Clinical observation of Zhen’ai needling method in Nei Jing (Classic of Internal Medicine) for children with allergic rhinitis accompanied by adenoid hypertrophy
2020-08-29ZhangCuihong张翠红LiuZhanwen刘占文HongJue洪珏LiuJie刘婕XieChen谢晨WuLingxiang吴凌翔YangYanting杨延婷MaXiaopeng马晓芃
Zhang Cui-hong (张翠红), Liu Zhan-wen (刘占文), Hong Jue (洪珏), Liu Jie (刘婕), Xie Chen (谢晨),Wu Ling-xiang (吴凌翔), Yang Yan-ting (杨延婷), Ma Xiao-peng (马晓芃)
1 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
2 Shanghai Changning District Mental Health Center, Shanghai 200335, China
Abstract
Keywords: Acupuncture-moxibustion Therapy; Acupuncture Therapy; Point, Shanglianquan (Extra); Point, Tianrong (SI 17); Point, Lieque (LU 7); Rhinitis, Allergic; Adenoid Hypertrophy
Allergic rhinitis (AR) is a non-infectious inflammation of the nasal mucosa triggered by the contact with allergens, mainly mediated by IgE. It is a common disease in clinic[1]. In recent years, the incidence rate of AR in children has been increasing due to environmental pollution and unreasonable use of antibiotics[2-3]. The four main symptoms of AR are sneezing, runny nose, nasal itching and nasal obstruction, which can cause dizziness, headache, low spirit and hypomnesia. In severe cases, it can induce life-threatening complications such as asthma, pulmonary heart disease and emphysema, seriously affecting the quality of life of patients. The adenoids are pharyngeal tonsils. Adenoid hypertrophy (AH) refers to the pathological hyperplasia of adenoids due to repeated inflammatory responses. Because of nasal congestion and nasal reflux to the throat, AR is easily complicated with AH[4]. Study has reported that the incidence of AH in children with AR is 21.2%[5]. AH and AR are more relevant than other allergic diseases[6-7]. Children with AR accompanied by AH are vulnerable to systemic symptoms such as attention deficit, hypomnesia, learning difficulties, hyperkinetic disorder, anxiety and depression, which most scholars believe are related to abnormal sleep pattern caused by hypoxia at night and frequent nocturnal awakening[8].
Most treatments of modern medicine for such diseases are oral leukotriene receptor antagonists or hormone nasal spray, or surgeries in severe cases. Most of these drugs are symptomatic treatments and unable to cure the disease. Long-term applications may cause different levels of adverse reactions[9]. And resection operation has potential threats such as high anesthesia risk and various complications[10]. Adenoids are located at the junction of the top of the nasopharynx and the posterior wall. They play an important role in the local immune function of the pharynx and the entire upper respiratory tract in children, especially in children aged 3-5 years. They are the first defense gateway of the respiratory tract. Adenoids generally begin to atrophy after 10 years old, and most of them disappear in adulthood. Therefore, it is not recommended to surgically remove adenoids in children with AH. It is very important and meaningful to find a safe and effective conservative treatment for children with AR accompanied by AH. Acupuncture treatment has certain efficacy for AR and AH[11-12]. In this study, we observed the efficacy of points of Zhen’ai needling method inNei Jing(Classic of Internal Medicine) based on the conventional acupoint selection for children with AR accompanied by AH, in order to provide clinical evidence for acupuncture treatment of AR accompanied by AH.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of AR
This study referred the diagnostic criteria in the
Guidelines for the Diagnosis and Treatment of Allergic Rhinitis(2009, Wuyishan)[13]: at least two symptoms of sneezing, runny nose, nasal obstruction, and nasal itching, cumulative or lasting for more than 1 h per day; runny nose, nasal mucosa edema, pale nasal mucosa; may be accompanied by conjunctival congestion, itchy eyes and other symptoms.
1.1.2 Diagnostic criteria of AH
The diagnostic criteria of AH referred thePractical Pediatric Respiratory Medicine[14]: mouth breathing, nasal obstruction, snoring, and typical face of adenoid sometimes; visible red massive swelling in the nasopharynx by anterior rhinoscopy with nasal mucosa fully contracted; lobulated lymphatic tissue with longitudinal fissures on the top and posterior wall of the nasopharynx could be seen by nasal endoscopic examination run by the otolaryngology department of a regular class 2 and grade A hospital or above.
1.2 Inclusion criteria
Those who met the above diagnostic criteria of AR and AH; aged between 3 and 15 years old, without gender limitation; with a duration over 6 months; their guardians were fully aware of the study process, and signed informed consent.
1.3 Exclusion criteria
Those with severe systematic diseases; with acute infectious diseases; who had aspirin or steroids for over 6 months; coupled with nasal polyps or abnormally deflected nasal septum; those with a personal or family history of allergic diseases; with a clear history of inhalation sensitization; who had liver or kidney dysfunction; those with poor compliance, or were reluctant to accept the interventions; psychotics.
1.4 Elimination criteria
Those who did not follow the treatment protocol; those took medication out of the treatment protocol; those presenting with adverse reactions during treatment (recorded the adverse reactions and stopped the treatment).
1.5 Shedding criteria
Those who were unable to receive the treatment within the prescribed time; those dropped out during the treatment; those who dropped out after more than half of the treatment course were counted as invalid in the evaluation of efficacy.
1.6 Statistical method
All data were statistically analyzed by the SPSS version 18.0 statistical software. Measurement data in normal distribution were expressed as mean ± standard deviation (±s). Pairedt-test was applied to the intra-group comparisons. Independent samplet-test was applied to the comparisons between the groups. Measurement data in non-normal distribution were processed by Wilcoxon rank-sum test. Chi-square test was used for the comparison of rate.P<0.05 was considered to indicate a statistically significant difference.
1.7 General data
A total of 74 cases were enrolled, collected from the Clinic of Shanghai Research Institute of Acupuncture and Meridian, between January 2015 and December 2019. All cases were randomly divided into a control group and a Zhen’ai group by the random number table, with 37 cases in each group. During the treatment, 5 cases dropped out in the control group and 2 cases in the Zhen’ai group. There were no statistically significant differences in gender, age, or duration of disease in those who completed the required treatment between the two groups (allP>0.05), indicating that the two groups were comparable (Table 1).
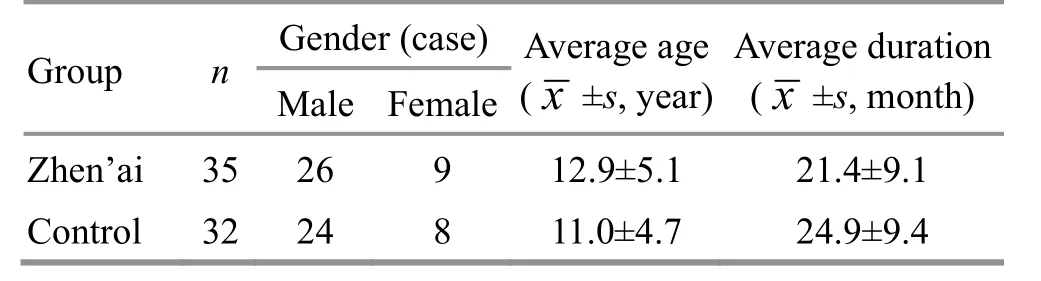
Table 1. Comparison of the general data between the two groups
2 Treatment Methods
2.1 Control group
Points: Yintang (GV 29), Shangxing (GV 23), Baihui (GV 20), and bilateral Zusanli (ST 36), Hegu (LI 4), Juliao (ST 3) and Yingxiang (LI 20).
Methods:The patient took a supine position. After routine disinfection, the physician perpendicularly punctured Zusanli (ST 36), Hegu (LI 4) and Juliao (ST 3) using sterile acupuncture needles of 0.25 mm in diameter and 40 mm in length; obliquely punctured Yingxiang (LI 20) upwards to Shangyingxiang (EX-HN 8); punctured Yintang (GV 29) by finger-squeezed insertion method, with the tip of needle reaching the nasal root, so that the needling sensation would spread to the tip of the nose; subcutaneously punctured Shangxing (GV 23) and Baihui (GV 20) with the tip of needles towards the back. The needles were retained for 30 min after qi arrival.
Cupping: After needle withdrawal, the patient took a prone position with back exposed. The physician applied flash-fire cupping method along the Bladder Meridian on the back. The skin was sucked into the cup for 5-8 mm, and the cups were removed 3-5 min later.
2.2 Zhen’ai group
Points: Same conventional points as those in the control group, Shanglianquan [Extra, located at 1 cun above Lianquan (CV 23)], and bilateral Tianrong (SI 17) and Lieque (LU 7).
Methods:The acupuncture methods for the same points were same as for the control group. Shanglianquan [Extra, located at 1 cun above Lianquan (CV 23)] and Tianrong (SI 17) were punctured with the needle tip towards the throat; Lieque (LU 7) was obliquely punctured with the needle tip upwards. After arrival of qi, even reinforcing-reducing manipulation was performed, and the needles were retained for 30 min.
Cupping: The cupping method was applied in the same way as for the control group after needle withdrawal.
The treatment was performed twice a week for both groups, 5 times as a course of treatment, and the efficacy was evaluated after 2 courses of treatment.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Total nasal symptom score (TNSS)
Four nasal symptoms were scored 0-3 points before and after treatment by the patients and their guardians, and the TNSS scores were obtained by summing of all component scores. The highest score of TNSS was 12 points. The higher the score, the more severe the symptoms[15].
3.1.2 Sino-nasal outcome test-20 (SNOT-20)
Twenty symptoms closely related to rhinitis were scored 0-3 points before and after treatment by the patients and their guardians, and SNOT-20 scores were obtained by adding the scores of each item. The highest score of SNOT-20 was 60 points. The higher the score, the more severe the symptoms[16].
3.1.3 Symptom scale for adenoid hypertrophy (SSAH)
Four AH symptoms were scored 0-3 points before and after treatment by the patients and their guardians, and SSAH score was obtained by adding the scores of each item. The highest score of SSAH was 12 points. The higher the score, the more severe the symptoms[17].
3.2 Criteria of curative efficacy
The curative efficacy was evaluated according to the symptoms, signs and SSAH reduction rate of the children[18-19].
SSAH reduction rate = (SSAH score before treatment – SSAH score after treatment) ÷ SSAH score before treatment × 100%.
Markedly effective: The symptoms and signs were significantly improved or basically disappeared; SSAH reduction rate >70.0%.
Effective: The symptoms and signs were improved; SSAH reduction rate >30.0%, ≤70.0%.
Invalid: The symptoms and signs were not significantly improved; SSAH reduction rate ≤30%.
3.3 Results
3.3.1 Comparison of the clinical efficacy
The clinical efficacy was assessed after 10 treatments. The total effective rate of the Zhen’ai group was 94.3%, and that of the control group was 93.8%. There was no significant difference in the total effective rate between the two groups (P<0.05). The markedly effective rate was 42.9% in the Zhen’ai group and 12.5% in the control group. The difference in the markedly effective rate between the two groups was statistically significant (P<0.05), suggesting that the efficacy of the Zhen’ai group was superior to that of the control group (Table 2).

Table 2. Comparison of clinical efficacy between the two groups (case)
3.3.2 Comparison of the TNSS score
There was no significant difference in the TNSS score between the two groups before treatment (P>0.05), indicating that the two groups were comparable. After 10 treatments, the TNSS scores of the two groups both decreased obviously. The intra-group differences were statistically significant (bothP<0.05). The TNSS score in the Zhen’ai group was lower than that in the control group, but there was no significant difference between the two groups (P>0.05), indicating that both methods could improve clinical symptoms of AR (Table 3).
Table 3. Comparison of the TNSS score between the two groups before and after treatment (±s, point)
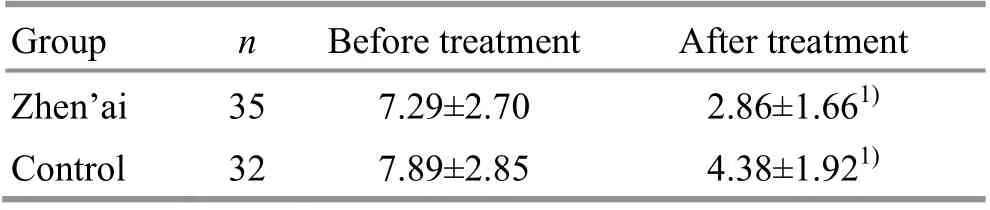
Table 3. Comparison of the TNSS score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05
Group n Before treatment After treatment Zhen’ai 35 7.29±2.70 2.86±1.661) Control 32 7.89±2.85 4.38±1.921)
3.3.3 Comparison of the SNOT-20 score
There was no significant difference in the SNOT-20 score between the two groups before treatment (P>0.05), indicating that the two groups were comparable. After 10 treatments, the SNOT-20 scores of the two groups both decreased obviously. The intra-group differences were statistically significant (bothP<0.05). The SNOT-20 score in the Zhen’ai group was lower than that in the control group, and the difference between the two groups was statistically significant (P<0.05), indicating that both methods could improve the nasal and paranasal sinus symptoms of children with AR, and the effect of the Zhen’ai group was superior to that of the control group (Table 4).
3.3.4 Comparison of the SSAH score
There was no significant difference in the SSAH score between the two groups before treatment (P>0.05), indicating that the two groups were comparable. After 10 treatments, the SSAH scores of both groups decreased obviously. The intra-group difference of the Zhen’ai group was statistically significant (P<0.05), while there was no intra-group difference in the control group (P>0.05). The SSAH score in the Zhen’ai group was lower than that in the control group, and the difference between the two groups was statistically significant (P<0.05), indicating that the effect in improving AH symptoms of the Zhen’ai group was superior to that of the control group (Table 5).
Table 4. Comparison of the SNOT-20 score between the two groups before and after treatment (±s, point)
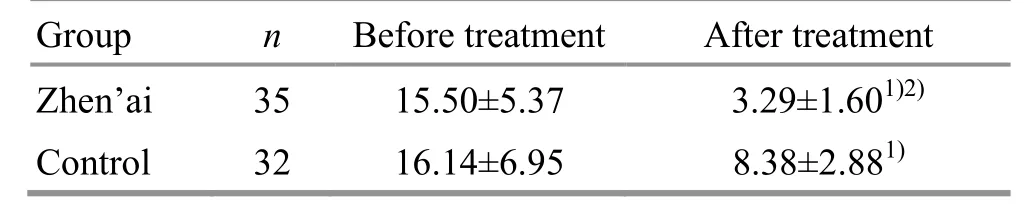
Table 4. Comparison of the SNOT-20 score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Zhen’ai 35 15.50±5.37 3.29±1.601)2) Control 32 16.14±6.95 8.38±2.881)
Table 5. Comparison of the SSAH score between the two groups before and after treatment (±s, point)
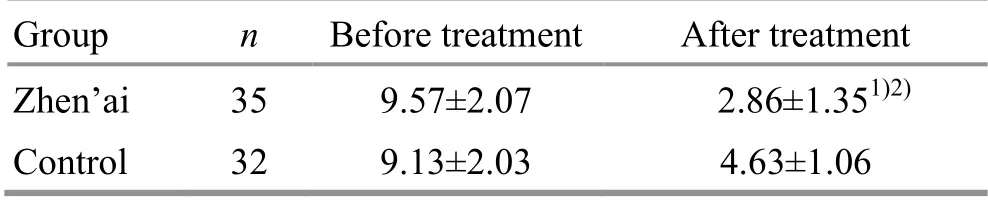
Table 5. Comparison of the SSAH score between the two groups before and after treatment (±s, point)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Before treatment After treatment Zhen’ai 35 9.57±2.07 2.86±1.351)2) Control 32 9.13±2.03 4.63±1.06
4 Discussion
Modern research believes that the indications of Zhen’ai needling method described inCijie Zhenxie of Ling Shu (the 75th Chapter ofSpiritual Pivot) are similar to allergic asthma and acute attack of asthmatic bronchitis in modern medicine[20]. In patients with AR, symptoms such as runny nose and nasal congestion after inhaling allergens like dust and smoke, and dyspnea, being unable to lie down and aggravation by inhalation of smoke in severe cases, are very similar to indications described in Zhen’ai needling method. Therefore, Zhen’ai needling method [acupuncture at Lianquan (CV 23) and Tianrong (SI 17)] can treat wheezing and rhinitis caused by allergens such as dust[21].
AR belongs to Bi Qiu (allergic rhinitis), Qiu Ti (sneezing) and Qiu Shui (runny nose) in traditional Chinese medicine. Its pathogenesis, syndrome differentiation and treatment methods have been discussed by physicians of each generation. The specific points for the treatment of nasal diseases also have been mentioned a lot in acupuncture verses[22]. In this study, Hegu (LI 4) was applied in the control group. It is the Yuan-Primary point of the Large Intestine Meridian, with quite good effect of dispersing wind-cold pathogens. It is the key point for treating diseases of head and face. Yintang (GV 29) is on the Governor Vessel. The Governor Vessel is the sea of yang meridians. Acupuncture at Yintang (GV 29) can inspire yang qi of the Governor Vessel, and the Governor Vessel passes through the nose. According to the theory that ‘an point can treat the disorders where its meridian distributes’, the selection of Yintang (GV 29) for AR complies with the principles of point-selection along meridian, local point selection and point-selection based on syndrome differentiation. Its therapeutic effect of for AR is reliable[23]. Shangxing (GV 23) can clear the nasal passage. Baihui (GV 20) is where the meridian qi and blood gather. It can raise yang and benefit qi, open the orifices and resuscitate[24]. Zusanli (ST 36) is the key acupoint for health care, having the effect of enhancing the body immunity. The selection of the above points was to combine the local points and distant points, for reinforcing the healthy qi and eliminating the pathogenic factors simultaneously. The therapeutic effect for AR was certain[11].
AH belongs to Ru E (tonsillitis), Han syndrome (snoring), and Tan He (phlegm node) in traditional Chinese medicine. It is a syndrome of healthy qi deficiency and pathogenic qi excess. Congenital insufficiency in children and deficiency of vital qi are the fundamental condition for the formation and development of the disease. The deficiency of vital qi is mostly due to the deficiency of lung qi and spleen qi. The deficiency of lung qi and the weak defense-exterior make children easily affected by exogenous pathogens. Spleen insufficiency is common in children, and the deficiency of spleen causes dysfunction of transportation and transformation, and intermingled phlegm and turbidity. Therefore, the external causes of AH are exogenous pathogens invading the lung, and the internal causes are the insufficiency of lung and spleen, intermingled phlegm and stasis. Children are delicate in Zang-fu organs and insufficient in the shape and qi, easily repeatedly affected by exogenous pathogens. If left untreated or improperly treated, pathogens stay at the junction of the nasopharynx, the phlegm and qi gather, the disease invading collaterals, then qi stagnation and blood stasis and intermingled phlegm and blood stasis will result in stubborn disease[25]. In the additional points in the Zhen’ai group, Tianrong (SI 17) has the effect of opening orifices to eliminate stagnation, regulating qi and directing qi downward[26], thus often used in the treatment of pharynx and larynx diseases[27-30]. Shanglianquan [Extra, located at 1 cun above Lianquan (CV 23)] has the effect of directing qi downward, benefiting throat and tongue, opening orifices and relieving swelling and pain. It is often used to treat cough, asthma, throat impediment, and sudden loss of voice[31-32]. These two points are points of Zhen’ai needling method. In this study, we added Lieque (LU 7). It is the Luo-Connecting point of the Lung Meridian and one of the Confluent Points of the Eight Extraordinary Meridians, communicating with the Conception Vessel. It has the effect of dispersing wind to eliminate the exterior pathogens, suppressing cough to calm panting, and directing qi downward for benefiting throat. The Zhen’ai group added these three points in addition to the points used in the control group, bringing significant improvement in throat symptoms in children with AH, which was reflected by the SSAH score.
According to the theory of traditional Chinese medicine, the incidence of Bi Qiu (AR) and Han syndrome (snoring) are related to the deficiency of lung, spleen and kidney, and the attack of external pathogenic wind-cold. Back-Shu points are the points where the qi of the Zang-fu organs are infused into the waist and the back. They are all located on the first lateral line of the Bladder Meridian on the back. In addition to treating the corresponding diseases of Zang-fu organs, they can also treat the diseases of the five sense organs related to the Zang-fu organs. Cupping along the Governor Vessel and the Bladder Meridian on the back can provoke yang qi of the body and visceral functions, and can fortify the spleen, lung, and kidney. The warm stimulation and negative pressure effect of cupping therapy cause local vasodilatation, increase of blood flow, acceleration of metabolism, and activate the immune system, thereby enhancing the disease resistance of the body[33-34].
The following three aspects were discovered during the study: One was that children with AR accompanied by AH were generally overweight, and the tongue body was also swollen. Some children had halitosis, suggesting that the function of the digestive system was abnormal. The halitosis disappeared after acupuncture for 2-3 times in both groups, suggesting that acupuncture could effectively improve the digestive function of the children. The other finding was that symptoms were relieved in the invalid cases during the treatment, but all relapsed due to overeating cold drinks or sweets. Therefore, it is recommended that parents of children with AR accompanied by AH must help the children stay away from cold drinks and sweets. The third finding was that most of the children with AR accompanied by AH were cared for by grandparents, who were too fond of the children. The children generally wore more clothes, and their constitutions were comparatively weak. Therefore, it is recommended that parents should care more about the children, not to put on too much clothes for the children, and let them exercise more to strengthen the constitution and control the weight[35].
In summary, the results of this study suggested that conventional point selection plus points of Zhen’ai needling method could improve the clinical symptoms of children with AR accompanied by AH, and its efficacy was better than that of conventional point selection. However, there were some limitations in this study. Firstly, we only observed the short-term efficacy after 2 courses of treatment, not the long-term efficacy. Secondly, due to the limitation of the study conditions, objective test results such as serum IgE and X-ray radiography could not be selected as the observation items to further clarify the mechanism of acupuncture for AR accompanied by AH[36]. We will consider studies with large-sample, long-term efficacy and objective observation indicators, so as to evaluate the clinical efficacy of conventional points selection plus points of Zhen’ai needling method for AR accompanied by AH more objectively.
Conflict of Interest
The authors declare that there is no potential conflict of interest in this article.
Acknowledgments
This work was supported by The Three-year Development Project for Traditional Chinese Medicine of Shanghai [上海市进一步加快中医药事业发展三年行动计划项目(2018 年-2020 年), No. ZY(2018-2020)-ZYJS- 43]; Shanghai Municipal Health and Family Planning Commission Research Project (上海市卫生和计划生育委员会科研课题, No. 201540150); Guidance Project of Traditional Chinese Medicine of Shanghai Science and Technology Committee (上海市科学技术委员会科研计划中医引导类项目, No. 17401932200).
Statement of Informed Consent
Informed consent was obtained from the guardians of the recruited children in this study.
Received: 19 September 2019/Accepted: 24 October 2019
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation of tuina manipulations for tic disorders in kids
- Clinical observation on muscle regions of meridians needling method in improving upper limb function for children with cerebral palsy of spastic hemiplegia type
- Electronic moxibustion apparatus and traditional moxibustion in treating knee osteoarthritis: a randomized controlled trial
- Clinical observation on filiform fire-needling plus continuous passive motion therapy for frozen shoulder
- Clinical study on auricular point sticking plus Western medicine for moderate gastric cancer pain
- Therapeutic efficacy of moxibustion plus medicine in the treatment of infertility due to polycystic ovary syndrome and its effect on serum immune inflammatory factors