Technical details of laparoscopic sleeve gastrectomy
2020-07-30TalarVartanogluAktokmakyanOzgunGungorAzizSumer
Talar Vartanoglu Aktokmakyan, Ozgun Gungor, Aziz Sumer
1Department of General Surgery, Istanbul Bagcilar Training and Research Hospital, Istanbul 34000, Turkey.
2Department of General Surgery, Memorial Hospital, Antalya 07000, Turkey.
3Department of General Surgery, Gaziosmanpasa Medicalpark Hospital, Faculty of Medicine, Istinye University, Istanbul 34000, Turkey.
Abstract
Keywords: Bariatric Surgery, obesity, sleeve gastrectomy, technique
INTRODUCTION
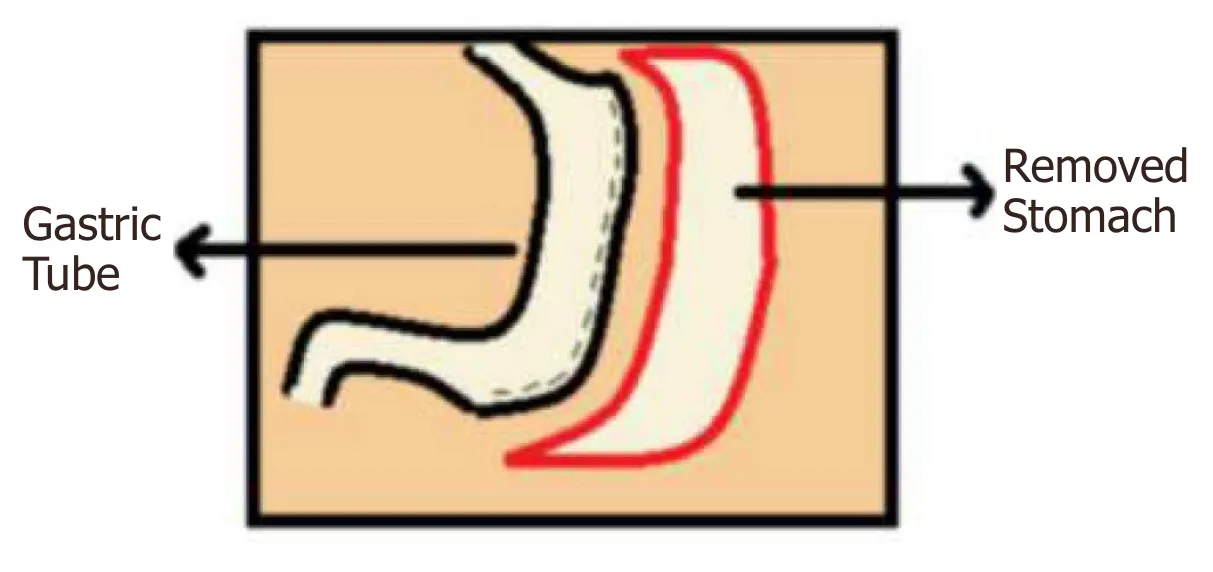
Figure 1.Demonstration of sleeve gastrectomy
Obesity is an expanding threat to the health of populations around the world.According to the National Health and Nutrition Examination Survey, the incidence of obesity was 39.8% in adults and 18.5% in youth in the United States between 2015 and 2016[1].Several endoscopic and surgical procedures have been advanced to achieve the best outcomes in obesity.Sleeve gastrectomy was first performed in 1990 as the first of a two-stage operation for biliopancreatic diversion with duodenal switch (BPD-DS)[2].Then, the first Laparoscopic Sleeve Gastrectomy (LSG) was applied in 1999.The original indication for sleeve gastrectomy was to initiate weight loss in super-obese patients [body mass index (BMI) > 60] to safely enter the second stage, BPD-DS.When these patients were followed, the excellent decrease in excess body weights was found, and in 2008 these findings were published with indications for LSG[3].When compared to other bariatric surgeries, sleeve gastrectomy is technically easier with relatively less morbidity and thus has become a commonly performed bariatric surgery as an obesity control modality.LSG has become the most common bariatric surgical procedure in recent years, and its short-term results have been reported to be effective and safe.ASMBS (American Society for Metabolic and Bariatric Surgery) considers sleeve gastrectomy (SG) to be an acceptable option for the primary bariatric procedure or as a first-stage procedure in high-risk patients.However, its effectiveness and long-term consequences are still being discussed[4,5].
LSG is a restrictive bariatric technique consisting of subtotal partial vertical gastrectomy with the preservation of the pylorus.A gastric tube is created as a continuation of the esophagus along the lesser curvature with the resection of the fundus, corpus, and antrum [Figure 1].Although LSG is claimed as a restrictive procedure, it has neuro-humoral effects that stimulate recovery in weight loss and concomitant diseases.Moreover, SG induces fast gastric emptying and causes early food transportation into the small bowel[6].Despite the established safety and efficacy of LSG, controversy still exists on optimal operative techniques.This review aims to present the LSG technique with controversial aspects in the light of our clinical experience and skills as a technical note.
SURGICAL TECHNIQUES
The operation is performed in reverse Trendelenburg position on an operating table with an angle of 30° and the surgeon takes position between the legs of the patient.Pneumo-peritoneum is performed with the Veress needle in the left upper quadrant.The five-trocar technique is used.The first (10-mm) trocar is placed at the upper abdomen 1-2 cm above the umbilicus as an optical trocar.A 5-mm trocar is inserted at the sub-xiphoid area for the Nathanson liver retractor [Figure 2].A 15-mm trocar is introduced at the right upper quadrant and a 12-mm trocar is inserted at the left upper quadrant.Finally, a 5-mm trocar is introduced at the left subcostal anterior axillary line.
Firstly, the stomach is decompressed via a nasogastric tube by the anesthesiologist.Then, the omentum is released and ligated from the greater gastric curvature with the energy-based device continuing proximally into the esophagus and 2-4 cm proximal to the pylorus [Figure 3].
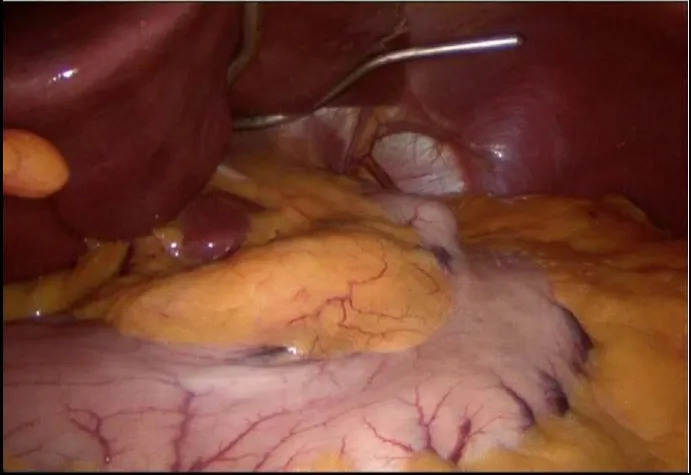
Figure 2.Retracted liver

Figure 3.Release and ligation of the omentum
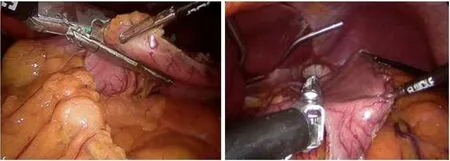
Figure 4.Insertion of first and second staplers from the 15-mm trocar
After the dissection of the greater curvature, a calibrating bougie (36F) is placed at the stomach and passed through the pylorus by the anesthesiologist.The first and second linear staplers are placed from the 15-mm trocar at the right upper quadrant to divide the stomach [Figure 4].To avoid the narrowing at the incisura angularis, the first stapler is adjusted parallel to the pylorus.The first fired stapler and traction from the left trocar is very important to ensure a straight stapler line.
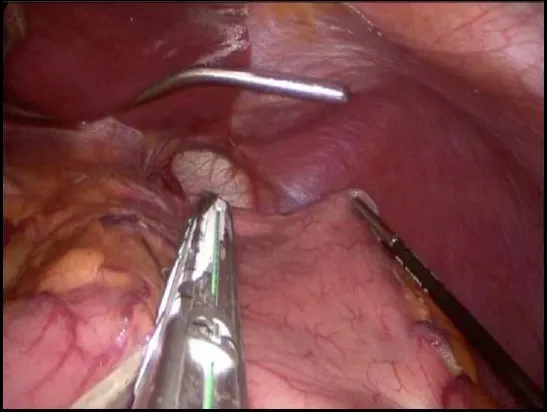
Figure 5.The stapler fired cranially
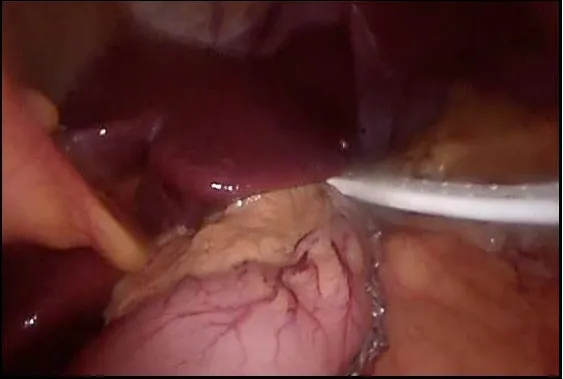
Figure 6.The gastric tube and the drain
The remaining staplers are fired in cranially along the greater curvature of the stomach [Figure 5].While black or green cartridges are applied to the first two firings, blue or purple cartridges are applied to the remaining part according to the thickness of the stomach.For transection, approximately 5-7 staplers are necessary to complete the transaction.During the transaction, clips are applied only to the staple joints and bleeding foci.Otherwise, no staple line reinforcement technique is used.If the twist is suspected, omentoplasty can be performed from three points as the antrum, incisura angularis, and its superior via suturing one by one.Methylene blue test is routinely applied to test for leakage.The resected stomach is removed from the left quadrant via a 12-mm trocar and a drain is placed from the right quadrant from a 15-mm trocar near the staple line [Figure 6].All incisions are sutured after removing all trocars.
RESULTS
Patients are hospitalized approximately 2-4 days.On Postoperative Day 2, methylene blue test is done for leakage.According to the negative test, the regimen is started with water, tea, and soup.After adequate tolerance of oral fluids, the patient is discharged after the drainage catheter is removed.For the first two weeks, juicy foods are recommended; in the following two weeks, soft foods are recommended.According to tolerance, after the first month, solid food is started with the recommendation of less and frequent eating.
DISCUSSION
The number of sleeve gastrectomy procedures performed increases annually.This is clarified by the advantages of the simpler and faster technique; no malabsorption, anastomosis, or mesenteric surgery; no foreign body being inserted; and patients rarely having symptoms of “dumping syndrome”[7].In a consensus conference in 2014, LSG was accepted as a standalone procedure that reduces appetite and creates a restriction.According to the consensus statement, LSG is a valid independent procedure and is a viable bariatric surgery option for high-risk patients, transplant candidates, and patients with lower BMI (30-35), patients with inflammatory bowel disease, and the elderly[6].
Although LSG is currently the most commonly used technique in the bariatric surgical repertoire and is even considered as a gold standard technique, technical controversies continue.However, many discussion points on the procedure create a range probability without consensus: the distance from the pylorus, the routine use of intraoperative seal testing the size of the bougie used as a calibrator, the necessity for reinforcement of the staple line, and the considerations in case of revision LSG (re-LSG) requirement.
The end of the lower dissection is argumentative because the antrum is divided at 2 or 7 cm from the pylorus, determined by the surgical team[8].Sánchez-Santoset al.[9], according to the results of the National Register of Spain, reported that they had better weight loss results in the follow-up of groups that started gastrectomy closest to the pylorus.Our reason for dissection 2-4 cm from the pylorus is to decrease the pressure in the gastric tube and allow preferable gastric emptying.It should be noted that the increase in pressure in the gastric tube is the main cause of leakages.Furthermore, gastric tube volume above and below incisura angularis and their ratio are important factors that affect weight loss.From our preliminary results published in 2018, an antrum volume of approximately one-third of the total remaining stomach volume appears to be ideal for optimal weight loss[5].Getting closer to the pylorus does not change weight loss and has a negative impact on using a non-touched antrum during revision surgery.
Another point of controversy is leak testing.The methylene blue test was initially defined to diagnose the post-gastrectomy fistulas.It is one of the most commonly used tests in bariatric surgery, consisting of oral administration of methylene blue and observation of any intraoperative outlet through the gastric tube[10].Methylene blue and/or air testing is recommended when the gastric tube is inserted into the distal esophagus and the antrum is clamped[11].There is a discrepancy between surgeons about which leak test they use, and whether it is performed[12].We apply methylene blue as a leakage test intraoperatively and on Postoperative Day 2.However, it should be kept in mind that a negative test does not warrant that there will be no postoperative complications including fistulas.
There is also the diameter of the remnant stomach in technical discussions about SG.Various evaluations have analyzed the results of surgery with different gastric tube calibration standards of more than 28-50 Fr.For example, Gagner[13]defines an inverse relationship among the size of the bougie and the rate of leaks and support the use of catheters between 50 and 60 Fr.In the Fifth International Consensus Conference, it was recommended that a large bougie should be used (median was 36 French)[14]and we also use 36 Fr.
Despite its simplicity, LSG can have serious complications.Gastric leakage is one of the most hesitated complications.Numerous maneuvers have been suggested to decrease the incidence of leak intraoperatively[15].Another discussion is in the reinforcement of the staple line.The main objectives of reinforcement of the staple line are to reduce hemorrhage rates and staple line leaks.There is no current consensus in recommendations about staple line reinforcement use.Its usage is surgeon-dependent and remains controversial[16].For instance, Bellangeret al.[3]showed a series of 529 patients who did not leak without using any reinforcing material after the gastric section except fibrin administration.In a recent meta-analysis, there was no statistically significant difference in leak ratio.Therefore, we do not prefer reinforcement methods.According to our experience with more than 1000 patients, only three leakages, three bleedings, and one stenosis were detected as complications.Two of the three leakages were detected in the patient who underwent re-sleeve as revision surgery.While percutaneous drainage and the endoscopic stent were applied to one of these two leakages, the other was treated with re-laparoscopy drainage and stent.The third case of leakage was followed conservatively.In terms of hemorrhage, two of the three bleeding cases were followed conservatively and they were discharged without any problem.Re-laparoscopy was performed when stabilization could not be achieved despite four units of blood replacement in only one bleeding case, but no bleeding focus could be detected and the bleeding had stopped.Only the hematoma was removed and the drain was replaced.
In up to 30% of cases, revision surgery is necessary for causes which include inadequate weight loss, weight re-gain, and/or the progress of severe upper gastrointestinal symptoms[17].Traditionally, conversion to DS after failed GS or more commonly to RYGB has been standard.The recently popular mini gastric bypass technique stands out in revision sleeve gastrectomies.It is important not only in revision of SG but also in revision of adjustable gastric banding[18].
However, the discovery of a possible dilation of the remnant stomach or the presence of a remaining gastric fundus led to changes in the approach of a failed LSG and the application of a re-LSG emerged with the reason of re-sizing the sleeve when the expansion is present on the imaginary modalities[19].We do not recommend LSG as a revision surgery since two of our three leakage cases developed after re-sleeve operation.When re-sleeve is applied, we try to prevent narrowing by applying separate staplers between the antrum and the incisura angularis, without touching the incisura angularis, and on the dilated stomach.
CONCLUSION
We describe the tips and tricks for the sleeve gastrectomy technique.We also discuss the controversial subjects in this technique.Further prospective large studies would help to define optimal techniques.Standardizing this surgical technique as much as possible is important so most teams work using homologous methods, as well as in view of performing systematic reviews, consensus conferences, and long-term multicenter studies.We will see in time whether the fate of sleeve gastrectomy, which has been popular for the last 20 years, will follow that of the adjustable gastric band.
DECLARATIONS
Authors’ contributions
Conception and design: Aktokmakyan TV
Administrative support: Sumer A
Provision of study materials or patients: Aktokmakyan TV, Gungor O, Sumer A
Collection and assembly of data: Aktokmakyan TV
Data analysis and interpretation: Gungor O
Manuscript writing: Aktokmakyan TV, Gungor O, Sumer A
Final approval of manuscript: Aktokmakyan TV, Gungor O, Sumer A
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
