60°C (forH-RasandN-Ras) and 58°C forK-Rasfor 30 s,and extension:72°C for 30 s] followed by a final extension at 72°C for 5 min.
Restriction endonucleases MspI (Thermo Scientific),BstNI (Thermo Scientific),HphI(Thermo Scientific),and MScI (Thermo Scientific) were used to digest amplified PCR fragments containing codon 12 ofH-Ras,codon 12 ofK-Ras,codon 13 ofK-Ras,and codon 61 ofN-Ras,respectively.Buffers and incubation conditions (37°C for 1-16 h)were used according to the manufacturers’ recommendations.The digested and undigested fragments were subjected to electrophoresis on 3% agarose gel.A summary of theRasgene assays is described in Table 2.
Direct DNA sequencing
Coding exons 1 and 2 each ofH-Ras,N-RasandK-Raswere amplified by the laboratory developed primer pairs (Table 3).Primers were designed for the GenBank reference sequence ofH-Ras,N-RasandK-Ras(accession numbers:NM_001130442.1.1,NM_004985.4.1,NM_002524.4.1,respectively) by Primer plus software.The 200 ng of DNA was amplified with 10 pmol primer using the Phusion high-fidelity PCR kit(Thermo Scientific).The thermal profile included initial denaturation at 98°C for 40 s,followed by 35 cycles of (1)H-Ras:[denaturation:98°C for 5 s,annealing:63.2°C (for exon 1) and 64.8°C (for exon 2) for 10 s,and extension:72°C for 15 s];(2)N-Ras:[denaturation:98°C for 5 s,annealing:62.1°C (for exon 1) and 61.4°C (for exon 2) for 10 s,and extension:72°C for 15 s];(3)K-Ras:[denaturation:98°C for 5 s,annealing:61.8°C(for exon 1) and 61.3°C (for exon 2) for 10 s,and extension:72°C for 15 s];followed by a final extension at 72°C for 7 min.Amplified PCR products were electrophoresed on 2% agarose gel,eluted and purified with a QIAquick®PCR purification kit (Qiagen,Hilden,Germany) according to the manufacturer’s instructions.Sequencing reactions were performed for both the DNA strands by the BigDye™ Terminator v1.1 Cycle Sequencing Ready Reaction Kit version 3.1 (Applied Biosystems,Monza,Italy) on a total of 10 ng of purified PCR products.Sequence analysis was performed using a 3500 Genetic Analyzer.The files/electropherogram obtained were analyzed by seq scap_v5.2 software.Sequence results of bladder mucosa were aligned with the reference sequences (mentioned above) using Blastn.Furthermore,DNA sequences of the respective regions in bladder tumor specimens were compared with that of wildtype sequences to examine the presence/absence of mutations in the coding exons 1 and 2 of theH-Ras,N-RasandK-Rasgenes.
RESULTS
Clinical histopathological summary of patients
The mean age of the patients included in the study was 58.3 years (range:25-83 years)and 44 (50.17%) patients were older than 60 years.The male to female ratio was 11:1.Of 87 patients,66 (75.86%) had a positive history of either smoking or a tobacco chewing habit.Twenty of 87 tumors (22.98%) were more than 3 cm in size,whereas 67 tumors (77.01%) were less than 3 cm.Pathologically,42/87 (48.27%) tumors wereclassified as NMIBC and 45/87 (51.72%) as MIBC.According to the histopathological classification,80.95% (34/42) non-muscle invasive tumors were of low grade and 19.04% (8/42) were of high grade.All MIBC patients had a high grade tumor.Of 87 tumors,26/87 (29.88%) were recurrent type,while the remaining 61/87 (70.11%) were identified as primary tumors (Table 4).

Table2 Summary of Ras gene assays
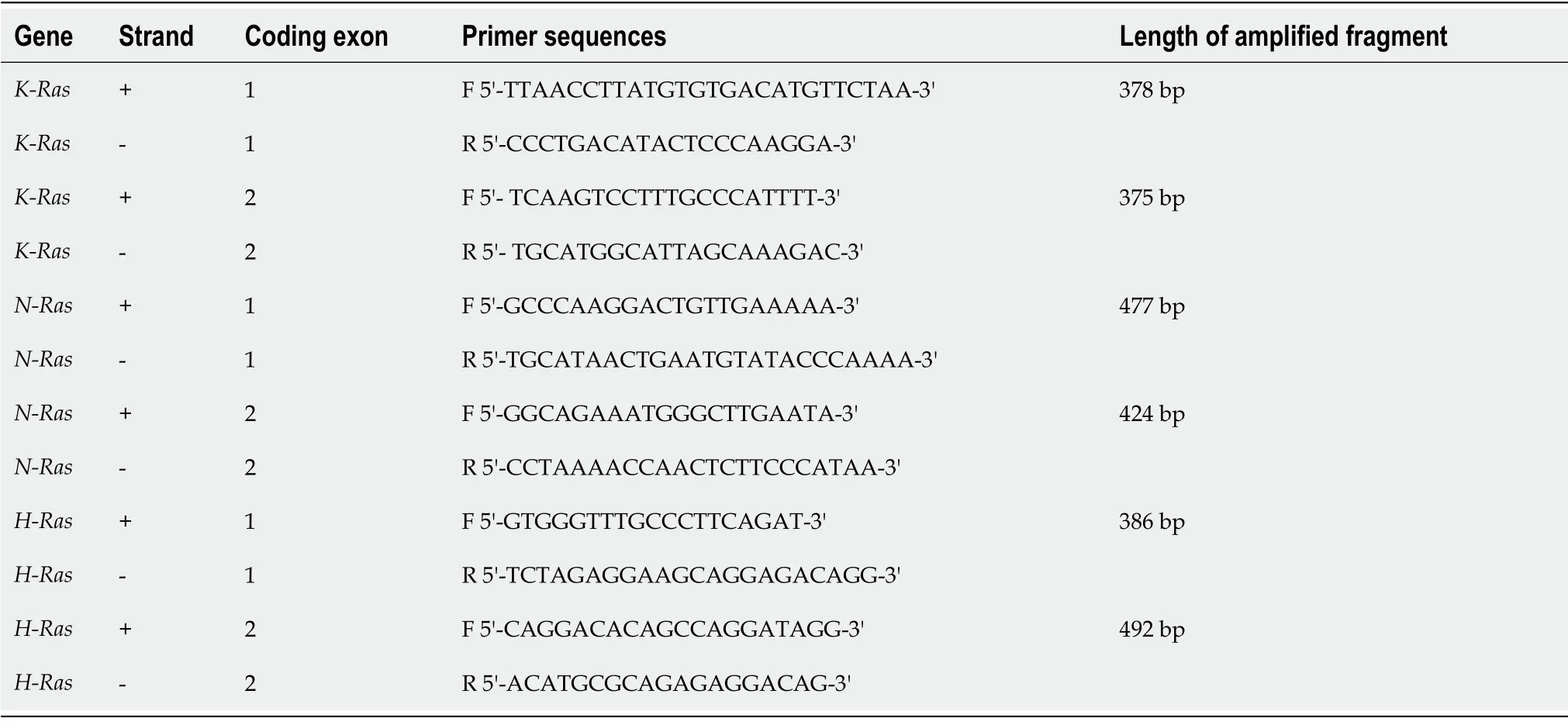
Table3 Primer sequences used in direct DNA Sequencing
Point mutation detection in H-Ras
PCR-RFLP was carried out to examine the point mutation in codon 12 ofH-Rasgene in 87 bladder tumor tissues and 23 normal bladder mucosal tissues.Digestion of the wild-type amplicon of 420 bp by MspI gave rise to two bands of 390 bp and 30 bp.The presence of a point mutation at codon 12 results in loss or modification of the endonuclease recognition site which is indicative of the translational change of glycine(GGC) to serine (AGC)/valine (GTC)/alanine (GCC)/aspartic acid (GAC).In our study,none of the tumors were examined for the presence of point mutation at codon 12 ofH-Rasgene (Figure 1A).

Table4 Clinicohistopathological profile of patients with urothelial carcinoma of bladder
Direct DNA sequencing of the coding exonic region 1 spanning the codons 12,13 and exon 2 containing hotspot codon 61 ofH-Rasgene was performed.Blastn results of DNA sequences in all the tumor specimens showed 100% alignment with that of the wild-type.Electropherogram analysis did not identify the presence of any point mutations in exons 1 and 2 ofH-Rasgenes in the tumor specimens (Figure 1B and C).
Point mutation detection in N-Ras
Tumor specimens from 87 UCB patients and 23 normal bladder mucosal tissues were examined by PCR-RFLP for the presence or absence of specific point mutations at codon 61.The presence of a point mutation at codon 61 may result in the conversion of glutamine (CAA) to lysine (AAA)/arginine (CGA)/leucine (CTA).The proper restriction site (TGG↓CCA)was created by changing only one nucleotide in a forward primer just before the start of codon 61.Restriction digestion of the wild-type amplicon of 65 bp by enzyme MscI resulted in its cleavage into 21 bp and 44 bp(Figure 2A).The present study failed to detect the presence of point mutations in 87 UCB and 23 normal mucosal specimens.
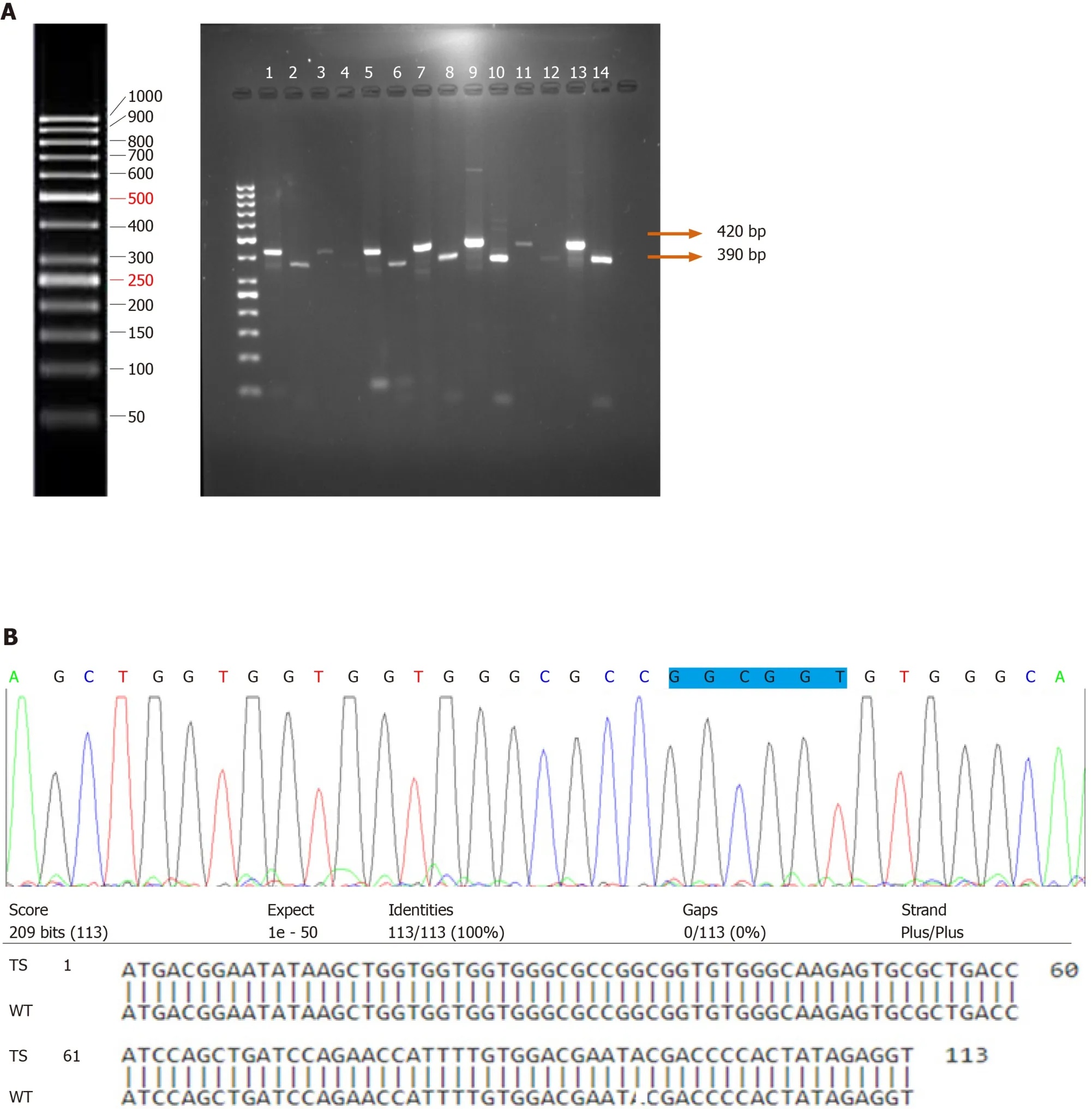
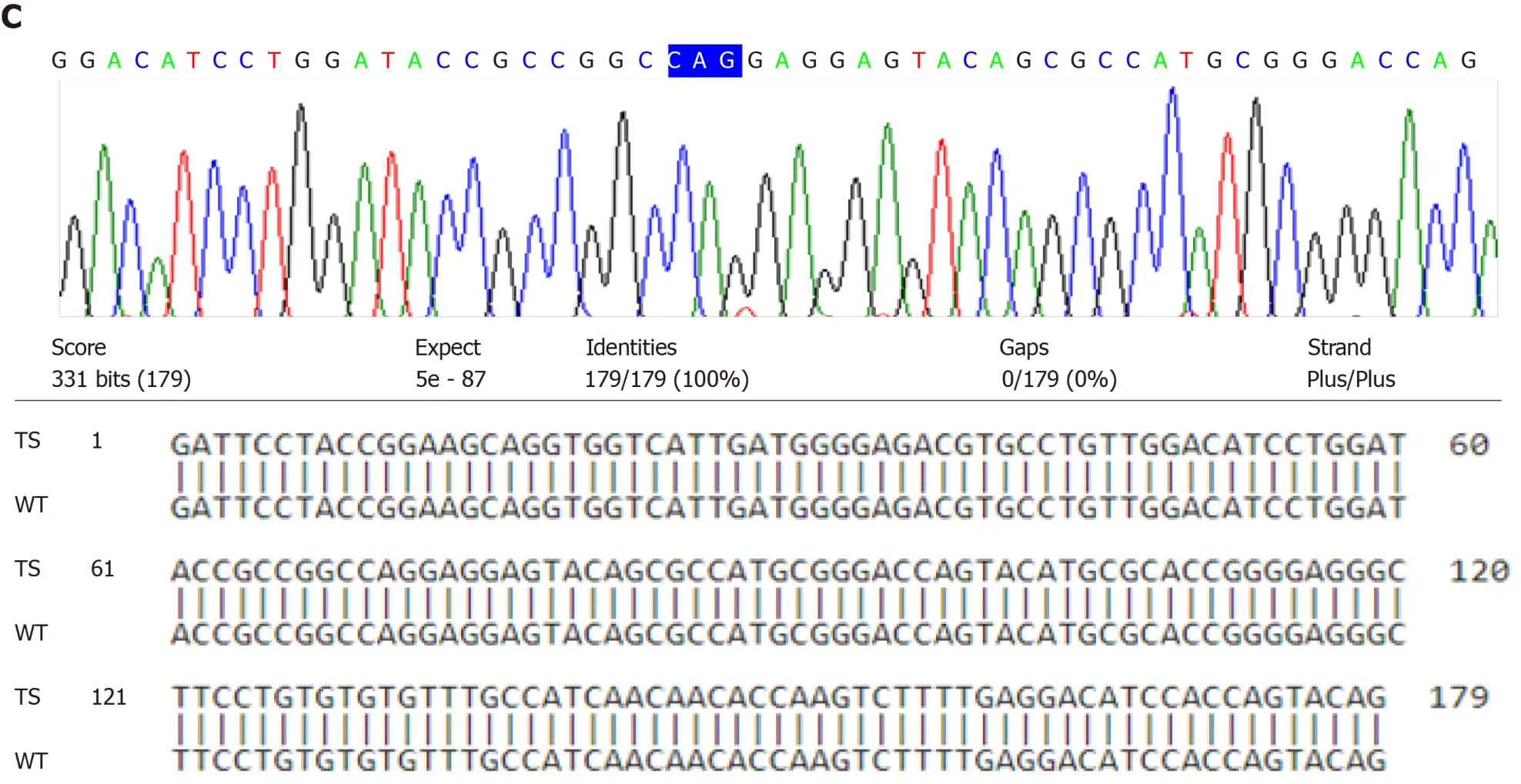
Figure1 H-Ras gene point mutation analysis in patients diagnosed with urothelial bladder cancer.
Direct DNA sequencing was performed to detect the point mutations inN-Rascoding exons 1 and 2 spanning codons 12,13;and 61,respectively.Sequencing results in the wild-type and tumor specimens were analyzed and compared.The presence of point mutations in the hotspots of codon 12 and 13 of exon 1 and codon 61 of exon 2 ofN-Rasgene was not detected in any of the bladder specimens (Figure 2B and C).
Point mutation detection in K-Ras
PCR amplification followed by RFLP was carried out to determine the presence of point mutations in codons 12 and 13 inK-Rasgene in 87 UCB and 23 normal bladder mucosal tissues.A primer was designed to create a restriction site just before the start of codon 12.Restriction digestion of the wild-type amplicon of 144 bp by enzyme BstNI resulted in its cleavage into 115 bp and 29 bp.The presence of a point mutation at codon 12 results in loss of the recognition site which is indicative of the translational change of glycine (GGT) to valine (GTT)/aspartic acid (GAT)/serine (AGT)/arginine(CGT)/alanine (GCT)/cysteine (TGT).The presence of a point mutation at codon 12 inK-Rasgene was not observed (Figure 3A).
Enzyme HphI was used to cleave the restriction site (GGTGA7/8↓) at codon 13 which is indicative of the conversion of glycine (GGC) to aspartic acid (GAC) inK-Rasgene.This site does not exist in the wild-type but tends to appear in mutants.The wild-type amplicon yielded a fragment of 144 bp when cut by HphI.Nevertheless,the presence of a mutation at codon 13 would yield two fragments of 101 bp and 43 bp oligonucleotides on restriction digestion (Figure 3B).PCR-RFLP failed to identify any mutational change in codon 13 ofK-Rasgene in tumor and normal bladder mucosal tissues.
The results of direct DNA sequencing and Blastn of coding exons 1 (spanning codons 12 and 13) and 2 (spanning hotspot codon 61) ofK-Rasgenes in tumor and normal bladder mucosal tissues exhibited 100% alignment.DNA sequencing analysis verified the results of PCR-RFLP.No point mutations in the hotspots of exonic regions 1 and 2 of theK-Rasgene were observed (Figure 3C and D).

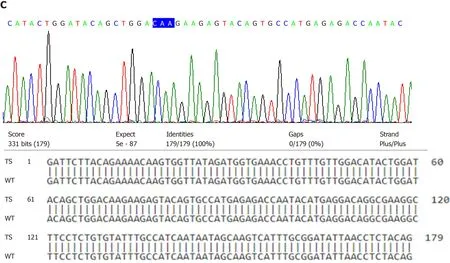
Figure2 N-Ras gene point mutation analysis in patients diagnosed with urothelial bladder cancer.
DISCUSSION
Considerable experimental evidence has demonstrated the significance of continual expression of mutantRasin tumor maintenance.Withdrawal or suppression ofRasexpression impairs thein vitrogrowth ofRas-mutant human cancer cell lines and tumor regression in mouse models driven by inducible mutantRas.These findings indicate that mutantRasis a therapeutically useful drug target even in advanced metastatic tumors[6].
Studies of a variety of tumors have demonstrated the prevalence of specific point mutations in the hotspots ofRasisoforms.These point mutations are known to transformRasproto-oncogene into an oncogene and prevent normal deactivation ofRasproteins.ActivatedRasproteins are associated with drug resistance,enhanced metastasis,poor prognosis and shorter survival of patients[7].The present study examined the mutational spectrum at the hotspot regions ofH-Rascodon 12,K-Rascodons 12,13 andN-Rascodon 61 by PCR-RFLP followed by direct DNA sequencing of the coding exons 1 and 2 of the threeRasisoforms in 87 UCB patients and their clinical impact if any.
The incidence ofRasmutations varies,and greatly depends on the tissue or cell type from which the cancer cells are derived.AlthoughRasmutations occur in 75% to 95%of pancreatic carcinomas and in 50% of colon carcinomas,they are rare in several other neoplasms[15].TheH-Rasmutation was first detected in the human bladder cancer cell line T24.Subsequent studies demonstrated the frequent occurrence ofH-Rasmutations in urinary tract tumors compared to mutations inK-RasorN-Rasgenes[21].A number of studies has reportedH-Rasmutations with variable frequencies in urinary bladder cancer specimens.Fitzgeraldet al[22]reported mutations in theH-Rasgene in 44% of urine sediments from bladder cancer patients.Czerniaket al[17]observedH-Rasmutation specifically at codon G12 in 45% of bladder cancers.Zhuet al[19]and Buyruet al[18]showed 46.7% and 39% point mutations inH-Rasat codon 12,respectively.Cattanet al[23]detected only 1% of such alterations in bladder cancer patients[23].In constrast,Przybojewskaet al[24]observedH-Rasmutations in 84% of patients with bladder cancer using PCR-RFLP.In contradiction to many earlier published studies,we did not find mutations at H-Ras codon G12 (glycine to valine/serine/alanine/aspartic acid) or in the coding exons 1 and 2 in a cohort of North Indian urothelial bladder cancer patients.
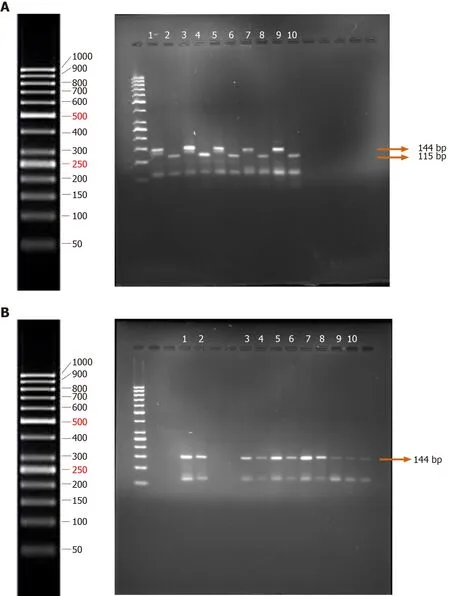

Figure3 K-Ras gene point mutation analysis in patients diagnosed with urothelial bladder cancer.
N-Rasgene mutations have mainly been associated with hematopoietic malignancies and melanoma[25,26].Results of the study by Przybojewskaet al[24]revealed the frequent prevalence (80%) ofN-Rasgene mutations at codon Q61 (glutamine to lysine) in bladder tumor tissues.These tumor tissues were obtained following infiltration of urinary bladder walls as well as peripheral blood specimens from confirmed bladder cancer patients[24].Of the total mutations detected inN-Rasgene,60% of mutations were observed in codon 61 in a cohort of North Indian patients[26].A strong association between the percentage of mutations inRasgenes and smoking status of patients (total of 78% mutations) and the age of patients (more than 60 years with total of 80% mutations) was observed.However,no association between the percentage mutation distribution and tumor stage/grade was reported[27].Jebaret al[10]examined one mutation in codon 12 and three mutations in codon 61 in 98 urinary bladder tumors and 31 bladder cell lines.Our findings on the lack ofN-Rasgene mutations in bladder cancer patients are not in accordance with published studies.Heterogeneity in the results/genomic alterations could be attributed to the differences in ethnicity,exposure to different environmental carcinogens,genetic susceptibility to carcinogens and or tissue specificity.
High frequency ofK-Rasgene mutations has been detected in many forms of cancer,including pancreatic cancer (80%-90%) and adenocarcinoma of the lung (60%)[17,22].Cancers of the lung,large intestine (including colon,rectal and anal),pancreas and biliary tract exhibited higher frequency of mutations inK-Rasgene[28].Observed similarities in the percentage distribution of mutations inK-Rascodons in lung cancer(58%) and bladder cancer (47%) could be due to the effects of tobacco consumption.Tobacco is considered an important risk factor for both of these cancers and can induce local somatic mutations in genes[13].These studies did not report an association betweenK-Rasmutations and tumor stage/grade[13].Unlike the majority of tumors that harbor an activatedK-Rasgene,changes inK-Rasgene have been observed as a rare event in urinary bladder tumors[24].Studies examined the percentage mutation prevalence at codon G12 (glycine to valine/aspartic acid/serine/ arginine/alanine/cysteine) and codon G13 (glycine to aspartic acid) inK-Rasgene as an infrequent event in bladder cancer[29,30].A study by Nandaet al[15]identified 11.67%tumors which harboredK-Rasmutations as well as a significant correlation of theKRasmutant status with the smoking history of patients,high tumor grade,lymph node involvement and tumor recurrence.Yanet al[31]reported the ability of mutantK-Ras,but notH-Ras,to confer metastatic phenotype in cells by interfering with the maturation of cell surface integrins and disrupting cell-cell adhesion.A recently published study reported a higher prevalence of point mutations in all theRasisoforms in NMIBC (27%) compared to MIBC (9.4%) patients.
In contrast to earlier published studies,our findings on the lack ofH-Ras,K-RasandN-Rasgene mutations in urothelial bladder cancer patients provide evidence for the tissue specific activation ofRasisoforms.
Discrepancies/heterogeneity in the frequency distribution of mutations at hotspot regions/codons in different isoforms ofRasgene among different cohorts of UCB patients belonging to different ethnic groups are reported in many published studies.Observed heterogeneity among different studies could be explained on the basis of different etiological mechanisms involved in disease development/progression,inherent genetic susceptibility or alternativeRasdysfunction such as gene amplification and/or overexpression.
In conclusion,Rasmutations are the most common genetic alterations known in human cancers.Single base changes/point mutations in codon 12,13 and 61 of the three closely related isoforms of theRasgene family namely,H-Ras,K-RasandN-Rascause loss of intrinsic GTPase activity and thereby confer oncogenic functions.Oncogenic activation ofRasgenes is involved in urothelial malignancies.
The present study was conducted to determine the clinical impact of mutantRasby examining the relationship of clinical histopathological variables in 87 UCB patients with the mutational spectrum at the hotspot regions ofH-Ras,K-RasandN-Rasgenes by PCR-RFLP and direct DNA sequencing.
The current observations rule out the possible role of the mutations examined in the above-mentioned hotspot regions inRasgene activation.Our findings on the lack of mutations inH-Ras,K-RasandN-Rasgenes could be explained on the basis of different etiological mechanisms involved in disease development/progression,inherent genetic susceptibility,tissue specificity or alternativeRasdysfunction such as gene amplification and/or overexpression.
ARTICLE HIGHLIGHTS
Research background
Mutational activation of Ras genes has been established as a prognostic factor for the genesis of a constitutively active RAS-mitogen activated protein kinase pathway that leads to cancer.
Research motivation
Due to the reported heterogeneity among the distribution of the most frequent mutations in Ras isoforms in different patient populations with urothelial carcinoma of the bladder (UCB),it is necessary to determine the presence/absence of mutations in order to predict disease outcome.
Research motivation
The present study was conducted to determine the mutational spectrum at the hotspot regions of H-Ras,K-Ras and N-Ras genes.
Research objectives
PCR-RFLP and direct DNA sequencing were employed to determine the presence or absence of mutations in the Ras isoforms and their clinical impact,if any,in 87 UCB patients.
Research methods
None of the 87 UCB patients showed point mutations in codon 12 of H-Ras gene;codon 61 of N-Ras gene and codons 12,13 of K-Ras gene by PCR-RFLP.Direct DNA sequencing of tumor and control bladder mucosal specimens followed by Blastn alignment with the reference wild-type sequences failed to identify even a single nucleotide difference in the coding exons 1 and 2 of H-Ras,N-Ras and K-Ras genes in the tumor and normal bladder mucosal specimens.
Research results
Our findings on the lack of mutations in H-Ras,K-Ras and N-Ras genes could be explained on the basis of different etiological mechanisms involved in tumor development/progression,inherent genetic susceptibility,and or tissue specificity in a given cohort of patients.
Research conclusions
Gene amplification and/or overexpression of Ras could further explain an alternative mechanism of its dysfunction in Ras driven cancers.
杂志排行
World Journal of Clinical Oncology的其它文章
- Intravascular lymphoma with hypopituitarism:A case report
- Proton beam therapy of periorbital sinonasal squamous cell carcinoma:Two case reports and review of literature
- Concurrent renal cell carcinoma and hematologic malignancies:Nine case reports
- Management of neuroblastoma in limited-resource settings
- Effectiveness of a novel,fixed dose combination of netupitant and palonosetron in prevention of chemotherapy induced nausea and vomiting:A real-life study from India
- Novel molecular targets in hepatocellular carcinoma
