Adult-onset Still's disease: A case report
2020-07-23ArunAgarwalDarshanGondaliya
Arun Agarwal, Darshan N Gondaliya
Department of Internal Medicine, Fortis Escorts Hospital, Jaipur, India
ABSTRACT Rationale: Fever of unknown origin (FUO) is a frequently observed phenomenon in clinical practice. Definite diagnosis of FUO is a great challenge in clinical practice since potential causes for FUO involve more than 200 diseases. Adult-onset Still’s disease is a defined clinical entity and a known rare cause of FUO.Patient’s concern: A 19-year girl was referred to the clinic with the concern of intermittent fevers and shivering for almost a year despite multiple investigations and consultations. She had undergone intensive serologic, radiologic, laboratory investigations to exclude infectious diseases, connective tissue diseases, and malignancy, and all the investigation showed no conclusive diagnosis.Diagnosis: Adult-onset Stills disease.Intervention: Steroids and supportive treatment.Outcomes: The symptoms were relieved within three days, and the patient became asymptomatic.Lessons: Physicians need to be familiar with the diagnostic criteria of adult-onset Still’s disease, or it shall remain a diagnostic dilemma. Besides, all shivers are not infections.
KEYWORDS: Fever of unknown origin; Adult-onset Still’s disease;Autoinflammatory disease; Yamaguchi criteria; Fautrel criteria
1. Introduction
Fever of unknown origin (FUO) was originally defined by Petersdorfet al.[1] in 1961, which is now defined as fever >38.3℃(101oF) on at least two occasions; illness duration of ≥3 weeks;no known immunocompromised state; and the diagnosis remains uncertain after a thorough history-taking, physical examination,and the following obligatory investigations: determination of erythrocyte sedimentation rate (ESR) and C-reactive protein(CRP) level, platelet count, leukocyte count and differential, levels of hemoglobin, electrolytes, creatinine, total protein, alkaline phosphatase, alanine aminotransferase, aspartate aminotransferase,lactate dehydrogenase, creatine phosphokinase, ferritin, antinuclear antibodies, and rheumatoid factor, protein electrophoresis,urinalysis, blood cultures (n=3), urine culture, chest X-ray,abdominal ultrasonography, and tuberculin skin test[2].
Adult-onset Still’s disease (AOSD) is an autoinflammatory disorder characterized by the classic triad of persistent high spiking fever,arthralgia, and salmon-colored skin rash. Its diagnosis is challenging due to the absence of serological biomarkers. In fact, the diagnosis is usually through the exclusion of infectious, malignant, and other connective tissue diseases, and a definitive diagnosis is usually made based on the Yamaguchi[3] or Fautrel[4] criteria.
As per clinical presentation of the disease, two distinct AOSD phenotypes may be distinguished clinically: (1) An acute systemic febrile illness, with a monocyclic or polycyclic pattern, is highly symptomatic, and may evolve into a multi-organ dysfunction or failure and can even be fatal if not timely diagnosed and treated; (2) A more slowly evolving illness with arthritis and less of systemic symptomatology, and finally evolving into a chronic articular pattern.
Timely diagnosis and treatment with corticosteroids followed by maintenance therapy with disease-modifying anti-rheumatic drugs(DMARDs) or biologic drugs such as tumor necrosis factor-α(TNF-α) agents or interleukin (IL-1) antagonists, which can prevent complications and lead to a favorable prognosis. Steroid and DMARDs refractory cases with a systemic pattern may be benefited by anakinra, active arthritis with systemic symptoms by tocilizumab, and chronic polyarticular refractory AOSD by TNF-α blockers, respectively[5].
2. Case report
This study was approved by the Narayana Hospital Medical Ethics committee, Jaipur (No. NHMECJ/JPR/2020/08), and informed consent was obtained from the patient. A 19-year-old girl was referred to the clinic on December 4th 2019. She had a fever with shivering since February 2019, and her medical records showed that she had undergone extensive investigations and treated with several courses of antibiotics and antifungals for asymptomatic recurrent urinary tract infections. She was treated as an inpatient at a tertiary care center in Jaipur from February 26th 2019 to March 8th 2019 and discharged as a case of urinary tract infection. She was relatively better from June 2019 to October 2019 with off and on spikes of fever, for which she used to take paracetamol tablets. Since November 2019 she again had a persistent fever with shivering.Various investigations were done between February 2019 to May 2019 and November 2019 to December 2019 (Table 1). Though there were several reports, we have taken the highest total leucocyte counts (TLC), highest platelet count, highest ESR, and lowest hemoglobin (Hb) values during the respective months.
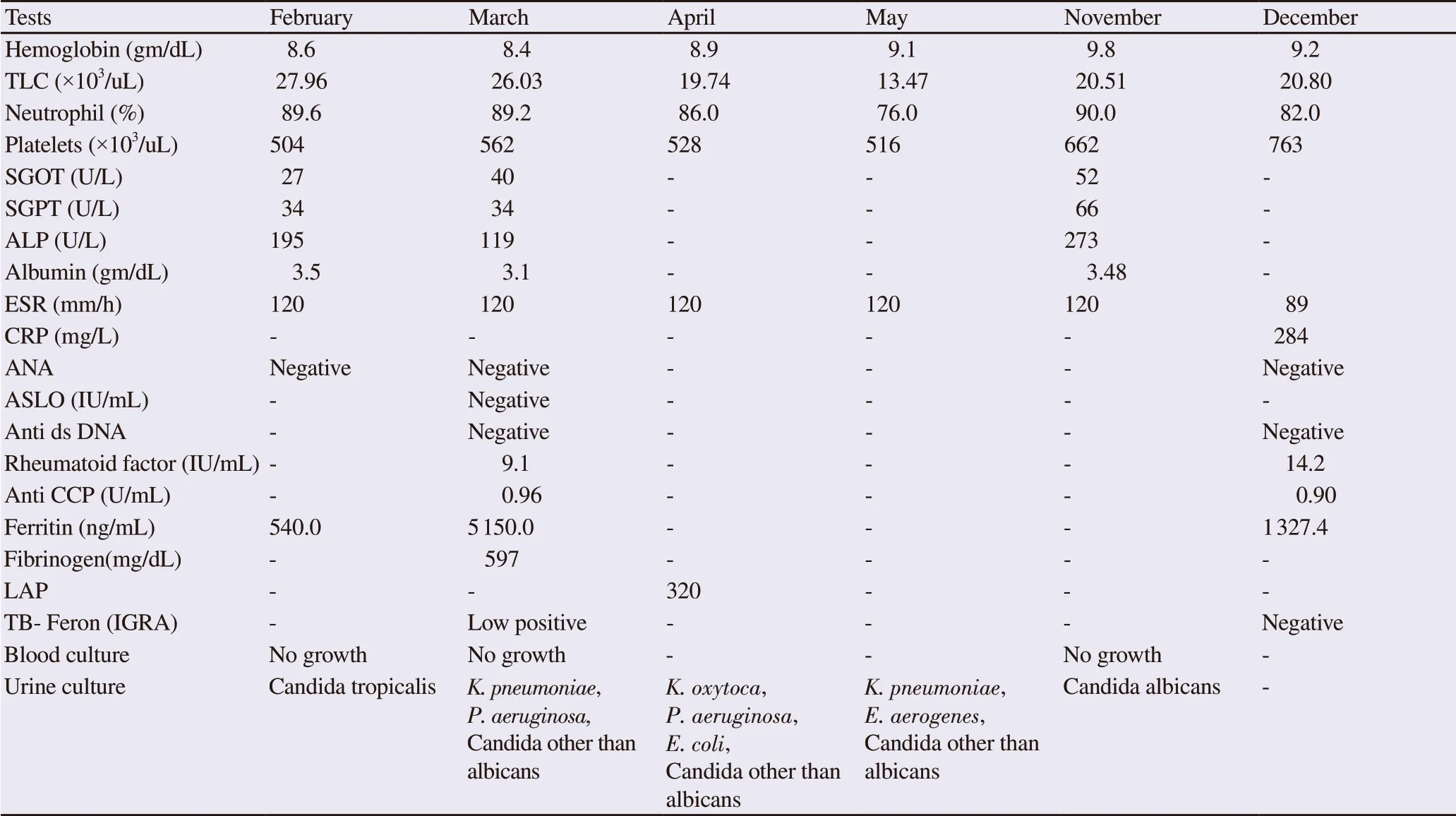
Table 1. Results of hematological/biochemical tests and culture test.
She complained of daily recurrent fever since November 22nd 2019, which was from moderate to high grade, associated with chills usually occurring in the afternoon or evening. She also had mild joint pains involving knees, ankles, hands, and wrists and also mild sore throat. On examination on December 4th 2019, she had a fair complexion, weighed 55 kg (BMI: 21.5 kg/m2), her pulse was regular 96/min, blood pressure 110/76 mm Hg, respiratory rate 19/min, peripheral capillary oxygen saturation (SpO2) 98% on room air and temperature 102oF. She looked unwell and had pain in legs on walking, and the proximal inter-phalange joints were mildly tender and swollen bilaterally. On systemic examination,she had mild nontender hepatomegaly. The rest of the systemic examination was essentially normal. In addition, the patient’s father reported that she usually developed a transient erythematous rash on her body and soles with high fever. The rash would disappear when the fever subsided and finally turned to be non-itchy. Her liver function was mildly deranged along with leukocytosis, neutrophilia,thrombocytosis, and high ESR.
Her laboratory tests such as Mantoux test, Widal test, serology tests for leptospira, brucellosis, scrub typhus, human immunodeficiency virus 1 and 2, hepatitis B and hepatitis C, interferon-gamma release assay forMycobacterium tuberculosis, malaria parasite, antinuclear antibody (ANA), antineutrophil cytoplasmic antibody, ds DNA antibody, protein electrophoresis, rheumatoid factor, anti-cyclic citrullinated peptide, respectively were negative. Bone marrow aspiration showed hypercellular marrow, normoblastic erythroids,and mild myeloid hyperplasia with toxic granulations, increased megakaryocytes and plasmacytosis suggestive of reactive marrow.Computerized tomography of the chest done on March 1st 2019 showed bilateral minimal pleural effusion; High-resolution computerized tomography chest done on March 8th 2019 was unremarkable; Ultrasound abdomen done on February 2rd 2019 and December 2rd 2019 showed bilateral polycystic ovaries and mild hepatomegaly; X-ray chests done on February 2rd 2019 and December 1st 2019 were normal, and 2D echocardiography done on February 27th 2019 was unremarkable.
Considering that we had earlier lost two patients due to late diagnosis of AOSD and the patient’s history of having received repeated courses of antibiotics for months, remittent and persistent fever, myalgias and arthralgia, and raised inflammatory markers with leukocytosis, we suspected AOSD, and then serum ferritin test was done which was reported high. She was reviewed on December 7th 2019, and in view of persistent remittent fever, transient erythematous rash accompanying fever, arthralgia, mild hepatomegaly, raised ESR, CRP and serum ferritin, leukocytosis with neutrophilia and no evidence of infection, malignancy, rheumatic disease or vasculitis,the possibility of an autoinflammatory disorder were evaluated.She fulfilled Yamaguchi and Fautrel criteria for AOSD and finally was diagnosed as a case of AOSD. She was advised to take oral prednisolone 40 mg/d along with other supportive treatment. She responded dramatically to the treatment and became afebrile within 3 d. She is under regular follow-up and is on tapering dose schedule of steroids.
3. Discussion
Connective tissue diseases (CTDs) represent the second most common cause of FUO. The first being infectious diseases[6,7]. The incidence of noninfectious inflammatory diseases is increasing despite the availability of better and advanced diagnostic facilities and awareness among clinicians. These diseases contributed to 17% of FUO cases in 1961 and increased to 22% in 2007[8]. In two retrospective studies, the incidence of AOSD reported was 17.2% among 215 cases of FUO and 15.4% among 130 cases of FUO respectively[6,7]. In one of these, a retrospective study from 215 patients who were diagnosed with FUO, the most common causes of the disease were infectious diseases (42.3%), followed by CTDs (32.1%), miscellaneous (10.7%) and neoplasm (6.5%),while the causes for the other 18 cases (8.4%) were still unknown.The most common types of the three causes were tuberculosis(17.6%), AOSD (53.6%) and non-Hodgkin lymphoma (42.9%),respectively[6]. The clinical findings in AOSD are heterogeneous,and the asymptomatic bacterial infections are generally treated with prescribing of several courses of antibiotics or antifungals for asymptomatic incidentally detected growth(s) in urine specimen as also happened in the case presented.
AOSD as one of the most frequent etiology of FUO is both under-diagnosed and under-reported. Its estimated prevalence is 1.5 cases per 105-106 people, with the first confirmed case in 1971. AOSD is a rare, idiopathic, autoinflammatory, multisystem disorder characterized by two subsets according to the clinical and laboratory features: systemic or articular. The authors have previously reported two fatal cases of AOSD who were diagnosed late[8] and another two patients who were diagnosed timely with a favorable prognosis[7,9]. In a patient with FUO, a maculopapular rash and/or arthralgia and/or sore throat should raise the suspicion of AOSD.
The patient discussed had an intermittent fever for almost 11 months and received multiple courses of antibiotics and antifungals. During the patient’s treatment as an inpatient in February 2019, she was extensively investigated including twice computerized tomography of chests, bone marrow aspiration, and 2D echocardiography. Evidence of transient serositis-pleuritis on first CT scan of chest was missed or ignored. At this time her serum ferritin was also reported high (5 150 ng/mL) but it was probably not considered significant by the treating clinician. A simple differential diagnosis of the various causes associated with hyperferritinemia could have suggested the diagnosis. Further, a polymicrobial growth in urine cultures on multiple occasions in an asymptomatic non catheterized patient should be considered as contamination.
Clinically, the most classic manifestations of AOSD are daily fever (60%-100%), macular or maculopapular evanescent salmonpink skin rash (60%-80%), sore throat (70%), and arthralgia(70%-100%) with fever and arthralgia being the commonest.Other symptoms reported are myalgias (45%), enlargement of the lymph nodes (50%), splenomegaly (40%), hepatomegaly (30%),transaminitis (70%), hypoalbuminemia (76%), serositis-pleuritis(40%), pericarditis (30%), abdominal pain (30%), pneumonitis(20%) and weight loss (27%)[8,10]. Laboratory investigations are notable for the consistent absence of ANAs and RF and can reflect the non-specific systemic inflammatory nature of the disease.Increases in the ESR, CRP level, and serum ferritin are common in AOSD (90%-100%) as were seen in the present case.
The diagnosis of AOSD is clinical. It is not based on serological tests and needs exclusion of infections, malignancies and other rheumatic/systemic vasculitides diseases. Our patient had febrile episodes with mild rash, arthralgia, sore throat, mild nontender hepatomegaly, mild transaminitis, mild hypoalbuminemia, and hyperferritinemia. Her earlier reports mentioned that she had mild transient serositis-pleural effusion on CT chest done in March 2019. The tests for ANA and rheumatoid factor were negative.Among the different criteria available for the clinical diagnosis of AOSD, the Yamaguchi criteria proposed in 1992 is the most widely cited criteria for the diagnosis of AOSD, most sensitive(96%) and still manage to retain a high degree of specificity[3]. It includes 4 major criteria (fever >39 ℃, lasting 1 week or longer,arthralgia or arthritis lasting 2 weeks or longer, typical rash and leukocytosis >10 000/mm3with >80% polymorphonuclear cells),5 minor criteria (sore throat, recent development of significant lymphadenopathy, hepatomegaly or splenomegaly, abnormal liver function tests, negative tests for ANA and rheumatoid factor) and exclusion criteria (Infections, malignancies and other rheumatic/systemic vasculitides). The diagnosis requires at least 5 features,with at least 2 of these being major diagnostic criteria. Our patient had all 4 of the major criteria, 2 of the minor criteria, and all 3 of the exclusion criteria. In 2002, Fautrelet al.proposed a new criterion which contained 2 new markers: serum glycosylated ferritin fraction <20% and >80% neutrophil polymorphonuclear count[4]. It includes 6 major criteria (spiking fever ≥39 ℃,arthralgia, transient erythema, pharyngitis, polymorphonuclear cells ≥80%, and glycosylated ferritin ≤20%) and 2 minor criteria(maculopapular rash and leukocytosis ≥10 000/mm3). Diagnosis of AOSD by Fautrel criteria requires 4 or more major criteria or 3 major and 2 minor criteria. Our patient had 5 major and 2 minor criteria. The sixth major criterion of glycosylated ferritin was not done due to the non-availability of the test. Instead, serum ferritin was done which was high in February 2019 as well as in December 2019.
Many different therapies have been tried for patients with AOSD.Besides symptomatic and supportive treatment, nonsteroidal anti-inflammatory drugs for fever, joint pain, and bone pain,corticosteroids for systemic symptoms, DMARDs, methotrexate,hydroxychloroquine, azathioprine or tumor TNF inhibitors are used depending on disease severity and drug safety. We treated this patient with nonsteroidal anti-inflammatory drugs, oral prednisolone, and supportive drugs with good response and defervescence. In refractory cases alternative treatment with anti-TNF agents (infliximab, etanercept, and adalimumab), IL-1 inhibitors (anakinra, canakinumab, and rilonacept) and IL-6 receptor antibody (tocilizumab), have been shown to induce remission in patients with AOSD. Plasma exchange and intravenous immunoglobulins are other treatment options in refractory AOSD patients.
To conclude, all shivers and fevers are not infections and inflammatory diseases, and particularly, AOSD should be considered early in FUO cases. Physicians need to be familiar with AOSD diagnostic criteria or it shall remain a diagnostic dilemma.Serum ferritin as a new biomarker may be used to facilitate early diagnosis of AOSD[9]. Timely diagnosis and treatment of the disease can prevent complications and lead to a favorable prognosis. Delay in diagnosis, pleuritis, interstitial pneumonia,markedly elevated ferritin levels, and failure of fever to subside after 3 d of treatment (prednisolone) are unfavorable prognostic factors for patients presenting with a severe systemic form of AOSD.
Conflict of interest statement
The authors report no conflict of interest.
Authors’ contributions
This work was carried out in collaboration between both authors.A.A. was the primary consultant in this case. He contributed to the conception, design, and analysis of the case study. He wrote the first draft of the manuscript and approved the final work to be published.D.N.G. managed the tabulation work, literature searches, and final grammar correction of the manuscript. Both authors read and approved the final manuscript.
杂志排行
Journal of Acute Disease的其它文章
- "Resuscitator": Golden medtech proposal introducing a new era for CPR
- Incidence of Enterobius vermicularis in acute appendicitis: A systematic review and meta-analysis
- Prevalence and antimicrobial susceptibility patterns of bacteria in ICU patients with lower respiratory tract infection: A cross-sectional study
- Effect of 8-week and 12-week triple therapy (doxycycline, rifampicin,and gentamicin) on brucellosis: A comparative study
- Open reduction and internal fixation for radial head fractures: A prospective observational study
- Cope’s sign and complete heart block secondary to acute cholecystitis: A case report
