Impacts and challenges of United States medical students during the COVID-19 pandemic
2020-09-10StaceyRolakAlexisKeefeEmilyDavidsonPrabeshAryalSandeshParajuli
Stacey Rolak, Alexis M Keefe, Emily L Davidson, Prabesh Aryal, Sandesh Parajuli
Stacey Rolak, Alexis M Keefe, Emily L Davidson, Department of Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI 53705, United States
Prabesh Aryal, College of Medicine, Nepalese Army Institute of Health Sciences, Kathmandu 44600, Nepal
Sandesh Parajuli, Division of Nephrology, Department of Internal Medicine, University of Wisconsin School of Medicine and Public Health, Madison, WI 53705, United States
Abstract
Key words:COVID-19;Education;Medical students;Telemedicine;Healthcare delivery;Schools
INTRODUCTION
The emergence of the coronavirus disease 2019 (COVID-19) has placed immense strain on healthcare, economic, and social systems globally.Social distancing practices have been adopted in attempts to “flatten the curve” of the virus to protect the health of the public and preserve healthcare resources.Multiple sectors of society have rapidly adjusted to new technologies and communication modalities to remain operational.Healthcare specifically has been hit particularly hard, with nation-wide shortages of personal protective equipment (PPE), workforce shortages, and high risk of disease transmission.Consequently, the emergence of COVID-19 in the United States has heavily disrupted undergraduate medical education in all stages of training.This opinion review will elucidate how COVID-19 has disrupted traditional medical education, outline a variety of medical student responses to the pandemic, and discuss the potential roles of medical students in the future.
COVID-19 AND TRADITIONAL UNDERGRADUATE MEDICAL EDUCATION
Medical student education in the United States has historically been structured as two years of pre-clinical coursework, followed by two years of clinical training.During the pre-clinical years, students learn the basic sciences, anatomy, pharmacology, and begin practicing basic clinical skills.During the clinical years, students rotate through different core clerkships, including pediatrics, internal medicine, surgery, neurology,and obstetrics and gynecology, and participate in elective rotations.Many schools are adopting innovative curricula with 12-18 mo of basic sciences, followed by 12 mo of core clerkships, and 12-18 mo of individualized learning to explore different careers through advanced clinical rotations, scholarly projects, sub-internships, and audition rotations at different institutions[1,2].COVID-19 has altered medical education at each of the pre-clinical, core clerkship, and advanced career exploration stages[3].
As COVID-19 spread throughout the United States, the Association of American Medical Colleges (AAMC) and Liaison Committee on Medical Education (LCME), two governing organizations on medical student education and school accreditation,published general recommendations for student education.For students in their preclinical years, the AAMC recommended that each school guide their own education delivery based on institutional policies and public health guidelines.Many schools have implemented changes to protect students, faculty, and standardized patients, as summarized in Figure 1.For students in their core clinical rotations or advanced clinical rotations, recommendations have been even more varied, and the disruption of education during this crucial time of career exploration has been stressful for many.On March 17, 2020 the AAMC first suggested that medical schools temporarily suspend clinical rotations.More recent recommendations suggest that unless there is a critical healthcare workforce need locally, medical students should refrain from direct patient care activities.They outline PPE restrictions and limited availability of COVID-19 testing as reasons for this suggestion.Without these resources, it will be difficult to resume providing clinical experiences to medical students.
LCME guidance stated that in preparing for future rotations, schools could shorten their core clerkship lengths.Their standards do not support a complete clerkship being taught online;however, they posit that it is acceptable for some course content to be delivered virtually.Each school has been adapting differently to provide relevant online coursework in lieu of in-person clerkships, and are adjusting how they will format clerkships in the future[3].Some of these adjustments are highlighted in Figure 1.
In addition to these coursework changes, the ability to take the United States Medical Licensing Exams (USMLE) was interrupted with the temporary closure of Prometric Testing Centers, our nation’s proctoring sites for USMLE Step 1 and Step 2 Clinical Knowledge.Step 2 Clinical Skills, which requires interactions with standardized patients, was also suspended, and on May 26ththe USMLE announced that the exam would continue to be suspended for the next 12-18 mo.It is generally recommended to complete Step 1 and Step 2 Clinical Knowledge before residency application season in the fall of students’ fourth year.There has been no comprehensive national guidance on how testing delays will affect residency applications or graduation, though the USMLE governing board has been pursuing and implementing alternative test delivery options on medical school campuses.
Some medical students set to begin their internships in June of 2020 have graduated early to bolster the healthcare workforce in areas most affected by COVID-19.The LCME guided this transition.While some students geared up to begin their residencies early, Match Day celebrations and graduation ceremonies were cancelled and held virtually throughout the country.
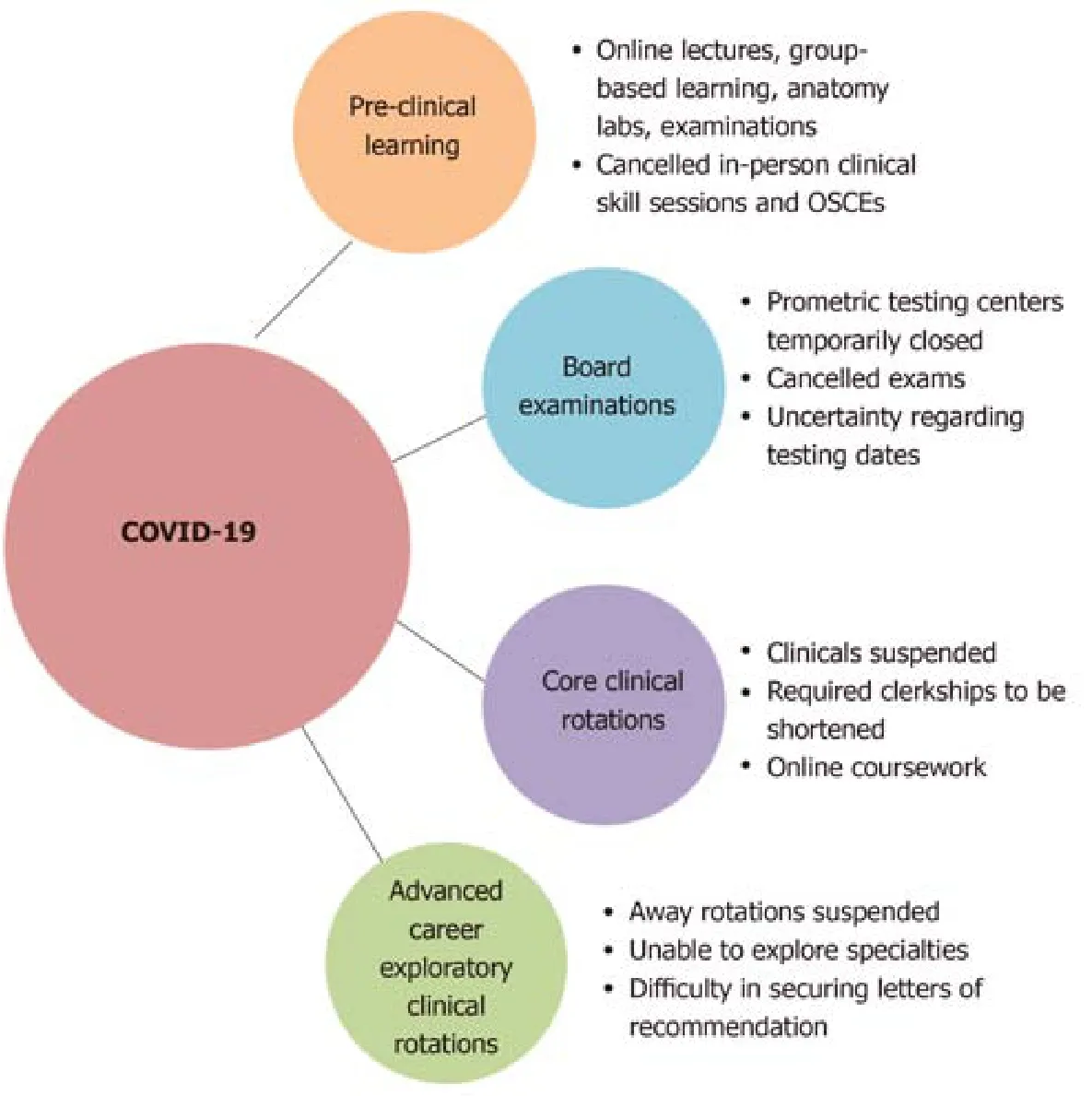
Figure 1 Education changes due to coronavirus disease 2019.
BARRIERS TO MEDICAL STUDENT CLINICAL EDUCATION
Medical students receive their clinical education through preceptorships and clerkships at teaching institutions.As these experiences cannot be readily delivered virtually, students in their core clinical rotations and advanced clinical rotations are most tangibly affected by the current medical education changes.Medical students are considered non-essential in the delivery of clinical care, and require attending physician supervision of their work.Students may potentially act as vectors of viral transmission between different patients and personnel, and may be asymptomatic carriers, although further research on viral epidemiology is needed to determine this risk.These limitations, combined with medical institutional adaptations to COVID-19,have made it difficult to strike a balance of providing supervised learning opportunities to students.
As medical systems face furloughs and provider and administrative salary cuts,there may not be sufficient faculty and resident availability for medical student teaching and supervision.Non-COVID-19 related emergency room visits and general medicine admissions for non-COVID-19 problems have purportedly decreased at some institutions.There is also limited capacity for medical students to be involved on procedural and surgical rotations, given limited PPE and fewer elective cases being performed.The adequacy of administrative staff to schedule and facilitate student learners through their rotations also varies by institution and discipline, and is another factor precluding medical student participation in the clinical environment.
Many health systems have transitioned to telemedicine visits for both inpatient and outpatient visits in light of social distancing[4-6].Telemedicine has been adopted to triage and manage suspected COVID-19 patients, as well as outpatient non-COVID-19 patients, to ensure continuity of care for patients.Telemedicine is important in reducing face-to-face contact between healthcare practitioners and patients, reducing the risk for viral transmission, and eliminating the need for travel to visits.More widespread use of telemedicine is a great adaptation to COVID-19, though there are limitations to its use, including administrative and regulatory barriers to telemedicine between institutions, and payment discrepancies between telemedicine and in-person services[7].Because direct contact is not required in telemedicine, one would think that it is a system that medical students could readily be involved in.There has recently been increased integration of telemedicine-based lectures, clinical cases, and case studies in medical education[8].The 2015-2016 LCME Annual Medical School Questionnaire showed that over 25% of Medical Doctor programs have implemented some component of telemedicine training into their pre-clinical education, and over 50% have integrated telemedicine education into the clerkship phase[8].However, it is not heavily emphasized in many curriculums, and medical students report low confidence in utilizing telemedicine efficiently[8].Therefore, more training is needed to make this a viable option for students, and this is an option that should be explored in the future.
MEDICAL STUDENT RESPONSES TO COVID-19
Amidst the turmoil of COVID-19, medical students in all stages of training have demonstrated a true commitment to service by mobilizing to help their communities.Some of these actions are highlighted in Figure 2.At Harvard Medical School, students created a COVID-19 Medical Student Response Team for medical and community education and activism, to efficiently mobilize students in the COVID-19 response[9].Medical students at a variety of institutions throughout the United States are volunteering at equipment donation centers, food drives, providing childcare for medical personnel, and grocery shopping and running errands for residents and physicians.Some students are using telecommunications to translate patient visits.Others are involved in supervised telemedicine visits, such as virtual prenatal health visits.The ingenuity and altruism of students in creating ways to help and mobilize resources is remarkable.The prevailing sentiment is that medical students want to be helpful and prepared for the future.
Some medical students have disagreed with the AAMC recommendations that medical student involvement in patient care should be reserved for critical healthcare personnel shortages[10].They highlight the accurate point that medical students can help with routine outpatient telemedicine visits by interviewing patients and documenting their histories;following up with patients on lab and test results;and assisting with patient education.They also argue that medical students can help with daily hospital inpatient tasks for non-COVID patients that don’t require PPE.This is all recognized within the need for student and patient safety[10].
As current third year medical students, we acknowledge and appreciate that staying at home was a necessary precaution for us during this emerging pandemic, given the current barriers to our education and safety, and the rapid changes required of the healthcare system.However, as healthcare delivery adapts and we brace for the possibility of a continuous presence and resurgence of COVID-19, governing educational bodies and teaching institutions must be proactive in reinstating our clinical roles in order to ensure that the future physicians of the United States receive high-quality education.We want to have secure and equal opportunities to learn and explore our career goals.
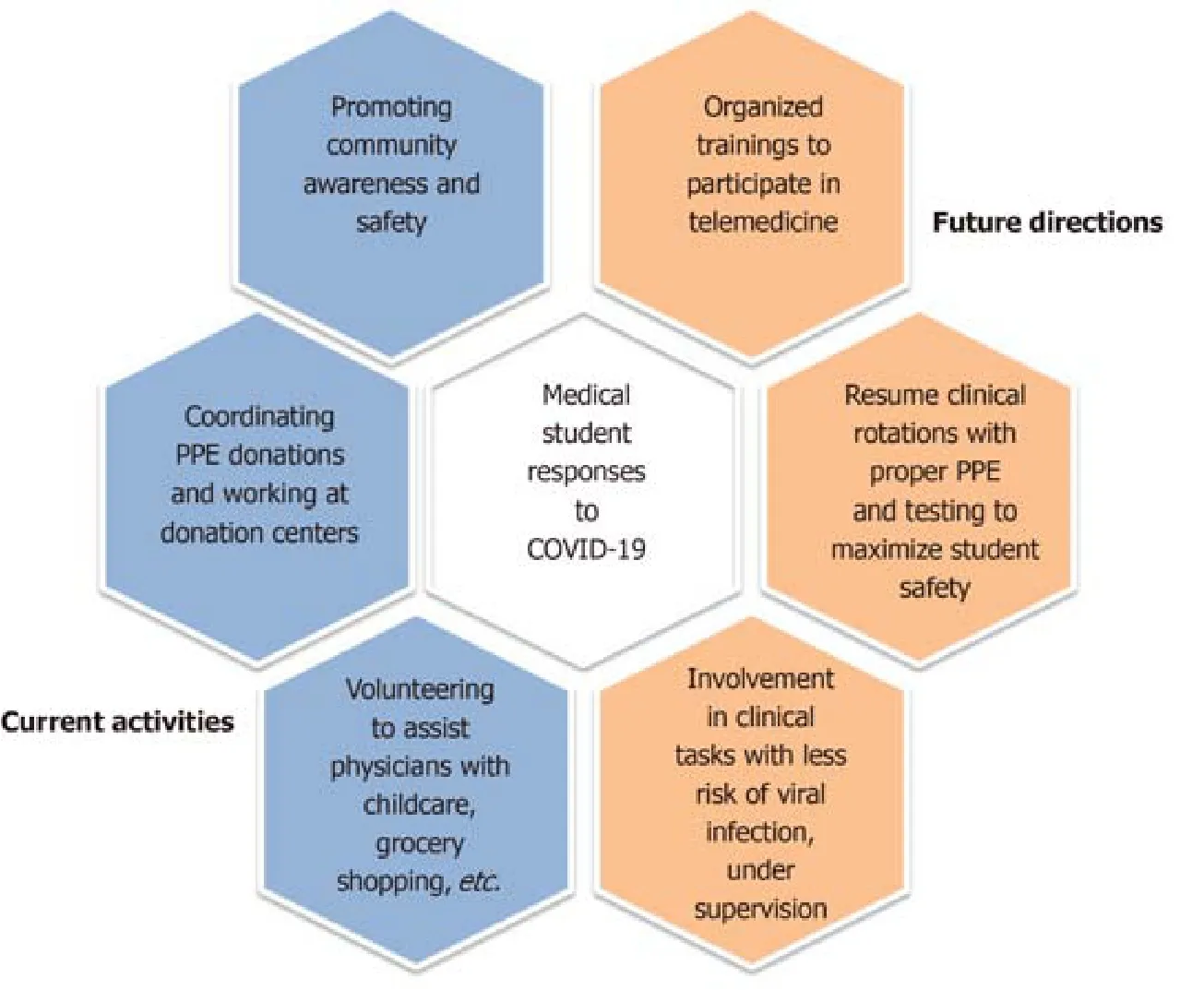
Figure 2 Medical student responses to coronavirus disease 2019.
FUTURE INVOLVEMENT OF MEDICAL STUDENTS
There are many questions regarding how long COVID-19 will continue to interrupt medical education.Since much is unknown about the future of the disease, a contingency plan must be set in place so our education will not be so heavily perturbed in the future.Students in their clinical years of medical school are overall eager to resume their clinical rotations.Some options for future medical student involvement are summarized in Figure 2.
As access to PPE and supervision improve, students should have the opportunity to return to critical learning experiences.With these resources available, the historical roles of medical students as part of the healthcare team should not change.Medical students in their clinical years positively contribute to patient care by obtaining medical histories, initiating documentation, and communicating with patients, family members, and consulting services.As health systems phase in elective and non-urgent surgical procedures and in-person visits, students should be able to return to these learning environments as well.Additionally, pre-clinical students can be reinstated to in-person clinical skills sessions to build their framework for the approach to physical exams and histories.
We recognize that some students have personal health concerns or objections to participating in clinical care at this time.Students should not be coerced to participate in potentially unsafe situations, and it may be necessary for medical schools to adopt no-consequence opt out policies for students in certain medical settings such as caring for patients with respiratory complaints or in intensive care units.Medical students are adult learners with the decision-making capacity to participate in patient care, and we argue that these opportunities should, at the very least, be available to us.
As continued social distancing will likely be required barring the development of a vaccine and widespread testing, alternative avenues must be explored to maintain student involvement in clinical activities.As mentioned previously, implementation of a telemedicine curriculum would be beneficial, and could include proper virtual etiquette and remote physical exam skills.Training future physicians on how to utilize this technology would continue the momentum that COVID-19 has kickstarted.Like any other clinical training, this too would require physician supervision, but is especially advantageous in allowing for non-contact clinical experiences during COVID-19 and beyond.
Medical students have demonstrated professionalism, dedication to the field,compassion, and humanism in their efforts to engage with communities and support residents and physicians during this COVID-19 pandemic.We are the future of the healthcare workforce and have clinical skills to offer to medical teams, and arguably should be involved in learning to care for patients during a pandemic, as we will be on the frontlines in the future.Many of us are eager to return to“normal”life to continue learning medicine and serving others.Overcoming the logistical barriers to achieve this transition will require continuous adaptation and resilience from medical institutions, educators, and students alike.
CONCLUSION
We have addressed many uncertainties surrounding COVID-19.For student and population safety, valuable clinical experiences have understandably been traded for temporary online coursework, leaving much unknown about the transition back to inperson training and clinical clerkships.Across the nation, medical students continue to engage with the communities that they will serve as physicians.Teaching institutions have quickly evolved to deliver an online curriculum to best meet the needs of their student learners.As testing, personal protective equipment, and information about virus epidemiology become more available, medical students are eager to return to their studies and contribute as members of their healthcare teams.As long as options are available to students and safety is protected, we believe that students should be welcomed back to doing what they want to do most–learn medicine.Specific policy adjustments concerning clinical care, along with an implementation of telemedicine curriculum, will help transition students safely back to the bedside.
杂志排行
World Journal of Clinical Cases的其它文章
- Recent advances in the management of gastrointestinal stromal tumor
- Medical research during the COVID-19 pandemic
- Progress of intravoxel incoherent motion diffusion-weighted imaging in liver diseases
- Typical and atypical COVID-19 computed tomography findings
- Review of possible psychological impacts of COVID-19 on frontline medical staff and reduction strategies
- Overexpression of AMPD2 indicates poor prognosis in colorectal cancer patients via the Notch3 signaling pathway
