Meta-analysis of the relationship between post-stroke depression and the risk of mortality
2020-07-23YinShaoYuZhaoLiMaXinBoWang
Yin Shao, Yu Zhao, Li Ma, Xin-Bo Wang
The First Affiliated Hospital of Heilongjiang University of traditional Chinese Medicine
Keywords:
ABSTRACT
1. Introduction
Stroke is the main cause of long-term disability and the second leading cause of death in the world[1]. As one of the common complications of stroke, post stroke depression (PSD) usually presents a series of clinical symptoms such as negative emotion increase such as depression, loss of interest, mental retardation and sleep disorder [2]. The incidence rate of incidence of PSD in mainland China is about 32.8%, which is higher than the average incidence rate of PSD in the mainland (about 29%). And the incidence rate increases with year by year [3-4]. As an independent risk factor for prognosis, quality of life and recurrence of stroke, the mortality of stroke patients with depression was significantly higher than that of patients without depression [5].
Although most of the existing studies show that PSD is closely related to the risk of death after stroke, due to the differences in genetic factors, age, gender, medical and mental history, stroke type and severity, lesion location, disability, etc., the results of these studies are quite different [6-7]. Therefore, this study systematically evaluated the published cohort studies on the relationship between post-stroke depression and all-cause mortality in recent years, and explored the relationship between post-stroke depression and mortality, in order to provide a better scientific basis for evaluating the prognosis of patients with post-stroke depression.
2.Materials and methods
2.1 Literature search
The Chinese and English databases such as PubMed, Cochrane Library, EMBASE, WanFang Data, CNKI and VIP are searched by computer. The research type is queue research, and the retrieval time limit is from the establishment of the database to February 2020. Chinese databases use "post stroke depression" or "post stroke depression", "risk of death" or "all-cause mortality" as key words for retrieval; English databases use "post stroke depression" or "post stroke mood disorder", "mortality" or "all-cause mortality" as key words for retrieval.
2.2 Inclusion and exclusion criteria
2.2.1Population
Patients diagnosed as post-stroke depression according to the diagnostic criteria.
Objective:To evaluate the relationship between post-stroke depression (PSD) and the risk of mortality in post stroke patients.Methods:Cohort studies related to PSD and risk of mortality were collected by searching PubMed, Cochrane Library, EMBASE, WanFang Data, CNKI and VIP databases. The retrieval time limit was from the establishment of the database to January 2020. The meta-analysis was carried out by Using Stata software after two researchers independently selected literature, extracted data and evaluated the bias risk.Results:A total of 243826 participants were included in 12 studies. The combined results showed that PSD increased all-cause mortality in stroke patients [HR=1.51, 95% CI (1.16, 1.85), P<0.001]. Subgroup analysis also showed that PSD significantly increased all-cause mortality in stroke patients during brief-term follow-up: [HR=1.45, 95% CI (0.96, 1.93), P<0.001] and longterm follow-up: [HR=1.51, 95% CI (1.23, 1.79), P<0.001].Conclusion:PSD can significantly increase the risk of mortality in post-stroke patients. Considering the limitation of potential heterogeneity, more high-quality literature studies are needed to verify.
2.2.2 Study type
retrospective or prospective cohort study and case-control study published at home and abroad.
2.2.3 Exposure factors
The exposed group was patients with post-stroke depression; the non exposed group was patients without post-stroke depression or healthy controls.
2.2.4 Outcomes
Mortality
2.2.5 Exclusion criteria:
(1) non Chinese and English literature; (2) repeated reports; (3) literature without relevant outcome indicators; (4) literature with incomplete data and without access to the author.
2.3 Data extraction
The title and abstract of the literature were selected by two researchers (Shao Yin and Zhao Yu) and evaluated in full after being included in the standard. A researcher (Ma Li and Wang Xinbo) extracts relevant information and data from the included research. If there is any inconsistency, a third person (Zhao Yu) will participate in the discussion to reach a consensus. The data extracted from the literature include the name of the first author, the year of publication, the country of study, the type of study design, the sample size, the definition of depression, the follow-up time and outcome indicators.
2.4 Bias risk assessment
Two researchers (Shao Yin and Zhao Yu) used the NOS scale recommended by Cochrane to independently evaluate the bias risk of the accepted literature, and cross checked the results. The NOS scale consists of 8 items, with a total score of 9 points. The score≥7 points is considered as a high-quality study.
2.5 Statistical analysis
In this study, Stata 15.1 software was used for analysis. The data were expressed by risk ratio (HR) and 95% CI. The random effect model was used. The heterogeneity between the results was analyzed by χ2test (test level was α = 0.1). At the same time, the heterogeneity was quantitatively determined by combining with I2. I2 > 50% was used to indicate the existence of heterogeneity. P < 0.05 showed that the difference was statistically significant.
3. Results
3.1 Literature selection process and results
A total of 482 documents were obtained through the preliminary examination. After re screening layer by layer, the literatures repeatedly published, reviewed, summarized and unable to provide effective data were eliminated, and finally 12 documents meeting the standards were included. See Figure 1 for the literature screening process.
3.2 Characteristics of the study
A total of 12 literatures were included in this study [6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17], 243826 patients with a sample size of 257-157243, all of which were retrospective studies and followed up for 1-12 years. The basic characteristics of the included literatures are shown in Table 1. The lowest score of NOS in the study was 5, the highest score was 8, and the average score of NOS was 6.5, indicating that the overall treatment of the literature was good. See Table 2 for scores and results.
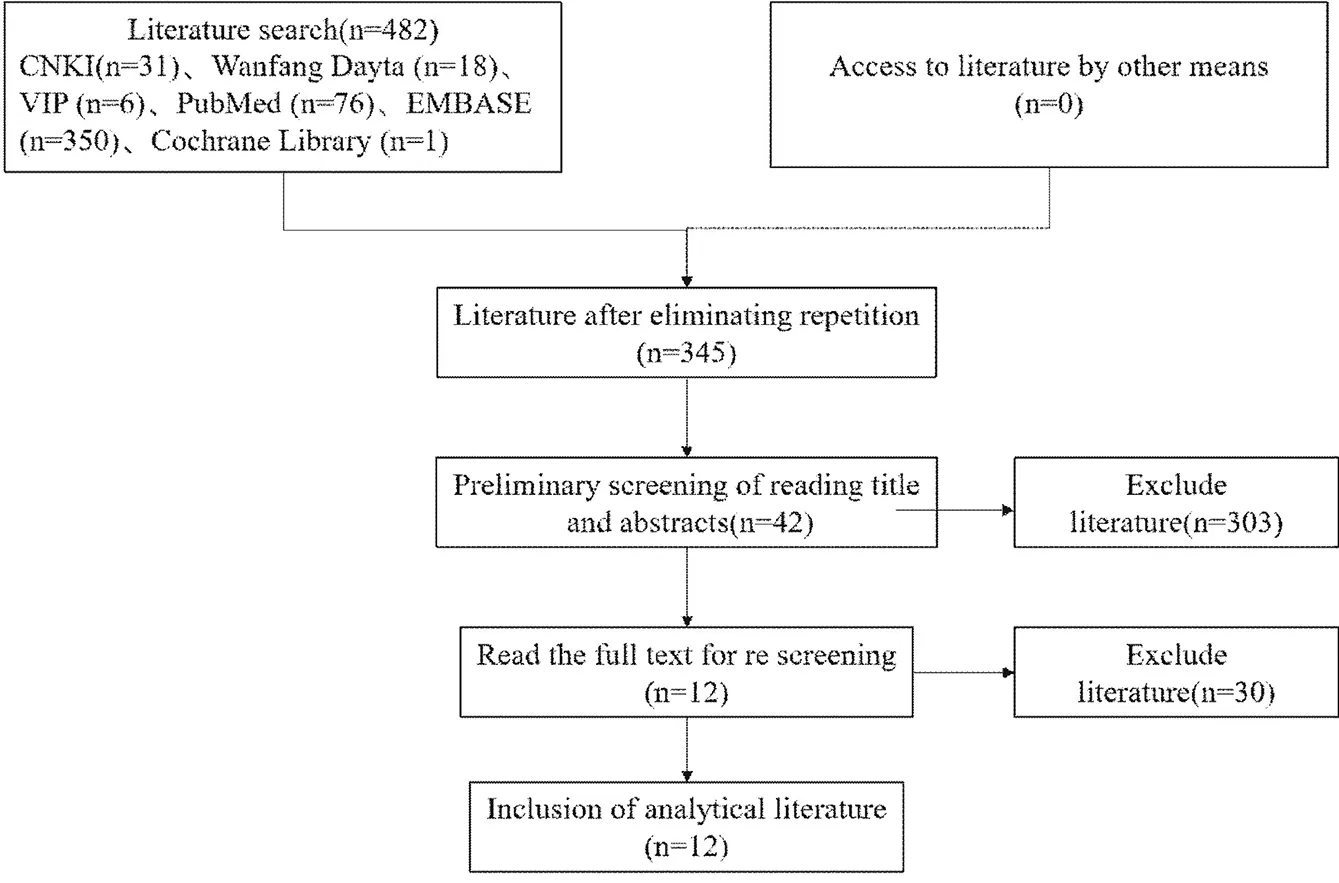
Figure 1. Flow chart of literature screening

Table 1. Basic characteristics of the study
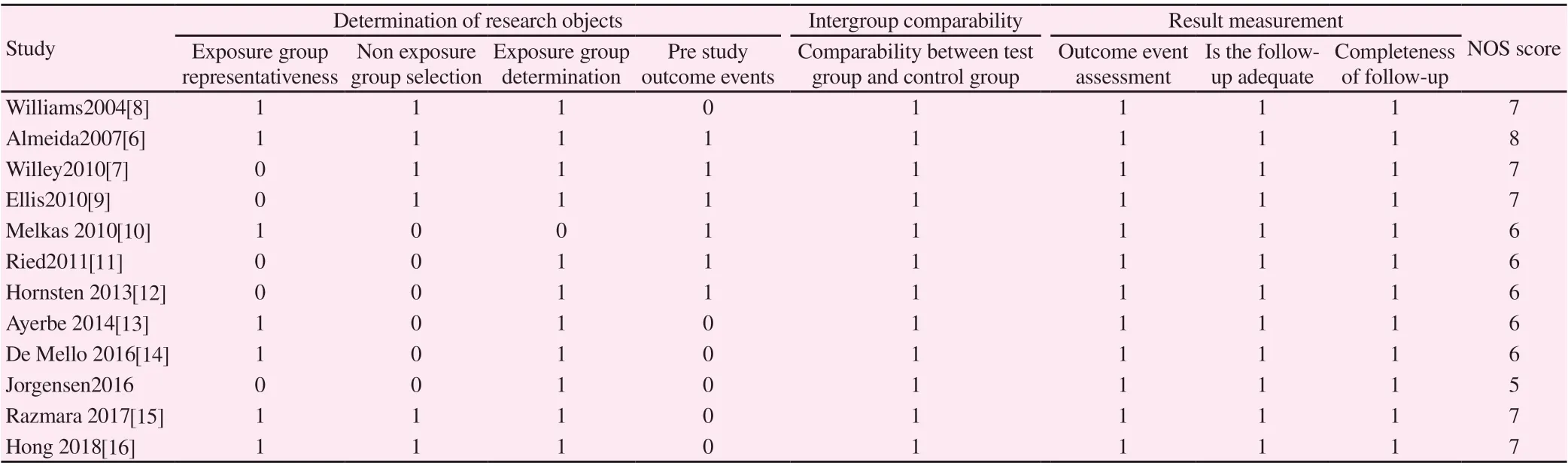
Table2. Bias risk assessment results included in the literature (points)
3.3 Meta analysis results
All 12 literatures [6,7,8,9,10,11,12,13,14,15,16,17] reported the correlation between PSD and all-cause mortality. The combined results showed that PSD and all-cause mortality of stroke patients showed significant positive correlation: [HR = 1.51, 95% CI (1.16, 1.85), P < 0.001; I2 = 98%, P < 0.001]. Due to the significant heterogeneity of the included studies, we conducted a subgroup analysis based on the follow-up time of the included literature. Subgroup analysis showed that PSD at short-term follow-up (follow-up time ≤ 5 years) and longterm follow-up (follow-up time > 5 years) were positively correlated with all-cause mortality of stroke patients. Short term follow-up: [HR = 1.45, 95% CI (0.96, 1.93), P < 0.001; I2 = 98%, P < 0.001]; long term follow-up: [HR = 1.51, 95% CI (1.23, 1.79), P<0.001; I2=0%, P=0.676]. See Figure 2.

Figure 2. HR forest map of post stroke depression mortality. Note: short term follow up (< 5 years) and long term follow up (> 5 years)
3.3 Publication bias
According to the length of follow-up time and all-cause mortality outcome index of PSD patients, funnel chart was drawn, and the distribution of each research point was basically symmetrical. The publication bias was detected by Begg's and egger's tests. The results showed that there was no publication bias in the included literature (P = 0.425 and P = 0.396). See Figure 3-5

Figure 3. Funnel chart of literature publication bias.

Figure 4. Begg's test of literature publication bias
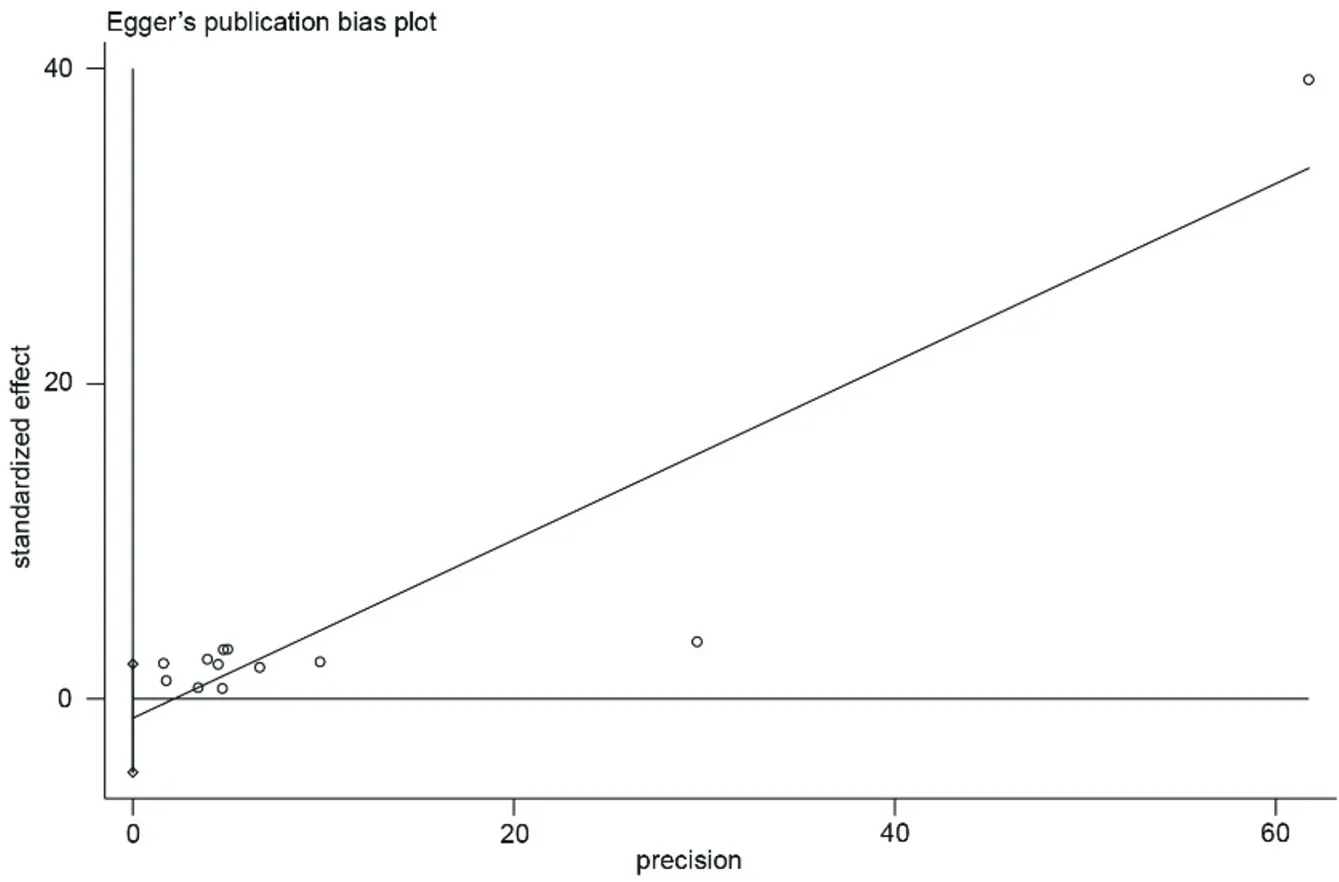
Figure 5. Egger's test for publication bias
4. Discussion
PSD is the most common complication after stroke, especially in the early stage after stroke, not only as a public health problem, but also brings huge economic burden to patients and families [18]. There are many difficulties in the diagnosis of PSD, especially in the early stage after stroke. Moreover, to some extent, PSD can significantly increase the risk of re stroke, suicide and cardiovascular death in patients with stroke [19-21]. Some research shows that the mortality rate of PSD patients is 3.5-10 times higher than that of non PSD patients [22], especially for moderate and severe PSD patients, the risk of death is higher [23]. Our meta-analysis results are consistent with those of our predecessors. The combined results show that PSD can significantly increase all-cause mortality in stroke patients.
At present, the specific mechanism of PSD is not very clear, among which the theory of neurotransmitters (including the change of monoamine neurotransmitters, inflammatory mechanism, growth factors related to glial cell analysis, vitamin D, homocysteine, neural network dysfunction, etc.) has gradually been accepted by most scholars [24]. PSD is closely related to the disorder of HPA axis, resulting in abnormal cortisol secretion, which leads to inflammatory response, especially the significant increase of IL-1 β, TNF - α and IL-6 levels, which may increase the risk of stroke recurrence and mortality [25-26]. In addition, PSD is also closely related to the anatomical site. Some scholars believe that the incidence of poststroke depression in patients with left hemisphere lesions, especially those close to the frontal pole, is significantly higher than that in patients with right hemisphere lesions [27]. Moreover, the damage of anterior cingulate cortex pathway and cerebello hypothalamic pathway of amygdala is also closely related to the occurrence of PSD [28]. Therefore, it is of great significance to recognize the importance of PSD, early diagnosis of PSD and timely and effective intervention for the later rehabilitation of stroke. How to better explain the relationship between PSD and the increase of mortality still needs a lot of research on pathophysiological mechanism. It is assumed that depression can cause cardiovascular risk, recurrence of cerebrovascular events and higher mortality. In addition, early depressive symptoms also frequently occurred in subjects with severe stroke consequences. Therefore, depression may have a significant relationship with the severity of stroke, which in turn may increase the risk of death. The nature of the relationship between depression and mortality remains unclear.
There are many deficiencies in our meta analysis results. First of all, although funnel chart, Begg's and egger's tests all show no publication bias, the included literatures are all from non-China. At the same time, all the studies included in this meta-analysis are retrospective studies, which can not exclude the influence of other interference factors, so the risk of bias is high, so the consideration of the results should be cautious. Secondly, there is significant heterogeneity in the 12 literatures. Although the sub group analysis of the included literatures is carried out, the problem of heterogeneity is still unsolved.
To sum up, the current evidence suggests that PSD affects the risk of death in stroke patients. Although the mechanism of this relationship is not clear, PSD seems to have a negative impact on both short-term and long-term stroke patients and thus affect their lives. Further clinical studies are needed to assess the relationship between emotional disorders and stroke.
杂志排行
Journal of Hainan Medical College的其它文章
- Network pharmacological study of Qingfei Paidu Decoction intervening on cytokine storm mechanism of COVID-19
- Study on the Potential Mechanism of Drug Pair "Honeysuckle-Astragalus" on COVID-19 based on Network Pharmacology
- Observation on clinical application effect of ankle rehabilitation robot
- Meta-analysis of clinical efficacy of combined traditional Chinese and western medicine in the treatment of granulomatous mastitis
- The effect of plasma uric acid on oxidative stress in ankylosing spondylitis by Keap1-Nrf2 signaling pathway
- LINC01614 expression in gastric cancer and its prognostic value based on bioinformatics analyses