Clinical observation on acupuncture plus subtle adjustment manipulation of the cervical spine for peripheral facial paralysis
2020-06-22ChenJianqiang陈剑强LiuChenxi柳晨希GongXufang龚旭芳ChenYaping陈雅萍LiangLi梁莉RongjunHospitalofZhejiangProvinceJiaxing314000China
Chen Jian-qiang (陈剑强),Liu Chen-xi(柳晨希),Gong Xu-fang (龚旭芳),Chen Ya-ping (陈雅萍),Liang Li(梁莉)Rongjun Hospital of Zhejiang Province,Jiaxing 314000,China
Abstract
Keywords:Acupuncture Therapy; Tuina;Massage;Manipulations;Facial Paralysis
The full name of peripheral facial paralysis is idiopathic peripheral facial paralysis, referring to an acute nonsuppurative inflammatory disease caused by physical or chemical stimulation to a lateral facial nerve during its passage through the stylomastoid foramen[1].Main clinical manifestations are decreased or disappearance of the forehead lines on the affected side, inability to completely close the eyes,retroauricular pain, hearing impairment, shallow nasolabial sulcus, taste abnormality, and deviation of the mouth. This disease is not life-threatening, but affects the patient’s facial appearance as well as physical and mental health. Besides, it may result in paralytic myoatrophy, mimetic convulsion and synkinesis if not properly or correctly treated[2]. It is a common disease in Acupuncture and Tuina Departments, with a high incidence rate of 258/100 000.The disease can occur in people at any age, mostly in young and middle-aged people[3], without obvious seasonal onset. Hormone, antiviral or neurotrophic drugs are mainly adopted by modern medicine, but presenting shortcomings such as long treatment course,uncertain clinical efficacy and sequelae. While traditional Chinese medicine (TCM), especially acupuncture,among thebest methods totreat peripheral facial paralysis recommended by the World Health Organization (WHO), has unique advantages of rapid clinical efficacy and less sequelae. Clinical practice has found that this condition is related to dislocation of small joints of the adjacent upper cervical vertebrae[4].Therefore, this study observed the clinical efficacy of acupunctureplussubtleadjustment manipulationof the cervicalspinefor peripheral facialparalysis. The details are as follows.
1 Clinical Materials
1.1 Diagnostic criteria
The diagnostic criteria referred theTherapeutics of Acupuncture and Moxibustion[5]:suddenonset;enlargedpalpebralfissure onthe affectedside,lagopthalmus, presence of the white sclera when the eyeballof theparalyzedsiderotatesupwardand outward, lacrimation, shallow or absence of forehead wrinkles on the affected side andinability to frown;shallow nasolabial folds on the affected side,mouth deviation towards the healthy side, air leakage from the angulusoris of the affectedsidewhenpuffingand whistling, salivating when chewing food, and speaking with a lisp; together with different degrees of hearing impairment and/or taste impairment of the front 2/3 of the tongue.
1.2 Inclusion criteria
Thosewho met theabovediagnostic criteria,meanwhile, presenting heaviness and distension in the occipitalregionof theneck,paininretroauricular mastoidarea,diagnosedasbilateralasymmetry of transverseprocess of atlas(posterior marginof the sternocleidomastoid muscle at the same height of the midpoint of the line between mastoid and mandibular angle), or deviated spinous process of axis, tenderness pain in perispinous process; aged between 16 and 65 years old, with disease duration between 1 and 60 d;signed informed consent.
1.3 Exclusion criteria
Those who were diagnosed as peripheral facial nerve injury caused by craniocerebral injury, tumor or other diseases;thosewithcerebrovascular diseasesand central facial paralysis; those with severe organ damage suchas heart,liver andkidney;womenwho were during pregnancy andhadahistory of threatened miscarriage; those who had contraindications of bone setting manipulation such as cervical fracture, tumor,tuberculosis, rheumatic arthritis,rheumatoid arthritis,severe osteoporosis, etc.; those who wereunable to cooperatewith the treatment as aresult of mental diseases.
1.4 Statistical methods
The SPSS version 23.0 statistical software was used for data analysis. The counting data were presented in the formof casenumber and/or percentage,and checkedby Chi-squaretest.The measurement data were expressed as mean ± standard deviation (±s)andcheckedbyt-test.P<0.05indicatedstatistical significance.
1.5 General data
A total of 60 cases withperipheral facialparalysis who received treatment from the Rongjun Hospital of Zhejiang Provincebetween July 2017 andDecember 2018wererecruitedinthestudy.According tothe method of randomnumber table generatedby SPSS version23.0,they were randomly dividedinto two groups,with30 casesineachgroup.Casesinthe acupuncture plus tuina group were aged between 16 and 65 years old, with disease duration between 1 and 60 d, while cases in the acupuncture group between 18 and 62 years old, with disease duration between 1 and 60 d.Therewerenosignificant between-group differencesingender,ageanddiseaseduration(allP>0.05),indicating that the twogroupswere comparable (Table 1).

Table 1.Comparison of general data between the twogroups
2 Therapeutic Methods
2.1 Acupuncture plus tuina group
Patients in the acupuncture and tuina group were given subtle adjustmentmanipulation of the cervical spine on theaffectedside, followedby acupuncture treatment.
2.1.1 Tuina treatment
Before acupuncture treatment, patients were given subtle adjustment manipulation of the cervical spine on the affected side.
Thedoctor applieddigitalAn-pressingandRoukneading to thepoints locatedin thepatient’s neck such asFengchi(GB20),Fengfu(GV 16) and Yifeng (TE 17), (Figure 1); Gun-rolling manipulation was used to relax the soft tissues of neck and shoulder muscles on the affected side, especially, the part from behind the ear totheendof themuscles at theinferior occipital muscles at tuberosity.
The patient lay on the healthy side on the treatment bed. Taking the right affected side as an example, the patient lay on the left side, and his head and neck were on a thin soft pillow to relax the head and neck and slightly extended backward.
The doctor stood in front of the patient’s chest and pointed the right thumb belly against the tip of the right transverseprocess of the atlas, theleft thumbbelly against the right mandibular angle, and the two thumbs were in the shape of a ‘cross’. Slowly and evenly, the right thumbpushedbackwardwhiletheleft thumb forward. The manipulation stopped when there was a sense of shifting,oftenaccompaniedby bone joint friction sound (Figure 2). The operation was the same on the other side.
The doctor then touched the spinous process of the axis with his thumb to check if it deviating leftward or rightward (Figure 3). Taking it deviated rightward as an example, the left hand held the patient’s mandibular part, the four fingersand thenar of the righthand,except the thumb, held the patient’s occipital part, and the tip of the right thumb was against the right side of thespinousprocessof theaxis.Pulledoutand stretchedthecervicalvertebraewithgradually increasing strength and kept the head and neck slightly bent back (Figure 4). After 5 s of traction, the left hand turned the patient's head to the left, while the right thumbforcedagainst thespinousprocess of the epistropheustotheleftwithgradually increasing strength(Figure5). Themanipulationstopped when there was a sense of shifting, often accompaniedby bone joint friction sound.

Figure 3.Checking the spinous process of axis with the thumb

Figure 4.Bashen-pulling and stretching the cervical vertebrae
Slow, soft and continuous strength rather than brute strength should be employed in the manipulation. This treatment was given once a day, 10 times for a course of treatment, and lasted for three courses.forehead,frowning,closing theeyes,shrugging the nose, muscle strength of the affected side, nasolabial sulcus, bulging the cheeks, showing teeth, whistling and lowering the underlip, 10 points for each item, with the totalscore dividedinto 6 levels.LevelⅠmeant normality (100 points); levelⅡmild dysfunction (≥75 points,<100 points);levelⅢmoderatedysfunction(≥50 points,<75points);levelⅣrelatively severe dysfunction(≥25points, <50points);levelⅤsevere dysfunction(>0points,<25points);levelⅥmeant complete paralysis (0 point). The lower the total score,the severer the condition of the patient.
3.2 Efficacy evaluation criteria
Recovery: The total score went to levelⅠ, and the facial expression was normal.
Markedly effective: The total score went to levelⅡ.Bilateralforeheadlines andnasolabialsulcusgot basically symmetrical,lagophthalmusstillpresented,frownedwithoutstrength,andlabialangles were slightly asymmetric when laughing.
Improvement: The total score went to level Ⅲ after treatment, which was level Ⅳ or Ⅵ before treatment.
Failure: The total score was worse than level Ⅳ after treatment.
3.3 Results
3.3.1 Comparison of the efficacy
The total effective rate of the acupuncture plus tuina group was 93.3% while that of the acupuncture group was 70.0%, suggesting that the clinical efficacy of the acupuncture plus tuina group was significantly better than that of the acupuncture group (χ2=5.455,P=0.020),(Table 2).
3.3.2 Comparison of the rehabilitation score
Patients inbothgroupsreceivedrehabilitation assessment before and amonth after the treatment respectively. Before treatment, there was no significant between-groupdifferenceinthetotalscoreof rehabilitation assessment (t=0.396,P=0.694). A month after treatment,thetotalscores of rehabilitation assessment inbothacupunctureplus tuinagroup(t=76.473,P=0.000) and acupuncture group (t=47.390,P=0.000) weresignificantly higher than thosebefore treatment, and the total score of the acupuncture plus tuina group was significantly higher than that of the other group(t=35.885,P=0.000).Check Table 3for details.

Table 2. Comparison of the efficacy between the two groups (case)
2.1.2 Acupuncture treatment
Points located in the head and face: Touwei (ST 8) on theaffectedside,Yintang(GV 29),Cuanzhu(BL 2),Yuyao (EX-HN 4), Taiyang (EX-HN 5), Quanliao (SI 18),Yangbai (GB14), Sibai (ST 2), Juliao (ST 3), Yingxiang (LI 20), Shuigou (GV 26), Dicang (ST 4), Jiache (ST 6),Chengjiang (CV 24), Xiaguan (ST 7), Qianzheng (Extra)and Yifeng (TE 17).
Distal points: Hegu (LI 4) on the healthy side.
Point combinationonthepatterndifferentiation:Lieque (LU 7) for wind cold; Quchi (LI 11) for wind heat;Fenglong (ST 40) for phlegm obstruction; Taichong (LR 3)for heat inliver andgallbladder; Zusanli(ST 36)for deficiency of qi and blood.
Methods:Hwatobranddisposablesterile acupunctureneedles of 0.30 mmindiameter and 25-40 mm in length were used. The patient lay on the treatment bedwithrelaxation. The skinaroundthe point wasdisinfectedwith75% alcoholcottonball.Needled Sibai(ST 2), Shuigou(GV 26) and Yingxiang (LI 20) by 0.3-0.5 cun; needled Touwei (ST 8), Yintang(GV 29),Yangbai(GB14)andYuyao (EX-HN4)by 0.3-0.5 cun; needled Cuanzhu (BL 2), Taiyang (EX-HN 5),Quanliao (SI 18), Juliao (ST 3), Chengjiang (CV 24) and Qianzheng (Extra)obliquely by 0.5-1.0cun;needled Dicang (ST 4) and Jiache (ST 6) toward each other; and needled the rest points perpendicularly by 0.5-1.0 cun.Evenreinforcing-reducing manipulationwasadopted after obtaining qi and the needles were retained for 30 min. During needles retaining, the specific electro- magnetic wavetherapeutic instrument (Chongqing ZhongzhiMedicalInstrumentCo.,Ltd.,China)was employed to irradiate the retroauricular region and the face of the affected side. The treatment was given once a day, 10 times as a course and lasted for 3 courses.
2.2 Acupuncture group
Patients in the acupuncture group only received the same acupuncture treatment as in the other group.
3 Observation of Therapeutic Effects
3.1 Rehabilitation assessment
Assessmentof peripheralfacialparalysiswith integrated traditionalChinese andWesternmedicine was adopted for rehabilitation assessment before and after treatment inbothgroups[6].Thisassessment methodcontained10 items,namely,raising the
Table 3.Comparison of the rehabilitation score between the twogroups ( ±s, point)
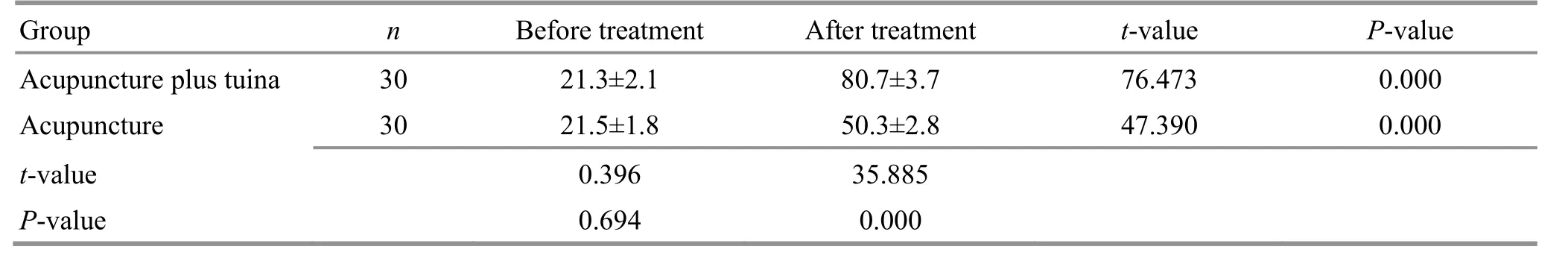
Table 3.Comparison of the rehabilitation score between the twogroups ( ±s, point)
GroupnBefore treatment After treatment t-value P-value Acupunctureplustuina 3021.3±2.180.7±3.776.4730.000 Acupuncture3021.5±1.850.3±2.847.3900.000 t-value 0.39635.885 P-value0.6940.000
4 Discussion
In traditional medicine, peripheral facial paralysis falls under the category of ‘deviation of the mouth and eyes’,anditscausecanbe internal,external,andneither internalnor external.The internalcauseis the deficiency of healthy qi,the externalcausemostly attributes to the exposure to wind, cold and heat, while neither internal nor external cause includes phlegm and stasis. These factors may obstruct the flow of qi and blood and result in malnourishment of meridians in the face[7]. The disease is located in the Stomach Meridian and the Small Intestine Meridian. TCM patterns include wind-cold obstructing collaterals, wind-heat obstructing collaterals, and wind-phlegm obstructing collaterals[8].While modern medicine holds that it is due to facial muscle dyskinesia caused by virus infection, dysfunction of autonomic nerve and nerve entrapment[9]. In clinical treatment, it is found that the stability of the occipito- atlanto-axialjoint isrelatedtotheoccurrenceof peripheral facial paralysis. The relationship between the stability of theupper cervicalvertebraeandthe peripheral facial paralysis presents in two aspects. Firstly,the development of cervical spondylosis to a certain extent may beacausing factor of peripheralfacial paralysis. Secondly, cervical spondylosis can hinder the treatmentandrecovery of peripheral facialparalysis caused by other factors. Long-term bad postures and strain can lead to tension of muscles in the neck, and biomechanical imbalance, thus resulting in dislocations of occipito-atlanto-axial joints.Under this dislocation,the transverseprocessof atlas willpresent displacementinthreedirections:upwardand downward,leftwardandrightward,forwardand backward. However, the anterior edge of the transverse process of atlas is adjacent to the facial nerve which runs from the mastoid foramen, so that the mechanical compressionandstimulationof facialnervecanbe caused[10].Therefore,patientswithperipheralfacial paralysismay feelpaininthemastoidandthe retroauricular regionof theaffectedside,andalso present edema at the mastoid foramen and transverse process of atlas,deviation of the spinous process of upper cervicalvertebrae,andobviousparavertebral tenderness[11]. The blood supply to the facial nerve in the intracranialsegment is viatheanterior-inferior cerebellar arteries, which originate from the middle and lower one third of the basilar artery or the vertebral artery. Therefore, the insufficient blood supply of the vertebrobasilar arteries causedby the dislocations of occipito-atlanto-axial joints can reduce the blood flow of the anterior-inferior cerebellar arteries, thus affecting thebloodsupply to theintracranialsegment of the facial nerve, and ultimately leading to the dysfunction of the facial nerve due to loosing nourishment[12]. Given that, we hold the view that the treatment of peripheral facialparalysis shouldgivepriority tocorrecting the dislocations of occipito-atlanto-axial joints, relaxing the soft tissues around the cervical vertebrae, and relieving the mechanicalcompressionandstimulationto the facial nerve.
By adopting theprincipleof subtleadjustment of spinal short lever, the subtle adjustment manipulation of the cervical spine candirectly adjust theposition relationshipbetweentheoccipito-atlanto-axialjoints via relaxing the soft tissues of muscles in the nape and relieving musclespasm,so asto restorethe occipito-atlanto-axial joints to the normal physiological curveandanatomicalposition,thusrelieving the mechanical compression and stimulation to the facial nerve,improving thenourishment to facialnerve,eliminating local inflammatory edemaincluding facial nerveedema,and improving thebloodcirculation around facial nerve[13].
Meanwhile, needling the local points to unblock the facialmeridians andcollaterals,andpromotethe circulationof qiandblood,hasthesameeffect of stimulating facial muscles to increase their excitability adopted in Western medicine. Combination of the distal point functions to dispel wind and dissipate cold, and regulate qi and activate blood[14], and also to restore the conduction function of the facial nerve and strengthen thecontractionof muscles[15].Acupuncture canalso regulate and maintain the balance of nerves, endocrine and immunity of the body, enhance the resistance to disease and increase the immunity[16-20].
In conclusion, the clinical efficacy of this treatment is valid.It caneffectively relievethemechanical compressionandstimulationtothefacialnerve,promote the absorption of edema, shorten the time of facial nerve compression, improve the function of facial nerve, and thus increase the chance of recovery, and shorten the treatment course.
Received:20September 2019/Accepted:1November 2019
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic observation on lung-clearing and spleen-strengthening tuina in children with exogenous cough
- Effects of electroacupuncture plus drug anesthesia on pain and stress response in patients after radical surgery for stomach cancer
- Therapeutic effect of heat-sensitive moxibustion plus medications for senile osteoporosis and its effect on serum BMP-2 and OPG levels
- Clinical observation on heat-sensitive moxibustion plus lactulose for postoperative constipation of mixed hemorrhoid due to spleen deficiency
- Therapeutic efficacy observation on auricular point sticking therapy for cardiac syndrome X in women
- Therapeutic observation of manipulation plus exercise therapy in treating upper crossed syndrome postures of primary school students
