Blastocyst elective single embryo transfer improves perinatal outcomes among women undergoing assisted reproductive technology in Indonesia
2020-06-23IvanSiniNiningHandayaniAdindaPratiwiAriePolimAriefBoediono
Ivan Sini, Nining Handayani, Adinda Pratiwi, Arie A Polim,3, Arief Boediono,4
1Morula IVF Jakarta, Jakarta, Indonesia
2IRSI Research and Training Center, Jakarta, Indonesia
3Department of Obstetrics and Gynecology, School of Medicine and Health Science, Atmajaya Catholic University of Indonesia, Jakarta, Indonesia
4Department of Anatomy, Physiology and Pharmacology, IPB University, Bogor, Indonesia
ABSTRACT
KEYWORDS: Single embryo transfer; Perinatal outcome;Blastocyst transfer
1. Introduction
In vitro fertilization (IVF), as part of assisted reproductive technology (ART), has been acknowledged globally since its introduction in 1978 for providing a promising solution to infertility treatments in both developed and developing countries[1,2].Traditionally, to achieve “desirable” implantation and clinical pregnancy event, multiple embryo transfer was often performed in ART programs. However, high rate of multiple births, low birth weight, and preterm birth were later found to correspond to the practice of multiple embryo transfer[3]. Therefore, over the last decade, there was an intentional reduction in the number of embryos that can be transferred to the uterus at one time, with the prospect of reducing multiple gestation events and improving perinatal outcomes[4].
Previously, the number of transferred embryos in ART prevailed as the clinician’s main concern due to its considerable association with pregnancy rates[5]. However, presently, with the apparent paradigm shift in the aim of ART, favorable perinatal outcomes have been regarded as crucial as successful clinical pregnancies. The main expected goal of ART has now inclined towards achieving a single live birth of a healthy and non-low birth weight baby[6]. To accomplish this,elective single embryo transfer (eSET) and double embryo transfer(DET) have become the two most implemented practices in IVF around the world, including Indonesia[5,6].
Compared with DET, the practice of eSET has been claimed to be more superior in improving perinatal outcomes by reducing the rates of twin and multiple pregnancy without compromising the overall IVF success rate[7,8]. Nevertheless, most of the proponents of this evidence involve studies conducted on European and American populations which might not apply to the Asian population,particularly the Indonesian population[9-13].
Even though IVF is not a new practice in Indonesia, eSET is still uncommonly performed. In fact, DET remains as the most popular method used in IVF programs due to reasons such as financial limitations, lack of patients’ understanding regarding the complications of multiple pregnancy, as well as patients’ own preferences in conceiving twins.
To our knowledge, no study has yet compared the perinatal outcomes of eSET and DET in Indonesian population. Moreover,similar studies conducted in developing countries were still limited and provided scarce results. In this study, we, therefore, aimed to compare the effectiveness between eSET and DET in lowering the risks of poor perinatal outcomes including low birth weight, preterm birth, and perinatal mortality in Indonesian IVF patients.
2. Materials and methods
2.1. Study design and eligibility criteria
A retrospective observational study was conducted at Morula IVF Clinic, the largest fertility clinic in Indonesia. The inclusion criteria were women who achieved birth following either a successful blastocyst eSET or DET in the clinic between January 2015 and December 2017. Good prognosis women (anti-Müllerian hormone level ≥1.1 ng/mL, antral follicle count >5, basal follicle-stimulating hormone level ≤12 mIU/mL, and/or basal estradiol ≤75 pg/mL) and poor prognosis women [advanced maternal age (>38 years), antral follicle count ≤3, and/or anti-Müllerian hormone levels <1.1)] were included. Women with a history of recurrent miscarriages, severe endometriosis, or incomplete infants’ medical records were excluded to reduce potential confounders. All of the studied participants underwent controlled ovarian stimulation, including gonadotropinreleasing hormone agonist long protocol, gonadotropin-releasing hormone antagonist protocol, and mild stimulation protocol. During the study period, out of 644 women who underwent either eSET or DET in their IVF cycles, 233 were clinically pregnant. A total of 178 women eventually achieved births and one woman was stillbirth at 22 weeks of gestation. Briefly, a total of 76 women who underwent blastocyst eSET and 103 women who underwent blastocyst DET were included in the study (Figure 1).
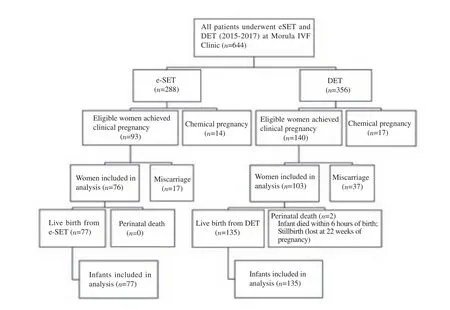
Figure 1. Schematic study of elective single embryo transfer (eSET) versus double embryo transfer (DET).
2.2. Study parameters
The primary study parameters included low birth weight rate,preterm birth rate, and perinatal mortality. Low birth weight was defined as birth weight less than 2 500 g (multiple gestations included)[14]. Preterm birth was defined as childbirth occurring between 20 weeks 0 day and 36 weeks 6 days of gestation.Preterm birth rate was calculated as the number of preterm births divided by the total number of live births (multiple gestations included)[15]. Perinatal mortality that consisted of stillbirths, was defined as pregnancy loss at >20 weeks, and early neonatal deaths within the first 7 days of life[12]. The secondary study parameters included Apgar score (based on a total score of 1-10, subjects were categorized into Apgar score of ≥7 or <7 at 1 min and 5 min after birth), neonatal intensive care unit (NICU) admission rate, multiple pregnancy, and maternal complication during pregnancy. Multiple pregnancy was defined as the presence of more than one fetal heartbeat through ultrasound examination.
2.3. Sampling and statistical analysis
To optimize the power of research and internal validity, a total(purposive) sampling method was used. Data were analyzed by using the Statistical Package for the Social Sciences (Release 20.0,SPSS, Inc., Chicago, IL, USA). To compare categorical variables between eSET and DET group,χ2test was performed. To compare continuous variables, either independent t-test or Mann-Whitney U test was performed accordingly depending on the data distribution.To adjust for potential confounders, multiple logistic regression was performed for the primary outcomes. A P-value <0.05 was considered statistically significant.
2.4. Ethics statement
The study was approved by the Ethical Committee of the Faculty of Medicine, University of Indonesia on August 13, 2018 (protocol number: 0818/UN2.F1/ETIK/2018).
3. Results
3.1. Participants’ baseline characteristics
Compared with the DET group, women in the eSET group had a significantly lower proportion of participants ≥35 years old and median of body mass index. Of the women involved in this study, 94.97% were good prognosis patients while the remaining 5.03% acquired poor prognosis. Other baseline characteristics including median age, types of infertility, history of female smoking and female alcohol consumption between the two groups were comparable. The most common infertility causes among the studied women were other factors (e.g., polycystic ovary, myomas,diminished ovarian reserve), followed by sperm factors, tubal factors and unexplained factors.
No significant differences (P>0.05) between the eSET and DET groups were observed with regard to the anti-Müllerian hormone level, antral follicle count, basal follicle-stimulating hormone level,basal estradiol level, as well as estradiol level on the trigger day of human chorionic gonadotropin injection to induce follicular maturation. The number of embryos available for transfer was also comparable between the two groups (Table 1).
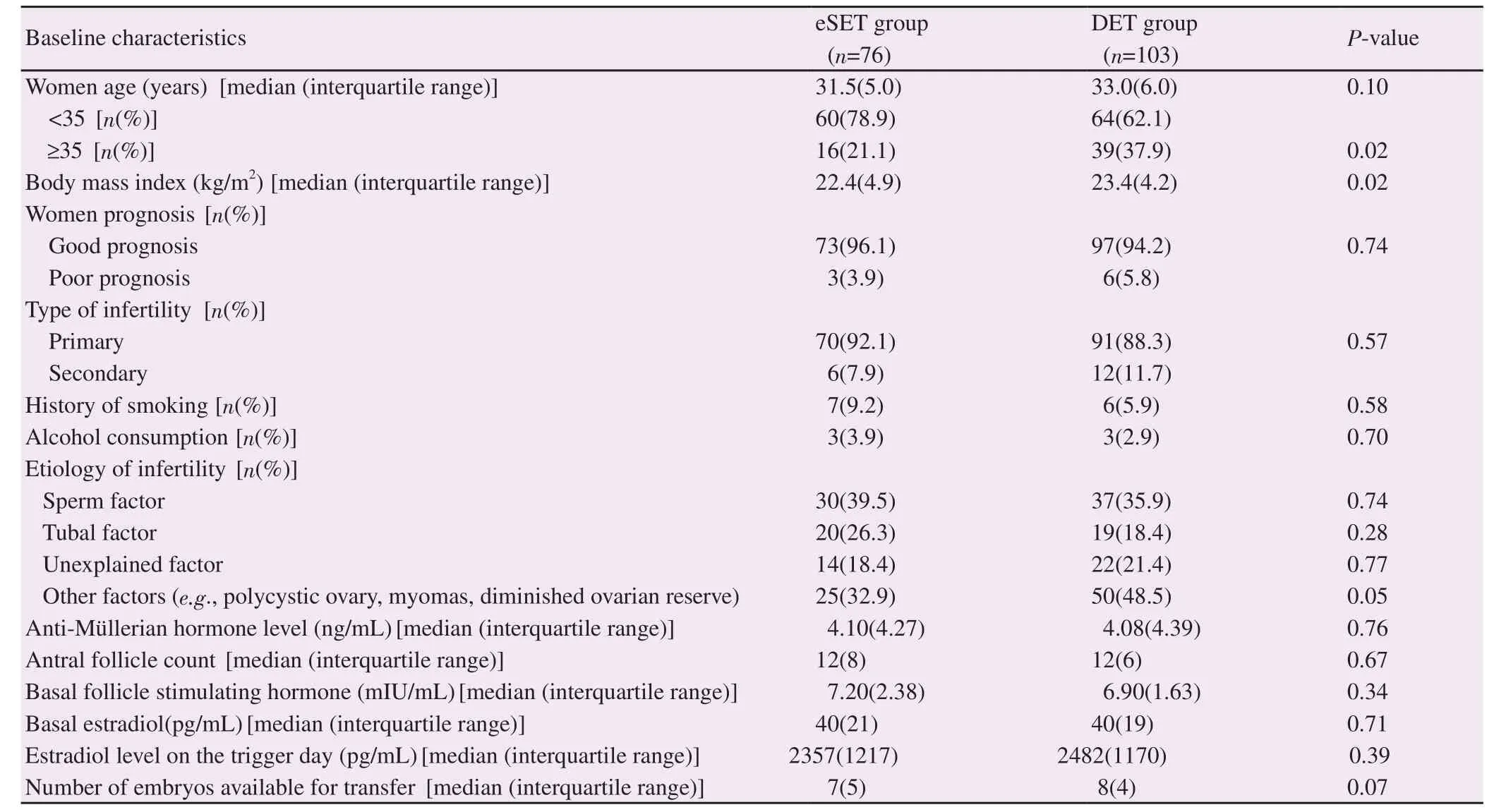
Table 1. Baseline characteristics of women in this study.
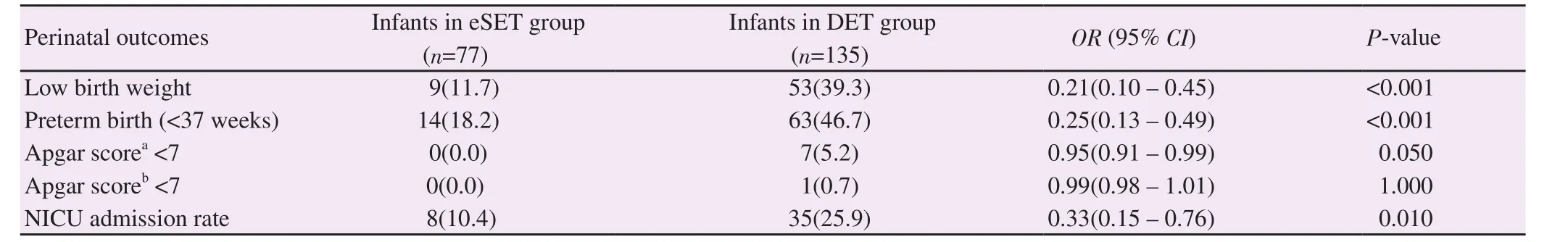
Table 2. Association of perinatal outcomes of live-born infants between the eSET and DET groups [n(%)].
3.2. Primary and secondary outcomes
A total of 76 women who underwent eSET achieved 77 live births,without any perinatal deaths. On the other hand, 103 women who underwent DET culminated to 135(98.5%) live births and 2(1.5%)perinatal deaths. No significant difference was noted in terms of perinatal mortality [odds ratio (OR)=0.98, 95% confidential interval(CI): 0.96-1.01; P=0.54] as well as Apgar score in both one minute and five minutes after birth (P≥0.05) between the eSET and DET groups.
Compared with the DET group, low birth weight rate and preterm birth rate were significantly lower in the eSET group (P<0.001).Consistent outcomes of low birth weight rate (adjusted OR=0.31,95% CI: 0.12-0.82, P=0.02) and preterm birth rate (adjusted OR=0.27, 95% CI: 0.13-0.54, P<0.001) were also noticed in the multivariate analysis adjusted for maternal age and presence of perinatal complications. In addition, eSET utilization significantly reduced the NICU admission rate (P=0.01) (Table 2).
From maternal aspects, women in the eSET group had a significantly lower risk of multiple pregnancy compared to the DET group (1.3% vs. 33.0%; OR=0.03, 95% CI: 0.003-0.186;P<0.001) after adjusting for potential confounders (maternal age,body mass index, antral follicle count, estradiol level on trigger day and number of embryo transferred). Despite the higher prevalence of multiple gestations in the DET group, there was no significant difference between maternal complications in both studied groups with respect to the occurrence of gestational diabetes (0.0% vs. 1.0%,P=1.00), preeclampsia (3.9% vs. 0.0%, P=0.07), and pregnancyinduced hypertension (5.3% vs.1.9%, P=0.40). However, antepartum hemorrhage was significantly lower in women who underwent eSET compared to those who went through DET (10.5% vs. 25.7%;OR=0.37, 95% CI: 0.15-0.89; P=0.03) after adjusting for potential confounders (maternal age and body mass index).
4. Discussion
This study showed that infants conceived through an IVF procedure with eSET would acquire reduced risks of poor perinatal outcomes,verified through the lower rates of low birth weight, preterm birth and NICU admission. This is justified by similar findings of other studies[16-18].
A study performed by Hayashi et al[16] on Japan’s 10-year perinatal database reported a significant decrease in the incidence of preterm delivery, low birth weight, and NICU admission following increased utilization of eSET. A larger observational study conducted by Kissin et al[17] also showed similar results. The study, involving 82 508 participants has indicated that in comparison with the DET practice,eSET culminated to better perinatal outcomes described as single or twin infants with normal birth weights (43% vs. 27%, respectively).On the contrary, a large cohort study conducted by Fechner et al[15]could argue against our findings for their disclosure of a higher preterm birth rate in ART program utilizing eSET compared to those which did not utilize eSET (17.6% vs. 12.0%). It was suggested that infertility itself was the predominant risk factor of preterm birth regardless of the number of embryos transferred and the incidence of multiple gestations. However, further study has to be conducted to validate this hypothesis[15].
Our study also reported that eSET had drastically reduced the multiple pregnancy rates, justifying several previous studies[15-18].Chambers et al[19] showed a linear decrease in multiple gestations as the practice of eSET expanded. Their study population was similar to ours, which consisted mostly of women aged less than 38 years old. As multiple pregnancy has been greatly associated with the occurrence of preterm birth, low birth weight and perinatal complications, the reduction of its incidence in IVF cycles utilizing eSET might have contributed to the favorable perinatal outcomes in the respective study group. In addition to its negative impacts on perinatal outcomes, multiple gestation could adversely influence infant’s first year of life and increase the demand for healthcare and cost of living throughout the neonatal period up to 1-year old[19].
Maternal complications were also apparent in a number of multiple pregnancy cases[20]. However, despite the higher prevalence of multiple pregnancy in the DET group, the manifestations of gestational diabetes, preeclampsia, and pregnancy-induced hypertension among the women in eSET and DET group of this study did not differ. This may be due to the multifactorial nature of maternal complications that were not solely driven by the multiple pregnancy events[21,22]. Additionally, not all of the risk factors of maternal complications were measured in our study.
The prevalences of gestational diabetes, preeclampsia, and pregnancy-induced hypertension in this study were comparable to that of the general Southeast Asian population[23-26], contrary to the prevalence of antepartum hemorrhage which was higher in our study population. Although the mechanisms remain unclear, this finding could be parallel to several underlying conditions such as uterine abnormalities and placental disorders, which both were often diagnosed in women undergoing ART[27,28].
Limitations common to any retrospective observational study designs are also relevant to our study. Firstly, several data were missing, specifically in regard to the baseline characteristics of the study population. Nonetheless, it had been assured that they did not affect the study results. Secondly, although multivariate analysis had been performed to adjust for potential confounders, immeasurable residual confounders still persisted. Thirdly, the decision-making procedures of the infertile couple in deciding the number of embryos to be transferred remained unknown. However, due to the lack of subsidies, overall cost of ART to achieve a live birth may exhibit a significant impact on the patients’ decision. We also acknowledged that a larger sample size is required to generalize our findings to the overall target population; IVF patients in Indonesia. Nevertheless,given the absence of a reliable national perinatal data registry, this study holds value for the Indonesian population in suggesting the practice of single embryo transfer to reduce the risks of perinatal complications.
In conclusion, infants conceived through ART program with eSET had significantly lower low birth weight rate and preterm birth rate compared to those conceived through DET. eSET also resulted in lower incidence of multiple pregnancy. Overall, our results seem to suggest that the reduction in the number of embryos i.e. blastocysts being transferred to the uterus at one time is important to improve the perinatal outcomes in IVF.
Conflict of interest statement
The authors declare that there is no conflict of interest.
Authors’ contributions
The original concept was conceived and designed by Ivan Sini.Data were collected and analyzed by Nining Handayani and Adinda Pratiwi. Ivan Sini, Nining Handayani, Adinda Pratiwi, Arie A Polim,and Arief Boediono performed study literature, data interpretation,and drafted the manuscript. All authors have read, revised and approved the final manuscript.
杂志排行
Asian Pacific Journal of Reproduction的其它文章
- Efficacy of standard therapy with synbiotic or without synbiotic to reduce Gardnerella vaginalis, Atopobium vaginae and Megaesphaera phylotypeⅠin pregnant women with bacterial vaginosis
- Effect of double cleavage stage versus sequential cleavage and blastocyst stage embryo transfer on clinical pregnancy rates
- Effects of vascular endothelial growth factor supplementation and alginate embedding on human oocyte maturation in vitro
- Antifertility effects of Azadirachta indica methanol seed extract on canine spermatozoa in vitro
- Ascorbic acid and curcumin alleviate abnormal estrous cycle and morphological changes in cells induced by repeated ultraviolet B radiations in female Wistar rats
- Effects of extender and packaging method on morphological and functional characteristics of cryopreserved Ossimi ram semen