COVID-19 with asthma:A case report
2020-09-10AiLingLiuNingXuAiJunLi
Ai-Ling Liu, Ning Xu, Ai-Jun Li
Ai-Ling Liu, Ning Xu, Ai-Jun Li, Department of Pulmonary and Critical Care Medicine, Weihai Municipal Hospital, Shandong University, Weihai 264200, Shandong Province, China
Abstract
Key words:COVID-19;Asthma;Glucocorticoids;Respiratory passage mucosa immune system;Case report
INTRODUCTION
In December 2019, a cluster of acute respiratory illnesses, now known as coronavirus disease 2019 (COVID-19), occurred in Wuhan, Hubei Province, China[1-5].The disease has rapidly spread worldwide from Wuhan.The World Health Organization declared COVID-19 a public health emergency of international concern on January 30, 2020[6].As of May 5, 2020, a total of 3489053 confirmed cases had been documented globally[7-9].
It is reported that at least 25% of patients with COVID-19 had at least one chronic disease[10].The existence of underlying conditions, especially chronic respiratory diseases, with long-term drug treatment, may affect the progress, treatment and prognosis of COVID-19.
Here, we report the course of a patient with COVID-19 combined with asthma.It took 41 d from disease onset to discharge to obtain two negative tests for this coronavirus.
CASE PRESENTATION
Chief complaints
A 48-year-old man returned to Weihai from Wuhan on January 10, 2020.He developed recurrent fever on January 20, 2020 with a maximum temperature of 38.2 °C with mild cough, without sputum, expectoration or chest tightness.Only oral antipyretics were taken.He went to the clinic on January 23, 2020 where real-time reverse-transcription polymerase chain reaction of pharyngeal swab specimens confirmed COVID-19[11].He was admitted to the hospital.
Medical history
The patient had asthma for 10 years that was stable in normal circumstances, without affecting daily life and activity.He inhaled salmeterol/fluticasone powder (Xeretide,50/500 μg) twice daily.Smoking or other medical history was denied.
Physical examination upon admission
On admission, temperature was 37.3 °C, respiratory rate was 23 breaths/min, and a few wheezing rales were heard in both lungs.Arterial blood gases at 21% fraction of inspiration O2(FiO2) showed partial pressure of oxygen (PaO2) 97 mmHg, partial arterial pressure of carbon dioxide (PaCO2) 39.5 mmHg, pH 7.393, and oxygenation index (OI, PaO2/FiO2) was 465 mmHg [normal range (NR) 400-500 mmHg].
Laboratory and imaging examinations
Laboratory parameters (Figure 1) were as follows:White blood cell count 4.66 × 109/L(NR, 3.3 × 109–9.5 × 109/L), neutrophil count 3.0 × 109/L (NR, 2 × 109–7.7 × 109/L),lymphocyte count 1.27 × 109/L (NR, 0.8 × 109–4 × 109/L), CD4 T lymphocyte count 542/μL (NR, 500–1440/μL), monocyte count 0.35×109/L (NR, 0.12 × 109–0.8 × 109/L),eosinophil count 0.03 × 109/L (NR, 0.05 × 109–0.5 × 109/L), platelet count 135 × 109/L(NR, 125 × 109–350 × 109/L), lactate dehydrogenase (LDH) 166 U/L (NR, 100–190 U/L), alanine transaminase (ALT) 15 U/L (NR, 0–50 U/L), aspartate transaminase(AST) 20 U/L (NR, 5–35U/L), albumin 39.8 g/L(NR, 38–55 g/L), C-reactive protein(CRP) 10.94 mg/L (NR, <4 mg/L).Procalcitonin, myocardial enzymes, serum electrolytes and renal and liver function tests were normal.Detection of antigen and antibody of respiratory tract pathogenic spectrum (including influenza virus A/B) was negative.Chest X-ray showed increased lung markings in both lungs.
FINAL DIAGNOSIS
Confirmed COVID-19 combined with asthma.
TREATMENT
Lopinavir/ritonavir (Kaletra/Aluvia) and moxifloxacin were given orally.The patient’s condition gradually worsened with repeated fever, chest distress, wheezing and diarrhea.Chest computed tomography (CT) images (Figure 2) on day 6(Figure 2A) after symptom onset (from January 20, 2020) showed ground-glass opacity(GGO) in the right lung.Neutrophil count, CRP, ALT, AST, LDH and fibrinogen increased, and platelet count, OI and albumin decreased.Procalcitonin was normal.He was treated with oxygen, intravenous methylprednisolone (40 mg q12h), aerosol inhalation of terbutaline combined with budesonide, interferon and traditional Chinese medicine.


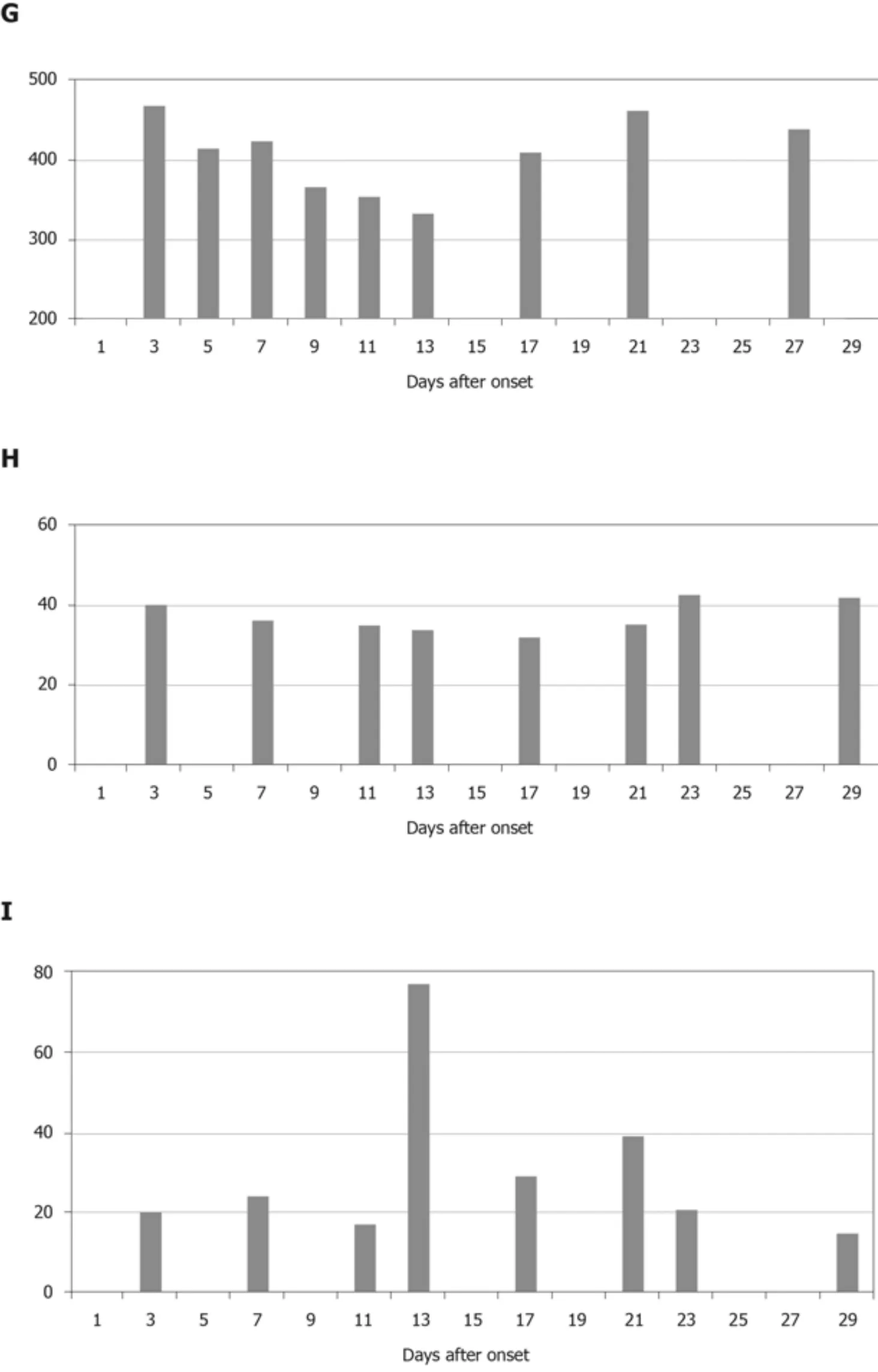
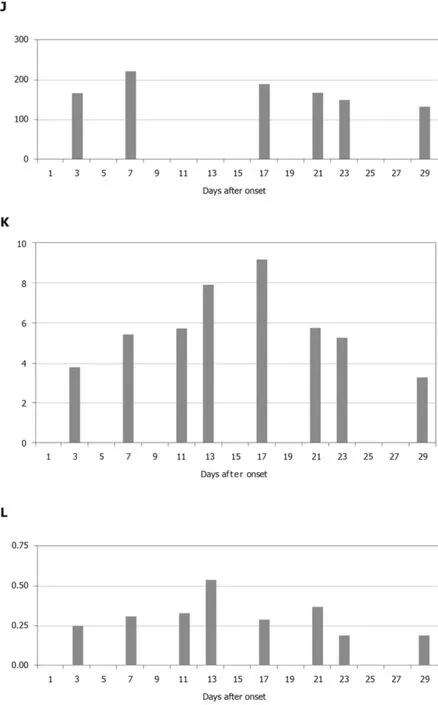
Figure 1 Dynamic profile of laboratory parameters in a 48-year-old male with coronavirus disease 2019 and asthma.
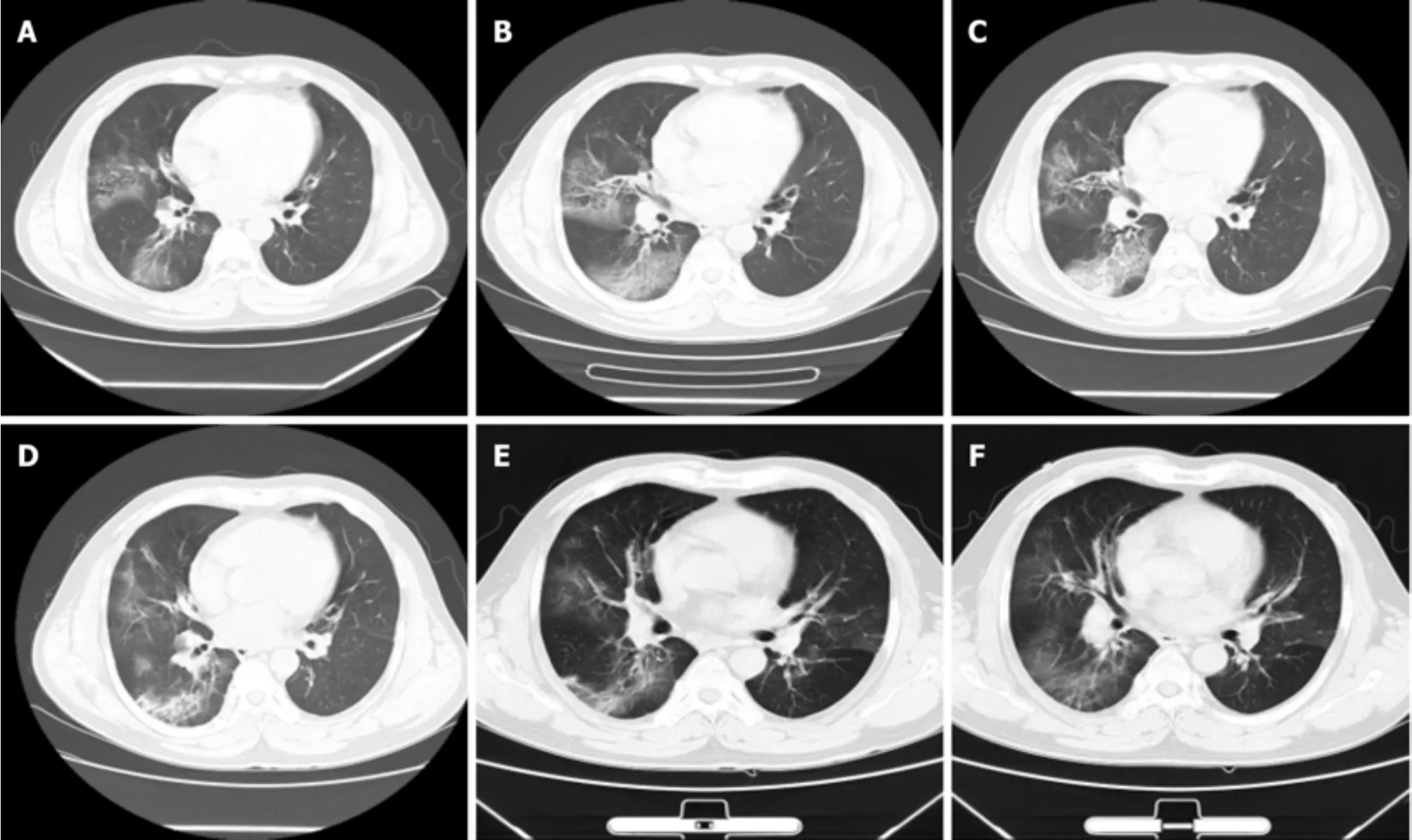
Figure 2 Chest computed tomography images of a 48-year-old male with coronavirus disease 2019 and asthma showing dynamic changes of lesions.
OUTCOME AND FOLLOW-UP
The disease peaked on day 12 after symptom onset.CT images on day 13 (Figure 2C)indicated that the density of lesions was higher than before.After treatment, the patient’s temperature gradually stabilized, and his symptoms improved.His condition was stable from day 17 without fever, cough, chest pain, chest tightness or diarrhea.Laboratory parameters gradually improved.CD4 T lymphocyte count was 793/μL.Therapy was changed to inhaled salmeterol/fluticasone powder (Xeretide, 50/500 μg)and symptomatic treatment.CT images on day 20 (Figure 2D) after symptom onset showed visible absorption.Virus detection by nasopharyngeal swab or sputum was persistently positive.We tested by PCR every 2-4 d.On day 41 (March 1, 2020) after symptom onset (January 20, 2020) the patient was discharged after two consecutive negative tests from nasopharyngeal swabs and sputum (>24 h interval).
DISCUSSION
COVID-19 is a public health emergency of international concern[6].The global population lacks immunity to COVID-19 and is generally susceptible.The existence of underlying conditions, especially chronic respiratory diseases, may affect the progress,treatment and prognosis of COVID-19[12].
The Chinese Center for Disease Control and Prevention traced back to February 11,2020 that there were 20982 new cases of COVID-19 reported that were combined with underlying diseases.The 511 patients with chronic respiratory diseases (2.4% in all)had a crude mortality rate of 6.3%, higher than 6% in patients with hypertension and 5.6% in cancer patients, and much higher than 0.9% of patients without underlying diseases[13].
Therefore, it is important to pay attention to the observation and active treatment of chronic underlying diseases in COVID-19 patients.Although the patient reported here suffered from asthma, he usually had good control and regular inhalation medicine.We continued his usual treatment when admitted.
The period between exposure and onset was 10 d, and the early clinical manifestations were fever and dry cough.There was no obvious severe dyspnea in the early stage of the disease.It is reported that most patients have dyspnea during disease progression, and a few patients have hemoptysis, diarrhea and other manifestations[11,14].Laboratory findings showed that routine blood analysis, blood gas analysis, myocardial enzymes, serum electrolytes and renal and liver function tests were normal, and CRP increased.X-rays showed no sign of pneumonia.The clinical characteristics of this case were consistent with previous reports[10].
The patient’s condition gradually worsened with repeated fever, chest distress,wheezing and diarrhea.It is necessary to distinguish whether the aggravation of symptoms was caused by an acute attack of asthma or progression of pneumonia.CT confirmed progression of pneumonia, and exacerbation of infection induced an acute attack of asthma.
After aggravation, chest CT indicated diffuse GGO, increased neutrophil count,CRP, ALT, AST, LDH and fibrinogen and decreased platelet count, OI and albumin.Procalcitonin was normal.
The changes in chest CT imaging can be divided into different periods.Early in the disease, GGO is found.After progression of the disease, diffuse GGO and consolidation develop.In the absorption period, the consolidation is gradually absorbed.After dissipation, the lesion is absorbed or some fiber strip shadow remains.Panet al[15]divided the dynamic changes in CT into four different periods according to the days after initial symptoms, in a similar manner to the present case.
Our patient had a normal peripheral blood leukocyte count.Increased neutrophil count and CRP were mainly associated with bacterial infection.Neutrophilia may be related to the coronavirus-induced cytokine storm, but in some severe cases,leukocytopenia may occur.Lymphocyte count was lower than at admission.But as the patient recovered, it gradually increased.Lymphocytopenia is common in patients with COVID-19, and in some cases it is severe.Our finding was consistent with recent reports[16].Eosinophil and platelet counts decreased as the disease progressed, which was related to myelosuppression.ALT, AST and LDH fluctuated in different periods,under the influence of COVID-19 or some drugs with hepatotoxicity.Lower albumin showed poor nutritional status as the disease progressed.In patients with COVID-19,prolonged PT, increased D-dimer and fibrinogen have been described and are more common in severe cases[10,12,16].Coagulation may be related to sustained inflammatory response.We found increased D-dimer and fibrinogen, consistent with previous studies[10].
The final diagnosis was confirmed as COVID-19 combined with asthma.There was no evidence of other virus infections.The patient had higher neutrophil count and CRP, CT indicated diffuse GGO, and bacterial infection was considered.Moxifloxacin was given as an antibacterial agent.Lopinavir/ritonavir (Kaletra/Aluvia) and interferon were used as antiviral agents on recommendation of the diagnosis and treatment plan formulated by the Chinese National Health Commission[17].There was not much experience in antiviral treatment at the beginning of the coronavirus epidemic.Now there are a variety of potentially effective recommended drugs, such as lopinavir/ritonavir, interferon, ribavirin, chloroquine phosphate and arbidol[17].
Glucocorticoids are the basic drug therapy for asthma, but their application in viral pneumonia is controversial.Glucocorticoids are believed to be able to antagonize some pathophysiological processes of acute respiratory distress syndrome, including excessive inflammatory response, excessive cell proliferation and abnormal collagen deposition.A review of the Cochrane system showed that glucocorticoids reduce mortality of patients with severe community-acquired pneumonia[18].For coronavirus infection, glucocorticoids were widely used during the epidemic of severe acute respiratory syndrome (SARS) in 2003.A retrospective cohort study showed that glucocorticoids reduce mortality and hospital stay[19].However, some studies showed that glucocorticoids might increase the mortality of SARS and delay virus clearance[20].Therefore, glucocorticoids should be used cautiously in patients with coronavirus pneumonia, and the indications and dosage should be strictly limited.Nevertheless, it is essential for the control and maintenance of underlying diseases.In the present patient, methylprednisolone was used for 3 d, followed by inhaled corticosteroid(ICS).His condition was stable from day 17, but virus detection was persistent until day 41 after symptom onset.Intravenous or oral glucocorticoids may inhibit the immune response and delay virus clearance[21], but it is not known whether ICSs have the same effect.
The respiratory mucosa immune system (RMIS) refers to the lymphoid tissue distributed in the respiratory mucosa and some exocrine glands.The RMIS makes contact with external antigens (such as symbiotic bacteria and harmful pathogens)directly on the surface of the mucous membrane.It is the first line of defense against invasion by respiratory pathogens.It can recognize and respond to inhaled antigens,generate effective immunity for rejection or elimination of harmful antigens or pathogens[22].The RMIS consists of cells and molecules such as T lymphocytes, B lymphocytes, natural killer cells, bronchial epithelial cells, dendritic cells and secretory IgA[22,23].ICSs can inhibit expression of inflammatory factors and chemokines, inhibit leukocyte infiltration and enhance intercellular adhesion so as to maintain epithelial integrity[24].Prosperiniet al[25]showed that the number of epithelial cells in sputum decreased after treatment with ICSs.Fukushimaet al[26]found that after treatment with ICS total IgA in saliva of asthmatic patients with positive oral candidiasis decreased.The efficacy and adverse reactions of ICSs are closely related to the RMIS.ICSs may affect immunity and virus clearance from local bronchi and alveoli.At present, no randomized controlled trial has confirmed this.
CONCLUSION
We have reported a typical case of COVID-19 with asthma.This case indicates the dynamic clinical characteristics, laboratory results, CT findings and adjustment of treatment.We have discussed the possible relationship between glucocorticoid therapy and virus clearance.We hope that this case provides more ideas for future research.
杂志排行
World Journal of Clinical Cases的其它文章
- Impacts and challenges of United States medical students during the COVID-19 pandemic
- Recent advances in the management of gastrointestinal stromal tumor
- Medical research during the COVID-19 pandemic
- Progress of intravoxel incoherent motion diffusion-weighted imaging in liver diseases
- Typical and atypical COVID-19 computed tomography findings
- Review of possible psychological impacts of COVID-19 on frontline medical staff and reduction strategies
