Comparison of the corneal volume and the anterior chamber volume using Pentacam in individuals with healthy, subclinical and early keratoconus eyes
2020-05-08FarshadOstadianFereydounFarrahiAtefehMahdianRadMohammadSadeghMirdehghan
Farshad Ostadian, Fereydoun Farrahi, Atefeh Mahdian Rad, Mohammad Sadegh Mirdehghan
Abstract
•AIM: To compare the anterior chamber volume and corneal volume using Pentacam in people with early keratoconus, subclinical keratoconus, and healthy subjects.
•METHODS: This epidemiologic study was performed on 63 patients who were candidates for refractive surgery. We classified our patients into three groups as normal, subclinical keratoconus, and early keratoconus according to the Amsler-Krumeich criteria. We collected demographic information, including age and sex, and obtained a full medical history of the patients. Complete visual examination was performed for all patients. Then, using Pentacam, corneal volume and anterior chamber volume were measured among three groups.
•RESULTS: Corneal volume in the control group was significantly higher than the subclinical keratoconus and early keratoconus groups (P<0.05), but the anterior chamber volume was not significantly different between the groups (P>0.05).
•CONCLUSION: Measuring the corneal volume can help to distinguish the eyes with subclinical keratoconus and early keratoconus from normal eyes. The chamber volume might not differ remarkably among people with subclinical keratoconus, early keratoconus, and those with normal eyes.
•KEYWORDS:Pentacam; corneal volume; anterior chamber volume; keratoconus; subclinical keratoconus; early keratoconus
INTRODUCTION
Keratoconus is a non-inflammatory ectatic corneal disorder that is commonly bilateral and associated with irregular astigmatism and visual impairment.In keratoconus, corneal tissue changes in the central and paracentral regions lead to the development of an abnormal cone-like cornea[1]. These changes occur primarily in myopia eccentric steepening may progress towards central corneal scarring and severe corneal thickness reduction in advanced stages[2-4]. The incidence of keratoconus varies according to the geographical situation, different diagnostic criteria consideration, type of samples, and other factors. The Russian Federation (approximately 0.3 per 100, 000 people) and India (2300 per 100, 000 people) have reported the lowest and the highest incidence of keratoconus, respectively. In Iran, keratoconus prevalence was between 0.022 and 0.024%[2,5]. Although different studies are still ongoing to expand our knowledge about the pathogenesis of keratoconus, collagen degeneration following proteolytic enzyme activity and, consequently, differences in collagen content in the regions of the cornea is considered as one of the most important mechanisms for the pathogenesis of keratoconus[6]. A positive family history of keratoconus, ethnicity, mechanical damage to the cornea, allergy and some diseases such as Marfan syndrome are associated with the incidence of keratoconus, which indicates the role of both genetic and environmental factors in this regard[2,7]. Although keratoconus gradually progresses, diagnosis of keratoconus, especially in the early stages of the disease, is essential in preventing sudden vision impairment and preventing progression of the disease after refractive surgery[2,7-8]. Topography and tomography of the cornea are widely used non-invasive approaches for the evaluation of corneal morphology and the diagnosis of corneal diseases, especially keratoconus[9]. Several studies have shown that using the Scheimpflug imaging method, the physician can carefully evaluate the anterior and posterior surface of the cornea, calculate the thickness of the cornea and subsequently provide the corneal elevation map[2,9-10]. Some studies have shown that the parameters of the anterior segment may indicate differences in the very early stages of the keratoconus in patients and healthy subjects, and by evaluating these parameters it may be possible to diagnose keratoconus in the early stages[1,4,11]. Considering the remarkable accuracy of Scheimpflug imaging technique in assessing the anterior segment and corneal tissue parameters, as well as the importance of detecting the early stages of keratoconus, and also the differences in the results of some studies in this field, this study aimed to compare the anterior chamber volume and corneal volume in people with early keratoconus, subclinical keratoconus, and healthy subjects which can help in early detection of subclinical keratoconus.
SUBJECTS AND METHODS
This epidemiologic study was performed on patients who were candidates for refractive surgery and had been referred to Imam Khomeini Hospital, Ahvaz, Iran in 2017-2018. We used the nonprobability sampling method and calculated the sample as 63 individuals according to the previous studies. Inclusion criteria were: 1) adults aged 18 years and older; 2) candidacy for refractive surgery; 3) spherical myopia less than six diopters; 4) myopia and astigmatism (spherical equivalent) of less than eight diopters; 5) astigmatism less than four diopters. Exclusion criteria were: 1) history of any eye surgery; 2) contact lens usage; 3) corneal scarring or hydrops; 4) history of corneal edema; 5) keratometry > 53 diopters; 6) pregnancy or breastfeeding at the time of the study. The study protocol was permitted (IORC-9707) by Ethics Committee of Ahvaz Jundishapur University of Medical First, we collected demographic information, including age and sex usinga questionnaire and obtained a full medical history of patients. Complete visual examination was performed for all patients including measurement of uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) using the Snellen chart, corneal anterior chamber, iris, lens and anterior vitreous examination with a slit lamp biomicroscopy, retinal examination with a 90 D non-contact lens and intraocular pressure measurement using a Goldman applanation tonometer. Then, using Pentacam (Oculus, Lynnwood, WA, USA), we collected corneal imaging data at the mid-day time (from 10 a.m. to 2 p.m.) at least 2h after the patient was awake. If the results of eye examinations and Pentacam were normal and corneas were healthy, the patient was allocated to the control (normal) group. In patients with BCVA≥20/20 and suspicious findings on Pentacam, even if eye examination results were normal, the patient was dedicated to subclinical keratoconus group. The presence of BCVA ≤ 20/25, at least one criterion in topographic maps, abnormal slit lamp examinations, or abnormal findings in Pentacam were considered as the early stages of keratoconus. According to Amsler-Krumeich criteria, patients with keratoconus could be classified into three normal (with myopic astigmatism), the subclinical and the early stages of the astigmatism groups[12-13]. According to the above criteria, we classified only grades I and II as the early stages of keratoconus and accordingly we had 3 study groups consists of group 1 as control group, group 2 as subclinical keratoconus and group 3 as early keratoconus group.
Table 1 Demographic information of the study patients Sciences.

GroupsParticipantsFemaleMaleControl24168Subclinical keratoco-nus17611Early keratoconus221111Total633330
The analysis was done using IBM© SPSS Statistics for Windows© version 24.0. Armonk, NY: IBM Corp. The quantitative data were presented as the mean and standard deviation, and frequency and percentage were used to display qualitative information, in the form of the table. Pearson correlation coefficient, Mann-Whitney test, and one-way ANOVA test were used to compare the data.P<0.05 was considered a significant statistical threshold.
RESULTS
Of the 63 patients, 24 were in the normal group, 17 in the subclinical group and 22 in the early stage of keratoconus. Details of the demographic information are shown in Table1.
Corneal volume measured with Pentacam in the control group was significantly higher than the subclinical keratoconusand early keratoconus groups (P<0.05) but the anterior chamber volume was not significantly different among the groups (P> 0.05) (Table 2).
Table 2 Results of corneal volume and anterior chamber volume evaluation among the control, subclinical keratoconus and early keratoconus groups using Pentacam
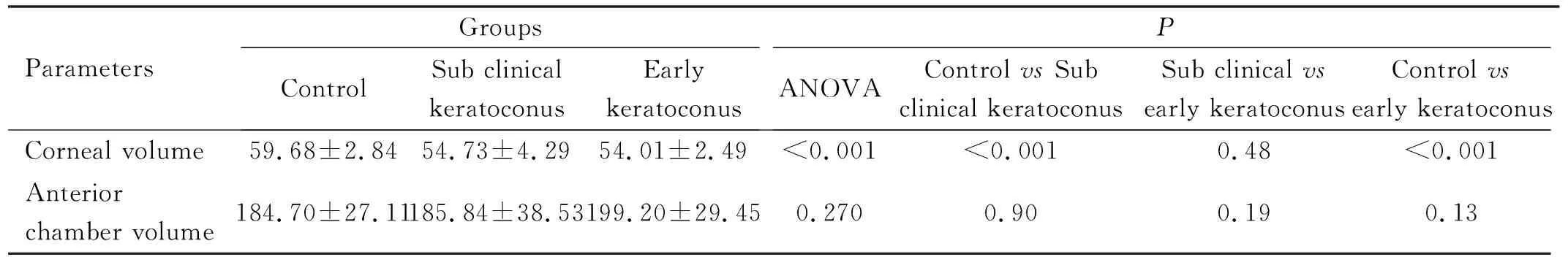
ParametersGroupsControlSub clinical keratoconusEarly keratoconusPANOVAControl vs Sub clinical keratoconusSub clinical vsearly keratoconusControl vsearly keratoconusCorneal volume59.68±2.8454.73±4.2954.01±2.49<0.001<0.0010.48<0.001Anterior chamber volume184.70±27.11185.84±38.53199.20±29.450.2700.900.190.13
DISCUSSION
The Pentacam technology has been used in various studies considering the superior accuracy in evaluating the corneal pachymetry and posterior corneal surface compared to the Placido-disk and scanning-slit systems, especially in cases where the patient has undergone corneal manipulation such as LASIK[3]. In this study, we evaluated corneal characteristics with Pentacam to distinguish subclinical and early keratoconus from normal cornea.
The results of our study demonstrated that mean corneal volume in the control group was significantly more than the subclinical and early keratoconus groups, but there was no significant difference between the subclinical keratoconus and early keratoconus concerning mean corneal volume. Regarding corneal volume and anterior chamber volume there was not particular area of the cornea that you measured consistently throughout.
Corneal imaging results in patients with keratoconus and healthy subjects performed by Safarzadehetal[14]revealed that corneal volume was higher in healthy subjects than suspected keratoconus, mild and moderate keratoconus, and the results found no significant difference among suspected keratoconus, mild and moderate keratoconus groups. Orucogluetal[15]also investigated the differences between the corneas of healthy individuals and keratoconus patients and observed that in healthy subjects, corneal volume was higher than those with keratoconus. According to Mannionetal[16]study, corneal volume in patients with keratoconus was significantly reduced in compared to the healthy subjects. Similarly, the study of Emreetal[4]also indicated that the corneal volume values were higher in normal subjects compared to patients with different stages of keratoconu. These results are similar to those of the study of Mas-Aixalaetal[1]In their study, the mean corneal volume in the keratoconus group was lower than that of the normal group. Similar to the previous studies, the study of Pieroetal[3]demonstrated that mean corneal volume in patients with keratoconus was significantly lower than healthy subjects. The results of all of the above studies are consistent with our findings and indicate the importance of corneal parameters in refractive surgery candidates. In the late stages of keratoconus, changes in the various layers of the cornea may be evident, but in the early stages of keratoconus, these changes are subtle and can be noticeable while there may not be many changes in the corneal parameters at the same time. This study and similar studies results challenges the studies that showed the low ability of Pentacam to detect very early stages of the keratoconus[16-18]. Although the thinning of the cornea is thought to be the cause of reducing the corneal volume in keratoconus, more investigations are required to clarify the mechanisms involved in this process.
The evaluation of the anterior chamber volume in our subjects revealed no statistically significant difference among the three groups, although this parameter was slightly higher in the early keratoconus group than in other groups. These results are consistent with Emreetal[4]findings. In their study, anterior chamber volume was not significantly different in the control group and the keratoconus group. No significant difference was found between the various stages of keratoconus, although the anterior chamber volume values were nearly higher in late stages of keratoconus. The evaluation of the anterior chamber volume in the study of Safarzadehetal[14]showed that this parameter was similar in normal individuals, suspected keratoconus and mild keratoconus patients, and as keratoconus progressed towards late stages, this parameter increased more significantly. Therefore, in the early stages of keratoconus, the anterior chamber volume was not significantly different from the normal eyes. These results are consistent with the findings of the study of Mas-Aixalaetal[1]. In their research, there was no significant difference between the normal and keratoconus patients regarding the mean anterior chamber volume. In a study of Alietal[11]50 normal individuals and 50 moderate keratoconus patients were examined, and the results indicated that the mean anterior chamber volume was higher in the moderate keratoconus group. This finding is similar to that of Orucogluetal[15], in their study, it was also observed that the mean anterior chamber volume in subjects with keratoconus was higher than normal individuals. In our study, the evaluation of anterior chamber volume by Pentacam did not find a significant differentiation between the early stages of keratoconus and subclinical cases as well as normal cases, and therefore the results of the last two studies mentioned earlier are not inconsistent with the findings of our research. However, their findings indicate the effectiveness of Pentacam in evaluating the anterior chamber volume to distinguish normal and more advanced stages of keratoconus. Also in our previous study we showed in patients with subclinical keratoconus, the corneal epithelial thickness increases to mask the thinning of stroma thus corneal epithelial map uniformity indices scans (S-I; SN-IT; T-N) could help early diagnosis of the subclinical keratoconus and differentiating them from normal eyes[19]which can be consider in association with results of this study to increase the ability of subclinical and early keratoconus detection.
One of the important limitations of the present study is the relatively low sample size and single center sampling. Besides, due to the lack of cut-off point for the differentiation of subclinical keratoconus and normal corneas, there might be a chance that some patients in subclinical keratoconus group have been wrongly allocated. Therefore, one should approach these results with caution and further studies in the future should be conducted, taking into account the above limitations.
Measuring the corneal volume can help to distinguish the eyes of subclinical and early keratoconus from normal eyes. The anterior chamber volume not differ remarkably between people with subclinical and early keratoconus, and those with normal eyes.
