Uniportal video assisted thoracoscopic left upper bronchial sleeve lobectomy in a pediatric patient
2020-08-02FirasAbuAkarBisanneShaqquraNisreenRummanKonstantinosMariosSoultanis
Firas Abu Akar, Bisanne Shaqqura, Nisreen Rumman, Konstantinos Marios Soultanis
1Department of Cardiothoracic Surgery, Makassed Charitable Society Hospital, East Jerusalem, Palestine.
2Department of Pediatrics, Makassed Charitable Society Hospital, East Jerusalem, Palestine.
3Department of Thoracic Surgery, 251 Hellenic Airforce General Hospital, Athens 11525, Greece.
Abstract Endo-bronchial tumors are sporadic in the pediatric population. Pneumonectomy is rarely indicated and best to be avoided if possible due to the morbidity it may cause. In children, preserving as much of the lung parenchymal tissue as possible is crucial and maintaining the integrity of the "still maturing" chest wall may reduce the risk of developing scoliosis and chest deformities in the future. The integration of minimally invasive surgical techniques and parenchymal sparing procedures rep-resents the best possible outcome for these patients. Of course,oncological principles should be re-spected when such a procedure is performed. We present the first report in the literature of a "left" upper lobe sleeve resection in an 8 year old patient via a single port video-assisted thoracoscopic surgery technique.
Keywords: Uniportal video-assisted thoracoscopic surgery in pediatrics, minimally invasive thoracic surgery in children, video-assisted thoracoscopic surgery sleeve lobectomy in pediatrics, pediatric thoracic surgery, bronchial carcinoid tumour in pediatrics, uniportal video-assisted thoracoscopic surgery sleeve lobectomy
INTRODUCTION
Thoracic surgery has recently undergone significant transformation and evolution. The traditional (open)thoracotomy has started to lose its popularity and thoracoscopic surgeries have started to gain interest amongst most surgeons. This is largely because of the benefits in reducing the proportion of postoperative

Figure 1. Bronchoscopic image showing a pedunculated mass occluding the left main stem bronchus
complications and an earlier return to normal life. Uniportal video-assisted thoracoscopic surgery(VATS) is the latest development in thoracoscopic surgery[1]. Aたer a decade of developing and adapting thoracoscopic surgery to a variety of thoracic conditions, it has now become possible to perform the most complex procedures through this technique, especially in adults[2-4]. However, this is still rarely utilized in children due to the difficulty of instrumentation and the lack of experience. Neuroendocrine tumours compose a small percentage of lung tumors not exceeding 2% of the general population. Neuroendocrine tumors however, are considered the most common airway malignancy in children[5]. It is well-known and generally accepted that surgical resection is the ideal solution in these cases[5]. The rarity of these tumors usually results in a significant delay in their diagnosis and treatment, as it may be treated for a long time as a chronic infection or foreign bodies in the respiratory tract[6]. Since the first bronchial sleeve operation was performed in the 1940s[7], these operations have evolved to become the preferred procedure to avoid pneumonectomies[8], and have recently been performed via the uniportal VATS technique with excellent results[3,4]. Except in one case by Gonzalez-Rivaset al.[9], these operations have not been performed previously with the uniportal VATS technique. In his article, Gonzalez-Rivaset al.[9]performed a right upper sleeve lobectomy and tracheoplasty in a 10-year-old child for a carcinoid tumor in the right main bronchus. In the current study, we report the second successful case of bronchial sleeve resection in a child through the uniportal VATS technique in the literature, and the first to be performed on the left main bronchus in an 8-year-old child with satisfactory results.
CASE PRESENTATION
A previously healthy 8-year-old female patient with a six-month history of fever and recurrent chest infections showed only partial improvement with antibiotics. A bronchoscopy was performed to rule out the presence of a foreign body, and to obtain samples for microbiology. A highly vascularised endobronchial mass arising from the leた main bronchus and occluding the bronchus to the upper lobe was found [Figure 1]. Transbronchial biopsy and bronchoalveolar lavage were performed. Pathological findings revealed a typical carcinoid tumor and cultures grewPseudomonas aeruginosa. i.v. antibiotics were given according to culture sensitivities and a 68Ga DOTATATE PET-CT was performed to exclude mediastinal and extrathoracic findings [Figure 2]. The case was discussed at the multidisciplinary team meeting and surgery was recommended. To avoid pneumonectomy at this young age, a bronchial sleeve resection was considered. Based on our experience in uniportal VATS operations in adults at a specialized and ultrahigh volume tertiary center[10], and aたer gaining further experience in paediatric patients[11], we decided to perform the surgery via the uniportal VATS technique to reduce the risk of complications and surgical trauma.
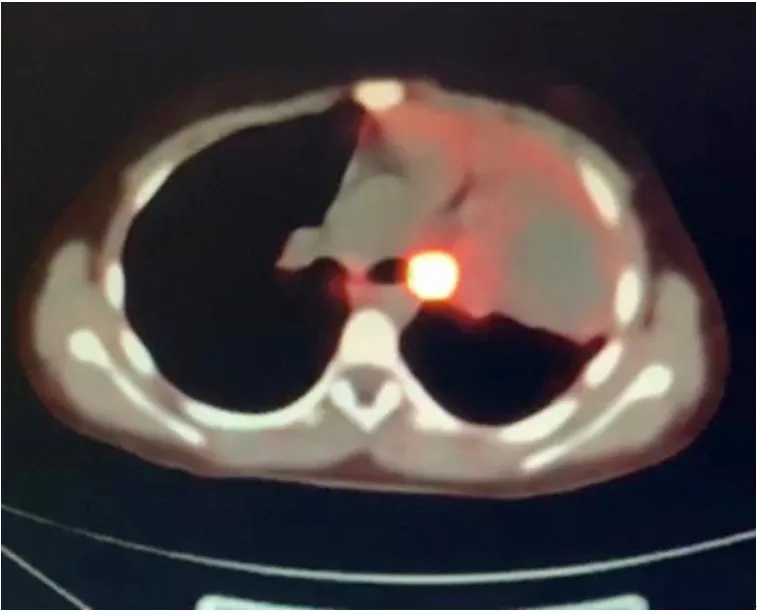
Figure 2. 68Ga DOTATATE PET-CT shows high uptake in a left main bronchus mass

Figure 3. Right decubitus positioning of the patient
Surgical technique
Once under general anesthesia, isolated right lung ventilation was maintained with a 26 Fr “right” double lumen endotracheal tube. The patient was positioned in the right decubitus position [Figure 3]. The uniportal VATS approach required a 3-cm incision at the 5th intercostal space, along the anterior axillary line. A high definition thoracoscope with 30°/10 mm lens was inserted through the incision. Exploration of the pleural cavity revealed severe adhesions, probably due to recurrent chest infections. Aたer adhesiolysis,a left upper bronchial sleeve lobectomy was performed. First, the left superior pulmonary vein was dissected free, encircled and then divided using Endo-GIA Stapler vascular reload (Endo GIATMCurved Tip Reload with Tri-StapleTMTechnology). Aたer that, branches of the pulmonary artery to the upper lobe were divided individually aたer tying with 0 silk thread or double clipped with polymer clips Click’aV PlusTMuntil the artery was completely separated from the upper lobe [Video 1]. The leた main and leた lower lobe bronchus were freed circumferentially by scalpel and surgical scissors before the lobe was retrieved inside a protecting bag. Frozen section confirmed disease-free margins. The inferior pulmonary ligament was divided, and the leた main pulmonary artery was retracted laterally using 0 silk stitch encircled around the artery and fixed to the chest wall [Figure 4], to both avoid tension and facilitate the subsequent anastomosis respectively. The leた lower lobe and leた main bronchus were anastomosed end to end using a continuous PDS 4/0 double needled suture, starting from the medial aspect of the bronchus and ending by tying the suture at the lateral corner of the anastomosis [Video 1]. Upon completion of the anastomosis, an air-leak test was done and inflation of the lower lobe was ensured. Aたer adequate hemostasis, a single 20 Fr chest tube was inserted through the same incision and the wound was closed in layers in standard fashion. The patient was successfully extubated and transferred stable to the pediatric ICU. The post-operative course was uneventful otherwise and the patient was stepped down to the ward 24 h post-surgery. Postoperative chest X-ray showed good expansion of the leた lower lobe [Figure 5]. The chest tube was removed on postoperative day 5, and the patient was discharged home on post-operative day 6 in an excellent condition.Follow-up bronchoscopy (at 1 and 6 months after the procedure) revealed intact anastomoses with no evidence of stenosis. At 9 months’ follow-up, the patient is asymptomatic and does not have any complaints.
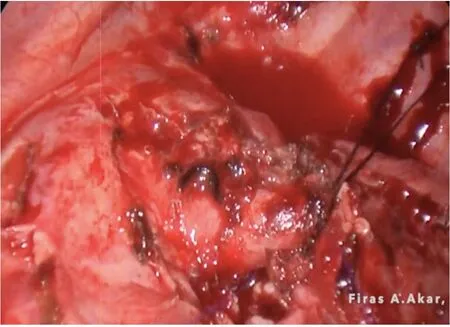
Figure 4. Intraoperative image showing the way of retracting the left main pulmonary artery to improve exposure of the bronchus
DISCUSSION
Sleeve bronchial resection procedures are usually performed in adults to avoid pneumonectomy and associated morbidity. These operations are conducted in cases of central or endo-bronchial tumours. In children, bronchial sleeve resections are extremely uncommon and rarely indicated due to the paucity of lung malignancies in the pediatric population in general, especially endobronchial tumors. A review of the literature only yielded one case of a bronchial sleeve operation performed via the uniportal VATS technique in a 10-year-old child who had a carcinoid tumour in the right main bronchus[9]; there were otherwise only a few reports on pediatric sleeve resection through the traditional open thoracotomy approach[9,12]. It is well known that VATS can significantly reduce complications and surgical trauma, contribute to earlier recovery and expedite the return to normal life for patients[13].
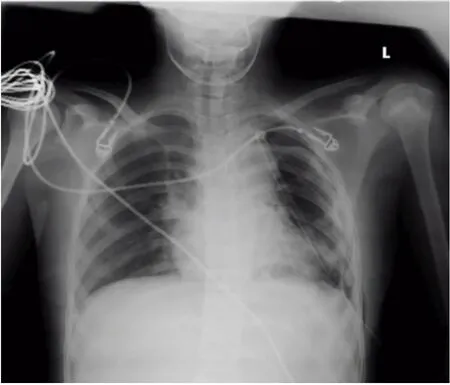
Figure 5. Postoperative chest X-Ray showing good inflation of the lung with no abnormalities
There are additional benefits of thoracoscopic surgery, especially in children, such as the avoidance of scoliosis and preventing breast asymmetry in females due to the damage that may occur in chest wall muscles from traditional open thoracotomy[14-16]. Therefore, the thoracoscopic approach to these pediatric cases is much more desirable and should be strongly encouraged. There are still some obstacles that may limit the applicability of this technique in children however, with the learning curve being particularly steep. The operative field available in the child’s pleural space is limited, which can lead to extreme challenges with instrumentation. Another difficulty that one may face during surgery is the complexity of lung isolation due to the unavailability of the double-lumen tube for all ages, which poses a challenge to the surgeon and anesthesiologist. This is on top of the lack of instruments specially designed for pediatrics. We usually use traditional instruments to perform uniportal VATS in infants[11], or those designed for adults in older children.
In conclusion, we strongly believe in the value and benefits of uniportal VATS surgery, especially in pediatric patients. Complex operations via the uniportal VATS approach as described is feasible in children. However, experience in uniportal VATS is necessary, and these operations must be performed in specialized and high-volume centers that contain all the necessary facilities. There is a need to develop specialized equipment specific for children for such operations to make it more manageable.
DECLARATIONS
Authors’ contributions
Conception and design of the study, and performed data analysis and interpretation: Abu Akar F, Shaqqura B
Performed data acquisition, as well as provided administrative, technical, and material support: Abu Akar F,Rumman N, Soultanis KM
Availability of date and materials
The authors declared that all data that support our findings can be found in our database and archive at Al-Makassed Hospital. Data can be deposited into data repositories or published as supplementary information in the journal.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Ethical approval and consent was obtained from the patient’s parents to publish the article.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
杂志排行
Mini-invasive Surgery的其它文章
- Cause of recurrent laryngeal nerve paralysis following esophageal cancer surgery and preventive surgical technique along the left recurrent laryngeal nerve
- Mediastinoscopic esophagectomy with lymph node dissection using a bilateral transcervical and transhiatal pneumomediastinal approach
- Current management of gastroesophageal reflux disease in the obese population - a review of the literature
- MlS Al - artificial intelligence application in minimally invasive surgery
- From TATA to single port robotic (SPr) taTME:approaches to distal rectal cancer
- Endoscopic-assisted lCG (EASl) technique for sentinel lymph node biopsy in breast cancer