我院肝病患者病原菌感染分布及耐药性分析
2020-07-27任建云陈琳王玥吴红章
任建云 陈琳 王玥 吴红章

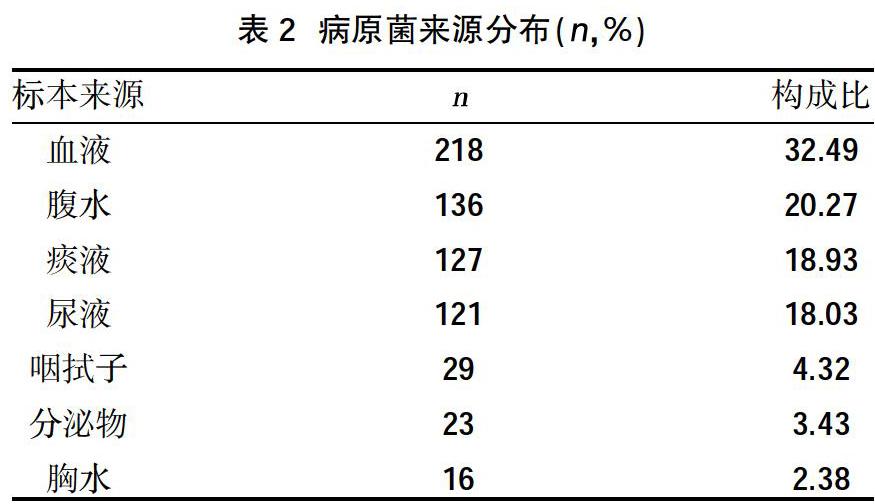
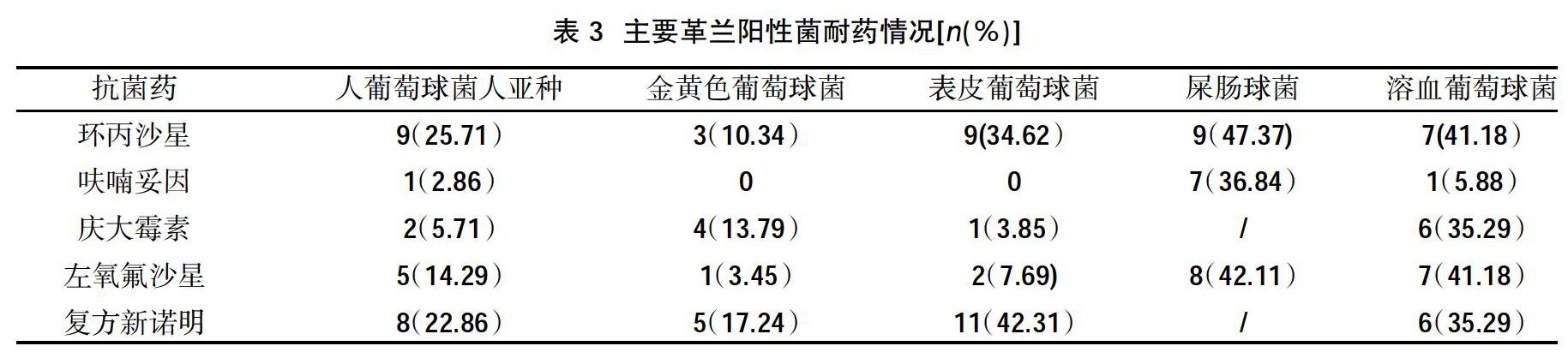
摘要:目的 探討我院肝病患者感染的病原菌类型、分布及主要细菌的耐药性,为临床合理使用抗菌药物提供理论依据。方法 回顾性分析我院2017年1月~2019年7月肝病患者送检的标本,使用VITEK-2COMPACT细菌鉴定药敏系统进行细菌鉴定、药敏试验,补充药敏试验使用纸片扩散法,统计标本中病原菌分布、来源及耐药情况。结果 共分离到非重复菌株671株,革兰阴性菌419株(62.44%),革兰阳性菌208株(30.99%),真菌44株(6.55%)。革兰阴性菌主要包括大肠埃希菌、肺炎克雷伯菌、铜绿假单胞菌、鲍曼不动杆菌、阴沟肠杆菌,检出率分别为24.14%、18.18%、3.58%、2.38%和1.94%;革兰阳性菌主要包括人葡萄球菌人亚种、金黄色葡萄球菌、表皮葡萄球菌、屎肠球菌、溶血葡萄球菌,检出率分别为5.22%、4.32%、3.87%、2.83%和2.53%;分离的菌株主要来源于血液、腹水、痰液和尿液等;大肠埃希菌与肺炎克雷伯菌对阿米卡星、头孢替坦、妥布霉素、哌拉西林/他咗巴坦、碳青霉烯类药物耐药率均低于6.79%;铜绿假单胞菌和鲍曼不动杆菌对氨基糖苷类药物、喹诺酮类抗菌药物耐药率低于6.25%,对除头孢他啶、头孢吡肟之外的其他头孢类抗生素耐药率均高于87.50%;阴沟肠杆菌耐药率均低于15.38%;葡萄球菌对替加环素、利奈唑胺与万古霉素均未发现耐药菌,对克林霉素、红霉素、苄青霉素耐药率均高于46.15%;金黄色葡萄球菌对呋喃妥因、利奈唑胺、莫西沙星、喹努普汀/达福普汀敏感;凝固酶阴性葡萄球菌对苯唑西林的耐药率高于60%;屎肠球菌抗菌药物普遍耐药。结论 肝病患者病原菌感染革兰阴性菌较多,主要为大肠埃希菌和肺炎克雷伯菌。及时分析肝病患者病原菌感染分布和耐药情况,可为临床医师合理使用抗菌药物控制院内感染提供参考依据。
关键词:肝病;病原菌;感染;耐药性
中图分类号:R446.5 文献标识码:A DOI:10.3969/j.issn.1006-1959.2020.13.038
文章编号:1006-1959(2020)13-0130-04
Analysis of Pathogenic Bacteria Infection Distribution and Drug Resistance
in Patients with Liver Disease in Our Hospital
REN Jian-yun,CHEN Lin,WANG Yue,WU Hong-zhang
(Department of Laboratory,Tianjin Second People's Hospital,Tianjin 300192,China)
Abstract:Objective To explore the types, distribution and drug resistance of pathogenic bacteria in patients with liver disease in our hospital, and to provide a theoretical basis for the rational use of antibacterial drugs in clinic.Methods Retrospective analysis of specimens from our hospital from January 2017 to July 2019 for liver disease patients, using the VITEK-2COMPACT bacterial identification drug susceptibility system for bacterial identification and drug susceptibility testing, supplementary drug susceptibility testing using paper diffusion method, statistics Pathogen distribution, source and drug resistance in specimens.Results A total of 671 non-repeated strains were isolated, 419 Gram-negative bacteria (62.44%), Gram-positive bacteria 208 (30.99%), and 44 fungi (6.55%). Gram-negative bacteria mainly include Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Acinetobacter baumannii, Enterobacter cloacae, the detection rates were 24.14%, 18.18%, 3.58%, 2.38% and 1.94%; Gram-positive bacteria mainly include human Staphylococcus aureus subspecies, Staphylococcus aureus, Staphylococcus epidermidis, Enterococcus faecium, Staphylococcus hemolyticus, the detection rates were 5.22%, 4.32%, 3.87%, 2.83% and 2.53%; isolated strains mainly come from blood, ascites, sputum and urine; Escherichia coli and Klebsiella pneumoniae against amikacin, cefotetan, tobramycin, piperacillin The resistance rates of babatan and carbapenems were lower than 6.79%; the resistance rates of Pseudomonas aeruginosa and Acinetobacter baumannii to aminoglycoside drugs and quinolone antibacterial drugs were lower than 6.25%. The resistance rates of cephalosporins and cefepime other than cephalosporins were higher than 87.50%; the resistance rates of Enterobacter cloacae were lower than 15.38%; the staphylococci were not resistant to tigecycline, linezolid and vancomycin drug-resistant bacteria were found, and the resistance rates to clindamycin, erythromycin, and benzylpenicillin were all higher than 46.15%; Staphylococcus aureus was resistant to nitrofurantoin, linezolid, moxifloxacin, quinupristin/dalfopristin sensitive; the resistance rate of coagulase-negative staphylococcus to oxacillin is higher than 60%; the antibacterial drugs of Enterococcus faecium are generally resistant.Conclusion There are many Gram-negative bacteria infected by pathogenic bacteria in patients with liver disease, mainly Escherichia coli and Klebsiella pneumoniae. Timely analysis of the distribution of pathogenic bacteria infection and drug resistance in patients with liver disease can provide a reference for clinicians to use antibacterial drugs to control nosocomial infections.
综上所述,我院肝病患者病原菌感染革兰阴性菌较多,主要为大肠埃希菌和肺炎克雷伯菌。及时分析肝病患者病原菌感染分布和耐药情况,可为临床医师合理使用抗菌药物控制院内感染提供参考依据。
参考文献:
[1]许根友.学习《全国临床检验操作规程》(第3版)第一篇对检验工作的实际意义[J].临床血液学杂志(输血与检验版),2010,23(6):759-760.
[2]杜方兵,吕志,杨万春.成人下呼吸道感染病原菌群的分布与耐药性研究[J].临床肺科杂志,2018,23(5):840-843.
[3]何卫平,崔恩博,卜昕,等.2012年度某传染病专科医院感染细菌分布及耐药性分析[J].传染病信息,2014,27(1):45-48.
[4]刘文静,徐英春,杨启文,等.2018年北京协和医院细菌耐药性监测[J].中国感染与化疗杂志,2019,19(6):639-646.
[5]李芳,李雅丽,雷金娥,等.我院中心ICU感染病原菌的分布及耐药性分析[J].西北药学杂志,2019,34(1):116-121.
[6]Richter SE,Miller L,Uslan DZ,et al.Risk Factors for Colistin Resistance among Gram-Negative Rods and Klebsiella pneumoniae Isolates[J].Journal of Clinical Microbiology,2018,56(9):e00149.
[7]Zheng J,Lin Z,Sun X,et al.Overexpression of OqxAB and MacAB efflux pumps contributes to eravacycline resistance and heteroresistance in clinical isolates ofKlebsiella pneumoniae[J].Emerging Microbes&Infections,2019,7(1):1-11.
[8]Pfaller MA,Flamm RK,Duncan LR,et al.Ceftobiprole activity when tested against contemporary bacteria causing bloodstream infections in the United States(2016-2017)[J].Diagn Microbiol Infect Dis,2019,94(3):304-313.
[9]Dowzicky MJ,Chmelarova E.Antimicrobial susceptibility of Gram-negative and Gram-positive bacteria collected from Eastern Europe:Results from the Tigecycline Evaluation and Surveillance Trial(T.E.S.T.)2011-2016[J].J Glob Antimicrob Resist,2019(17):44-52.
[10]杨朕.天津北部地区2977份临床标本细菌分布及耐药性分析[J].中国处方药,2019,17(4):117-118.
[11]陈春辉,郭燕,吴湜,等.替加环素、米诺环素对VanM型万古霉素耐药屎肠球菌体外抗菌活性[J].中国感染与化疗杂志,2016,16(3):327-329.
[12]于汉卿.2017-2018年南京市儿童医院儿科重症监护病房感染病原菌的分布及耐药性分析[J].现代药物与临床,2019, 34(11):3475-3480.
[13]俞云松.我国革兰阴性菌耐药态势及其机制[J].中华结核和呼吸杂志,2017,40(8):573-577.
[14]王健,潘亚萍,徐元宏,等.耐碳青霉烯类肺炎克雷伯菌药物敏感性和耐药基因研究[J].安徽医科大学学报,2018,53(8):1231-1235.
[15]王黎一,曹旭华,史利克,等.下呼吸道鲍曼不动杆菌感染患者对亚胺培南、美罗培南和头孢哌酮舒巴坦耐药的易感因素分析[J].河北医科大学学报,2019,40(3):332-338.
[16]周鹏鹏,员静,季萍.新疆地区多重耐药鲍曼不动杆菌耐药及分布特点[J].中国抗生素杂志,2019,44(6):732-735.
[17]刘红栓,蔡阳平,张庆, 等.重症监护室鲍曼不动杆菌感染的临床现状及耐藥性变迁[J].河北医学,2019,25(5):779-782.
收稿日期:2020-04-09;修回日期:2020-04-19
编辑/王朵梅
作者简介:任建云(1987.12-),女,天津人,硕士,检验技师,主要从事临床检验工作
