Eight years experience with botulinum toxin A and eyelid surgery in the treatment of hemifacial spasm
2020-05-08KennethLaiAndrewKukEdwinChanSimonKo
Kenneth K.H. Lai, Andrew K.T. Kuk, Edwin Chan, Simon T.C. Ko
Abstract
•AIM: To report the therapeutic outcomes of botulinum toxin A (Botox) and eyelid surgery in patients with hemifacial spasm (HFS).
•METHODS: Patients’ images and medical notes were retrospectively reviewed with subsequent analysis of both the therapeutic outcomes and complications of Botox injections.
•RESULTS: The information of 76 patients (Female=58) with HFS who received a minimum of 4 Botox injections were included. The mean follow-up interval was 83±50 (20-112)mo with an average of 16±10 (4-34) injections. The peak incidence was between 55 and 64 years and the average age of onset was 66±11 (32-85) years. Up to 23% of patients with HFS had aberrant vascular structures (Right=8, Left=7) in close relationship to the facial nerve (MRI=14, CT=1), where the vertebral artery (n=6) was the most involved vessel followed by the anterior inferior cerebellum artery (n=5). Patients with primary HFS had a shorter effective duration (2.5 vs 3.1mo, P<0.05), a longer onset time (4.1 vs 3.8d, P=0.739) and a lower Subjective Spasm Alleviation score (SSAs) (1.7 vs 1.9, P=0.179) than those with secondary HFS. Twelve of the 19 patients with pre-existing eyelid diseases underwent surgical correction including upper blepharoplasty (n=12), limited myectomy (n=7), browplasty (n=7) and advancement of levator aponeurosis (n=5). Five (41.7%) of those with surgical correction and suboptimal response to Botox showed improvement 6mo after surgery [onset time (P=0.0256), effective duration (P=0.374) and SSAs (P=0.0161)]. Those 12 patients with eyelid surgery had a lower complication rate than those without eyelid surgery (23% vs 42%, P≤0.05).
•CONCLUSION: Botox is an effective and safe treatment for HFS. We found that patients with primary HFS had a less favorable therapeutic outcome with Botox than those with secondary HFS. Eyelid surgery for patients with concurrent eyelid diseases can augment the effect of subsequent Botox injections by improving patient satisfaction and reducing complication rate.
•KEYWORDS:hemifacial spasm; botulinum toxin; botox; eyelid surgery; MRI
INTRODUCTION
Hemifacial spasm (HFS) is a form of dyskinesia with involuntaryclonic and/or tonic muscle contraction over the distribution of the facial nerve, which usually is unilateral and first involves the periorbital musculature[1]. Any damage along the facial nerve route can result in HFS. Primary HFS is caused by the presence of aberrant vascular structures compressing the root of the facial nerve where it exits the brainstem[2]. Secondary HFS causes include cerebellopontine angle tumors, arteriovenous malformations and brainstem vascular insults[3].
The prevalence of HFS increases with age and has a female preponderance[4]. Asian populations have been reported to have a higher prevalence[5]and an earlier age of disease onset[6]. As mentioned, primary HFS is associated with the presence of aberrant vessels at the root exit zone of the facial nerve[16]and was first reported by Campbelletal[8]in 1947. In contrast, Tashetal[9]reported that MR images detected facial nerve contact with vascular structures in up to 21% of patients who remained asymptomatic. A recent report[21]showed that secondary HFS has a milder intensity of disease than primary HFS, and that determining the types of HFS based on the demographic and clinical features[22]can be challenging.
HFS can result in serious ophthalmic complications such as corneal abrasion and functional blindness. Botulinum toxin was reported as a safe and effective treatment of HFS[11]and is now widely accepted[13]as the first line treatment of HFS and blepharospasm[14-15,21]. Frequently reported ophthalmological adverse reactions[12]include ptosis, diplopia and weakness causing asymmetry of the face[20]. In our study, we aim to report the demographic and radiological features as well as the long term treatment outcome of botulinum toxin A (Botox) among patients with primary and secondary HFS. We also look into the effects of eyelid surgery in the therapeutic outcomes of Botox in our patients with HFS over an 8 year interval.
SUBJECTS AND METHODS
This retrospective review study was approved by the Hong Kong East Cluster Research Ethics Committee of the Hospital Authority (REC Ref. No: HKECREC-2019-016). This study followed the Declaration of Helsinki. The information of 108 consecutive cases referred to our Botox injection clinic from 2010 to 2018 were reviewed. Only patients with a clinical diagnosis of HFS and had received at least 4 Botox injections were included into the statistical analysis.
Procedure records, medical notes and radiological images were reviewed. During each Botox injection clinic session the onset time, duration of effect, post injection complications and the degree of improvement were documented by our oculoplastic surgeons. The degree of subjective treatment outcome was measured using the Subjective Spasm Alleviation score (SSAs) which involves self-evaluation of the impact on activities of daily living (ADL): 0=Severe effect on ADL, 1=Partial effect on ADL, 2=No effect on ADL.
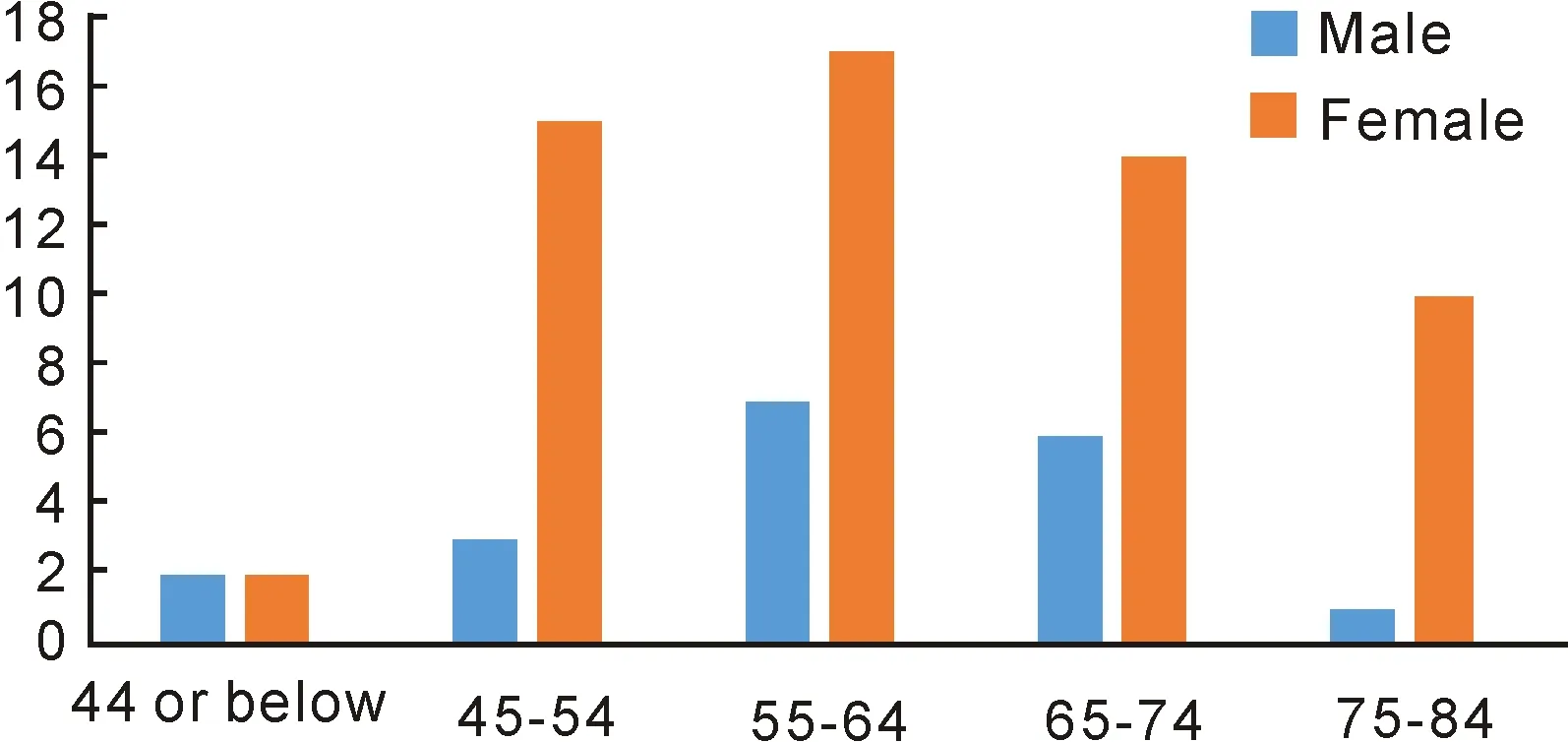
Figure 1 Number of patients with HFS of different age groups.
Table 1 Common conditions associated with HFS

Itemsn=76Bells Palsy11 (14%)Psychiatric conditions8 (11%)Parkinsons disease2 (3%)Dementia2 (3%)
HFS: Hemifacial spasm.
All patients received the same brand of Botox product from Allergan. 2.5 mL of 0.9% non-preserved sterile saline was mixed with the Botox product. 5 units of Botox were injected at each site according to the location of muscle spasm. The pretarsal portion of the orbicularis oculi muscle was the preferred injection site and the levator palpebral superioris muscle was avoided. All patients were regularly monitored ever 4 to 5mo. Patients with upper eyelid surgery for pre-existing eyelid diseases were sub-analyzed. Limited myectomy was defined as the stripping of both preseptal and pretarsal orbicularis oculi muscle from 1 cm lateral to the medial canthal angle to 1 cm medial to the lateral canthal angle, and every visible muscle fiber exposed after the removal of the redundant skin were excised completely. Complete myectomy surgery was not performed in our center. Test of significance was performed with Chi square test, 2-tailed pairedt-test and 2-tailed unpairedt-test withP<0.05 as significant value and a confidence interval of 95%.
RESULTS
The information of 76 patients diagnosed with HFS and who had received at least 4 Botox injections were included in our study. The average age of HFS onset was 66±11 (32-85) years with a female to male ratio of 58:18. The laterality showed 45 (59%) patients that manifested on the right side. The incidence among our different age groups are summarized in Figure 1. The mean follow up duration was 83±50 (20-112)mo. Conditions associated with HFS in our population are summarized in Table 1.
Treatment Outcome of Botox The average number of Botox injection per patient received was 16±10 (4-31) and the average dosage per session ipsilaterally was 24±26 (15-50) units. The average onset time was 3.8+/-2.6 (1-20)d, the average duration of effect was 2.9±1.0 (0.5-5)mo and the average SSAs was 1.9±0.4 (0-2). Thirty (40%) patients experienced at least one episode of post Botox injection complications and the details are summarized in Figure 2.
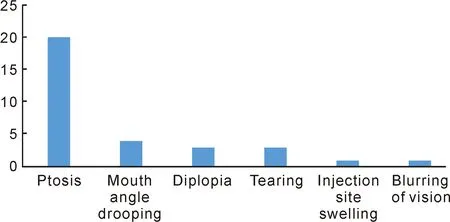
Figure 2 Numbers of patients among different post Botox injection complications.
Radiological Features All 72 brain images from 66 (86.8%) patients were reviewed including 24 magnetic resonance imaging (MRI) (Angiogram=6) and 48 computed tomography (CT) (Angiogram=1). Primary HFS was diagnosed in 15 (23%) patients with images of aberrant vascular structures (Right=8, Left=7) in close relationship with the facial nerve route, and 14 of them were diagnosed with MRI images. The vertebral artery was the most commonly involved vessel (n=6) (Figure 3). One patient had microvascular decompression of the anterior inferior cerebellar artery (AICA) 17 years ago without improvement of facial spasm. The types of aberrant vascular structure are summarized in Table 2. Twenty (30%) patients had small vessel disease of the brainstem and 3 of these had both small vessel disease and aberrant vascular structures. One patient was diagnosed with acoustic neuroma and 1 patient had aneurysm of the anterior communicating artery (Figure 4). Seventeen (26%) patients had unremarkable brain images.
Outcome of Botox in Primary and Secondary HFS The patients with primary HFS had a younger average HFS onset age (60±11vs61±12 years old,P=0.850) and a higher female to male ratio (13:2vs35:16,P=0.168) than those with secondary HFS. The average dosage of Botox per injection ipsilaterally was lower in patients with primary HFS (24.8±9.86vs27.6±7.37,P=0.127). When we compared the treatment outcome of Botox injection, patients with primary HFS had a longer onset time of action of Botox (4.1±2.7vs3.8±3.0d,P=0.739), a shorter effective duration of Botox (2.5±1.2vs3.1±0.9mo,P<0.05), and a lower SCIs (1.7±0.6vs1.9±0.4,P=0.179) than patients with secondary HFS.

Figure 3 MRI demonstration of a patient with compression of the left facial nerve root exit zone from the left vertebral artery (red arrow).
Patients with Upper Eyelid Surgery Nineteen patients were diagnosed with eyelid diseases including dermatochalasis (n=18), brow ptosis (n=7), lower lid entropion (n=1). Twelve (15.8%) of them underwent upper eyelid surgery including upper blepharoplasty (n=12), limited myectomy (n=7), browplasty (n=7) and advancement of levator aponeurosis (n=5). No surgical complication was reported. The details of upper eyelid surgery are summarized in Table 3. When comparing the 12 patients with eyelid surgery to the 64 patients without eyelid surgery, the onset duration was shorter (3.21vs3.80d,P=0.226), and the average effective duration was longer (2.92vs2.88mo,P=0.495) among those with eyelid surgery. The average dosage of Botox given ipsilaterally per session was lower in those with eyelid surgery (24.8±9.9vs27.6±7.4,P=0.127) and the SSAs was also higher (1.92vs1.83,P=0.232). The patients with eyelid surgery had a lower risk of experiencing post injection complications [3 (23%)vs27 (42%) (P≤0.05)), where ptosis was the most common complication among both groups (with eyelid surgery=2, without eyelid surgery=18).
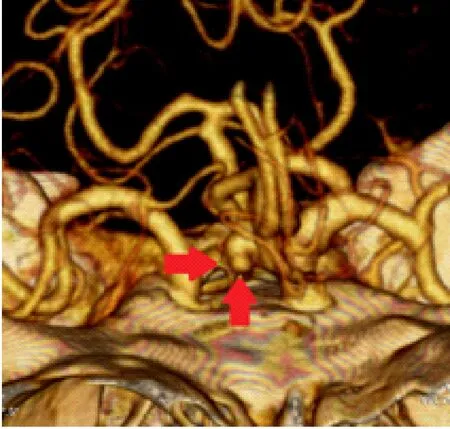
Figure 4 CT angiogram demonstration of left communicating artery aneurysm (red arrows).
Table 2 Types of aberrant vascular structures in close relationship with the facial nerve

Itemsn=15VA5AICA4NA3PICA2AICA+VA1
AICA: Anterior inferior cerebellum artery; PICA: Posterior inferior cerebellum artery; VA: Vertebral artery; NA: Non specific.
Five of the 12 patients received pre-eyelid surgery Botox injection with an average of 7 injection sessions and average Botox dosage of 25 units (20-30) per session ipsilaterally. Both the average mean onset time (2.3vs5.0d,P=0.0256) and the average effective duration had improved (3.2vs3.0mo,P=0.374) after upper eyelid surgery. Despite the average Botox injection dosage remaining the same [25 units (20-25) per injection ipsilaterally] the SSAs improved significantly (2.0vs1.2,P=0.0161). Three patients experienced post injection complications before surgery and none experienced post injection complications after upper eyelid surgery with an average number of Botox injection sessions of 6.6 over an average of 30mo follow up (P=0.0705).
Table 3 Information of patients with eyelid surgery

Pa-tients GenderAge, aEyelid surgeryPre ES surgery onset time, dPost ES onset time, dPre ES duration of action, moPost ES duration of action, moPre ES SCIS(0-2)Post ES SCIS(0-2)1F63UEB+LM+BPNA7NA3NA12F59UEB+LM+BP+ALANA3NA3NA23F68UEB+LM+ALA4333224M51UEB+LM+BPNA3NA2NA25F59UEB4333126F59UEB+BPNA3NA2NA27F53UEBNA3NA3NA28F73UEB+LMNA4NA3NA29F65UEB+BP+ALANA4NA3NA210M56UEB+LM+ALA51.5231211M69UEB+LM+BP32331212F80UEB+LM+BP+ALA424412
ALA: Advancement of levator aponeurosis; BP: Browplasty; LM: Limited myectomy; SCIS: Subjective clinical improvement score; UEB: Upper eyelid blepharoplasty; ES: Eyelid surgery.
DISCUSSION
In this evaluation of 76 patients with HFS, the average age of disease onset was 65 years and the incidence peaked between 55 years and 64 years. It showed a strong female preponderance with a female to male ratio of 26∶9. Our data showed comparable data to the local Hong Kong study by Kwanetal[11]where the peak age incidence was between 50 years and 60 years. Both Hong Kong studies showed a higher peak age than the Beijing study[6]which was between 41 years and 50 years. The female to male ratio of our data was higher than both Kwanetal[11]and Wangetal[6]of 1.9∶1 and 1.8∶1, which is similar to Caucasian populations[4]. Only 1 patient had bilateral HFS, which is similar to the data published by Tanetal[18]where only 1.65% of their patients had bilateral HFS. Our patient had a normal CT finding in contrast to the patients reported by Tanetal[18]who both had neurovascular contact of the root exit zone of the facial nerve on MRI/angiogram.
Approximately a quarter of our patients with brain CT/MRI showed aberrant vascular structures in close relationship with the facial nerve and they were defined as primary HFS. The most common involved vessels were the AICA and VA, which was comparable to the findings reported by Hitchonelal[10]indicating that the vertebral artery was the most commonly involved vessel. However the VA has also been reported to be the least common involved vessel[7].
Fourteen of the 15 patients with aberrant vascular structures in our population were detected by MRI. However, Tash[9]reported that facial nerve vascular structure contact also existed in asymptomatic patients. From our study we cannot conclude whether the presence of aberrant vascular structures contribute to the pathology of primary HFS. Microvascular decompression was reported to be an effective treatment of HFS, up to 90% of cases achieved total relief of spasm[17,19]. We suggest patients with suboptimal responses to injections to consider early MRI, and if aberrant vascular structures are present to then be referred earlier to neurosurgical colleagues for microvascular decompression.
Botox is an effective treatment for HFS with up to 85% patients achieving complete relief of facial spasm with minimal disturbance of ADL. However, we aware that the average effective duration was under 3mo for most patients. Flexible treatment regimen of Botox injection might give a better subjective improvement of symptoms in HFS when compared to the fixed treatment regimen[23]. We suggest that an individualized follow up interval length based on the effective duration might be beneficial to patients with HFS.
Our data suggested that patients with aberrant vascular structures had a longer onset time of action, a shorter effective duration and a lower SSAs than those without aberrant vascular structures, despite being statistically insignificant. Colosimoetal[22]showed that patients with secondary HFS have a milder intensity of disease and our results supported that patients with secondary HFS showed better response to Botox than primary HFS without significant difference in dosage of Botox received. Our data showed that patients of both primary and secondary HFS shared similar age of disease onset and sex distribution comparable to a multicenter study[22]in Italy where both primary and secondary HFS share common demographics to our population. Patients with suboptimal response to Botox injection should undergo early MRI and alternative treatment options might be beneficial to them. Five patients with suboptimal response to Botox injection as defined by the duration of effective period shorter or equal to 3mo or poor subjective symptomatic control had upper lid surgery and significant improvement of treatment outcome in terms of both subjective (SSAs) and objective (onset time) measures were reported. Patients who respond poorly to Botox should actively look for the presence of pre-existing eyelid conditions such as brow ptosis, dermatochalasis and entropion. These conditions were prone to post Botox injection ptosis and upper eyelid surgery may be able to improve the satisfaction of Botox injection usage.
We recognize that the retrospective nature of this study may involve recall bias,although thorough documenting of information provided by our patients at the time of injection was attempted to minimize this. Three oculoplastic surgeons were involved in the administration of Botox injections and surgical techniques may have varied. We also recognize that some variability of follow up interval between patients exists in our data.
Botulinum Toxin is a safe and effective treatment for hemifacial spasm. We found that patients with primary HFS had a less favorable therapeutic outcome than those with secondary HFS and earlier MRI should be arranged in those with suboptimal responses to allow for alternative surgical intervention to be planned sooner. We propose that surgical correction of those with eyelid diseases can not only improve the eyelid function but they can also reduce the rate of complications as well as improve the efficiencies of subsequent Botox injections. This is of particular importance to patients with pre-existing eyelid conditions such as dermatochalasis and ptosis with previous suboptimal response to Botox injections.
