Dental stem cells:The role of biomaterials and scaffolds in developing novel therapeutic strategies
2020-04-30
Cornelia Larissa Granz, Ali Gorji, Epilepsy Research Center, Westfälische Wilhelms-Universität Münster, Münster 48149, Germany
Ali Gorji, Department of Neurosurgery and Department of Neurology, Westfälische Wilhelms-Universität, Münster 48149, Germany
Ali Gorji, Shefa Neuroscience Research Center, Khatam Alanbia Hospital, Tehran 1996836111,Iran
Ali Gorji, Neuroscience Research Center, Mashhad University of Medical Sciences, Mashhad 9177948564, Iran
Abstract Dental stem cells (DSCs) are self-renewable cells that can be obtained easily from dental tissues, and are a desirable source of autologous stem cells.The use of DSCs for stem cell transplantation therapeutic approaches is attractive due to their simple isolation, high plasticity, immunomodulatory properties, and multipotential abilities.Using appropriate scaffolds loaded with favorable biomolecules, such as growth factors, and cytokines, can improve the proliferation, differentiation, migration, and functional capacity of DSCs and can optimize the cellular morphology to build tissue constructs for specific purposes.An enormous variety of scaffolds have been used for tissue engineering with DSCs.Of these, the scaffolds that particularly mimic tissue-specific micromilieu and loaded with biomolecules favorably regulate angiogenesis, cell-matrix interactions, degradation of extracellular matrix, organized matrix formation, and the mineralization abilities of DSCs in both in vitro and in vivo conditions.DSCs represent a promising cell source for tissue engineering, especially for tooth, bone,and neural tissue restoration.The purpose of the present review is to summarize the current developments in the major scaffolding approaches as crucial guidelines for tissue engineering using DSCs and compare their effects in tissue and organ regeneration.
Key Words:Cell transplantation; Regenerative medicine; Tissue engineering; Neural crest;Angiogenesis; Biomolecules
INTRODUCTION
Stem cells are undifferentiated cells with self-renewing and clonogenic capabilities,which can differentiate into various cell lineages.According to the basis of their origin,stem cells are categorized as embryonic, induced pluripotent stem cells (iPS), and adult (tissue-specific) stem cells[1-3].Based on their differentiation potential, stem cells can be classified as totipotent (the ability to give rise to all types of cells), pluripotent(the potential of the cells to produce any type of cells in the organism), multipotent(the potential to give rise to cells of their tissue of origin), oligopotent (the potential to differentiate into only a few cell types), and unipotent (the ability to produce one cell type)[4].Embryonic stem cells are pluripotent, whereas adult stem cells are limited to differentiating into various cell types of their original tissue (multipotent).iPS are pluripotent cells that originated from somatic differentiated cells after transduction.Adult stem cells exist in different tissues and organs, such as the bone marrow, blood vessels, peripheral blood, and skeletal muscles as well as the brain, heart, skin,intestine, liver, gonads, and teeth[5-7].
Human mesenchymal stem cells (MSCs), which are multipotent non-hematopoietic progenitor cells, have been isolated from both adult and fetal tissues, such as the bone marrow, adipose tissue, endometrium, bone, muscle, umbilical cord, blood, Wharton's jelly, and amniotic fluid as well as nervous and dental tissues[8].Human MSCs have the potential to differentiate into both mesodermal (osteocytes, adipocytes, and chondrocytes) and non-mesodermal (endodermal and ectodermal) lineages(hepatocytes and neuronal cells)[9]with both anti- and pro-tumorigenic properties[10]as well as a limited risk of inflammatory reactions and uncontrolled growth[11].The source of MSCs has a crucial role in the outcomes of stem cell-based tissue engineering[12].Dental stem cells (DSCs) are neural crest-derived cells that can be obtained easily from dental tissues of both adults and children; therefore, they are a reliable, accessible source of autologous stem cells[13,14].DSCs are undifferentiated cells that have non-limited self-renewal, multipotent differentiation potential, and colonyforming capacity[15].DSCs can be isolated from the dental pulp of deciduous, natal, and permanent teeth, the periodontal ligament, the apical papilla, the dental follicle, and gingival tissue (Figure 1)[16,17].One of the unique characteristics of DSCs is their ability to differentiate into mesodermal, ectodermal, and endodermal cell lineages[18].DSCs from each source are capable of specifically differentiating into various distinct cells,including epithelial cells, odontoblasts, osteoblasts, chondroblasts, adipocytes,vascular cells, endotheliocytes, neuronal cells, glial cells, photoreceptor cells, and muscle cells[19,20].Although all stem cells obtained from various sources are named DSCs in this study, their phenotype, differentiation potential (both inin vitroandin vivoconditions) and functional properties (such as biological response during differentiation and tissue repair) are different[21].For instance, stem cells obtained from the apical papilla possess greater proliferation ability, express a higher variety of neural markers, and induce more uniform dentine-like tissues compared to dental pulp stem cells[22-24].Furthermore, DSCs isolated from exfoliated deciduous teeth exert a higher capacity for osteogenic regeneration and a greater proliferation rate compared to dental pulp stem cells[25].DSCs isolated from pulp tissues are the first and most frequent cells evaluated for their odontogenic, osteogenic, and neurogenic differentiation potentials[26].This heterogeneity of DSCs is effectively modulated by the function of their microenvironment[27].DSCs obtained from different sources exhibit various patterns of cell surface markers (Table 1)[28-31].
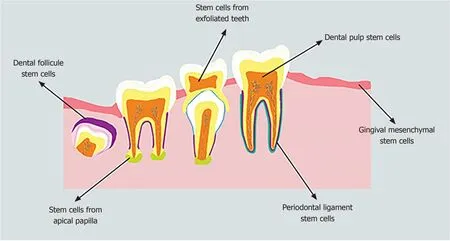
Figure 1 Schematic diagram of different sources where dental stem cells can be isolated.
DSCs secrete numerous immunomodulatory mediators, such as interleukin (IL)-6,IL-10, IL-1β, interferon-γ, and tumor necrosis factor-α as well as transforming growth factor-beta (TGF-β), hepatocyte growth factor, and vascular endothelial growth factor(VEGF)[32], and do not express the major histocompatibility complex class II antigen[33],which suggests their potential in the regulation of immune responses to promote tissue regeneration[34].DSCs from different sources may exert their immunomodulatory properties through the suppression of T-cell proliferation and lymphocyte activity as well as the activation of T-cell apoptosis[34,35].
The fate of the stem cells (proliferation and differentiation) is regulatedviaa combination ofintrinsicandextrinsicmechanisms.Intrinsic mechanisms consist of various transcription factors expressed by the cells.Extrinsic mechanisms are signals provided by the dynamic microenvironment (or “niche”), including the extracellular matrix (ECM), signaling molecules (such as growth factors and hormones), and neighboring cells[36,37].The microenvironment, which is a three-dimensional (3D)structure surrounded by specific cells and ECM, protects stem cells from inappropriate differentiation, cell damage, and apoptosis and governs tissue maintenance,regeneration, and repair[38,39].In addition to providing a physical microenvironment for cells, the ECM gives the tissue its mechanical properties (elasticity and rigidity),provides bioactive molecules and cues to residing cells, and establishes an environment to facilitate tissue remodeling in response to dynamic processes, such as wound healing[40].Furthermore, the ECM is produced and arranged by tissue-resident cells and secreted into the surrounding environment to provide support to the stem cells with its bioactive compounds[41].Stem cell behaviors are reciprocally regulated by the ECM and signals from the surrounding cells and molecules.Furthermore,inorganic ions, such as calcium and magnesium, as well as metabolic products, such as oxygen drive metabolites, and maintain stem cell fate[42].
The nature of the stem cell microenvironment differs in various tissues.In teeth, a particular microenvironment exists at specific anatomic sites that regulates the behavior of DSCs[39].Two different stem cell microenvironments have been identified in teeth; (1) the pulp cell-rich zone; and (2) the perivascular and perineurium of the dental pulp.The pulp is composed of four distinct zones; an outermost layer containing the odontoblasts, a cell-free zone (zone of Weil) with no cells and rich in the ECM, the cell-rich zone contains stem/progenitor cells, and the pulp core.Dental pulp tissue is populated by odontoblasts, fibroblasts, dendritic cells, macrophages, and progenitor cells, whereas the pulp core contains dental pulp cells, vessels, nerves, and ECM[43].The induction of odontoblasts, the biological cells of neural crest origin that survive throughout life, occurs during tooth development.However, under appropriate conditions, DSCs can differentiate into pre-odontoblasts and later secretory odontoblasts, which actively participate in reactionary dentinogenesis[44].
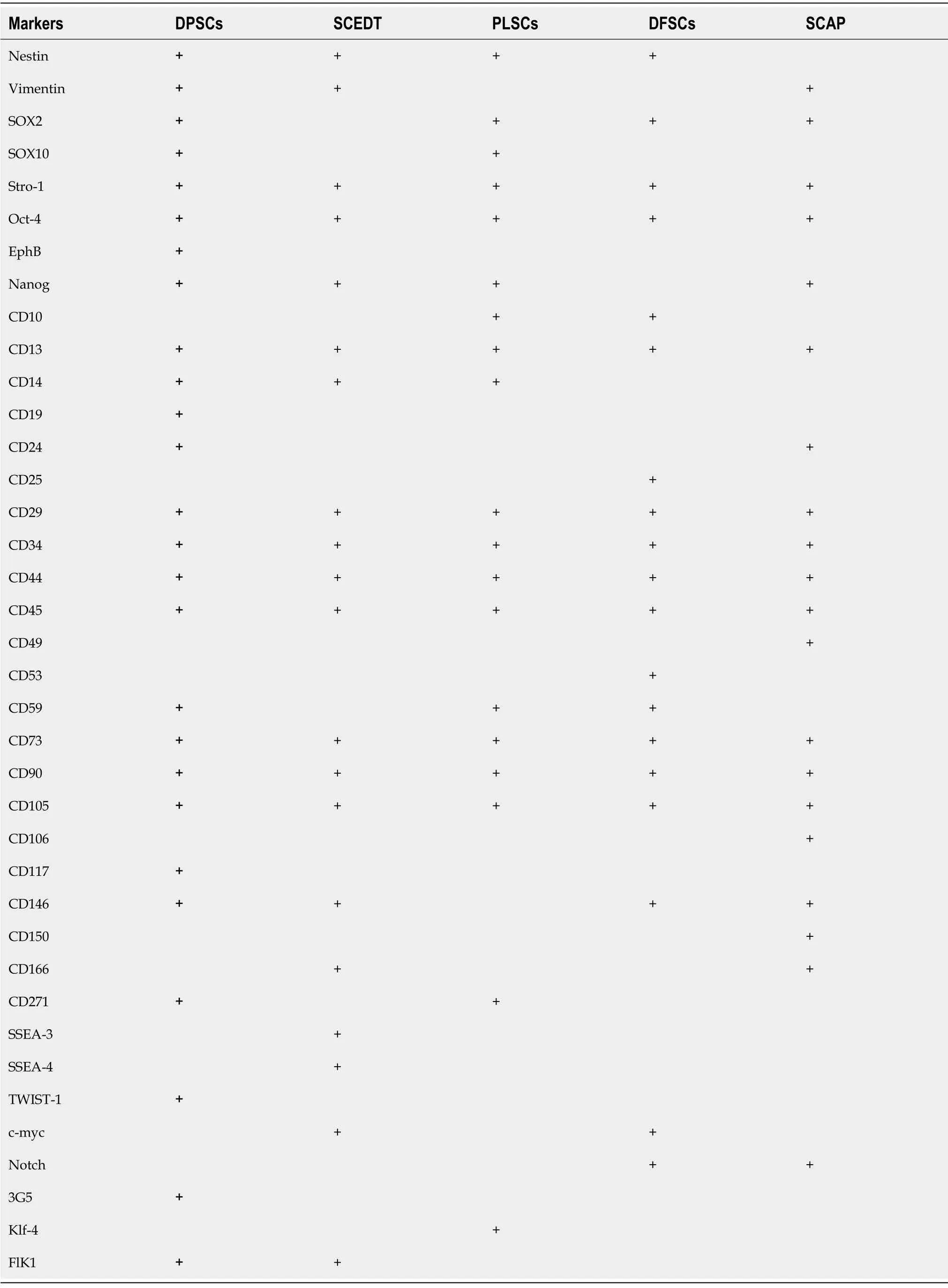
Table 1 Dental stem cells obtained from different sources exhibit various patterns of cell surface markers
Odontoblasts produce the main part of the ECM components of dentin and are involved in dentin mineralization[45].The dentin ECM consists of collagen(approximately 90%; Type I, III, and V), proteoglycans (such as chondroitin sulfate and heparan sulfate), growth factors [such as TGF-β and bone morphogenetic protein(BMP)], and enzymes (such as matrix metallopeptidase 1, 2, 3, 9, and 20)[46].In the dental pulp, DSCs also reside in perivascular and perineurium regions[47], which can be identified by aldehyde dehydrogenase-1 expression[48].The EphB/ephrin-B signaling pathway reciprocally modulates the attachment and migration of DSCs originated from the perivascular nicheviathe mitogen-activated protein kinase pathway and phosphorylation of Src family tyrosine kinases[49].
Pointing to the importance of ECM in maintaining homeostasis for proliferation and differentiation of DSCs, several studies have indicated that reconstruction of the appropriate microenvironment and boosting its interaction with stem cells are essential steps to successful cell therapy[50].The application of DSCs in stem cell therapeutic approaches is attractive due to their simple isolation and efficient administration[51].The multi-lineage capacity of DSCs differentiation to various tissues and organs suggests their greater ability than other adult stem cell populations for the treatment of different diseases[52].There is an enormous amount of evidence to indicate that DSCs have great potential for therapeutic cell approaches in various diseases,including liver disease, diabetes, myocardial infarction, ophthalmologic diseases,muscular dystrophy, Alzheimer’s disease, Parkinson’s disease, cerebral ischemia, and spinal cord injury[53].Furthermore, several studies have explored the potential of DSCs in the treatment of caries, periodontal disease, oral and maxillofacial defects, and alveolar bone atrophy[54,55].DSCs possess strong immunomodulatory abilities, which suggest that they are a favorable cell source for cell transplantation therapy in inflammatory disorders[33].It has been shown that DSCs are more beneficial for axonal regeneration than bone marrow stem cells due to their greater release of neurotrophic factors[56].Despite these extensive efforts, several essential parameters still need to be optimized for the clinical use of DSCs in cell transplantation therapy.One of the key challenges is the lack of an appropriate stem cell microenvironment, which leads to short-term survival of DSCs after implantation.To increase cell viability, transplanted cells require particular 3D structures with specific ECM components that protect DSCs from cell damage, maintain the stem cell homeostasis, and promote mutual biological information transfer between stem cells and the ECM[50,57,58].A large number of investigations have been carried out to reconstruct the stem cell microenvironment to strengthen the viability, proliferation, and appropriate differentiation of the transplanted cells for successful cell therapy[59].In this context, ECM scaffolds can form a desirable microenvironment for DSCs, which serve as a more favorable template for tissue repair and reconstruction[60,61].In this review, we provide a critical overview of the role of different biomaterials used to deliver DSCs to damaged tissue and their applications to improve, restore, and maintain tissue or organ reconstruction.
DIFFERENT TYPES OF SCAFFOLD FORMULATIONS
The general concept of tissue bioengineering involves three essential components;identification of suitable stem cells, development of appropriate scaffolds, and induction of potent signals to repair or regenerate human cells, tissues, or organs[62].Biomaterials are essential components for the construction of scaffolds.Tissue bioengineering combines scaffolds with various types of stem cells to reconstruct damaged tissues (Figure 2).The application of appropriate scaffolds could improve DSCs proliferation, differentiation, adhesion, and migration, which may promote their ability to repair the injured tissues and regenerate functional organs[63].Acellular tissues, as well as natural and synthetic biomaterials, can be used as the primary source for generating scaffolds[64].Acellular tissue matrices, such as an acellular adipose matrix, are derived from animal or human tissues with all cells eliminated during manufacture[65].In addition, the amniotic membrane has been suggested as a suitable biological scaffold for the proliferation and transplantation of DSCs[66].Natural biomaterials consist of proteins (collagen, gelatin, fibrin, and silk) and polysaccharides(agarose, alginate, hyaluronan, polylactic acid, and chitosan) which tend to be biocompatible due to their cellular adhesion sites, such as Arg-Gly-Asp binding sequences, and the ability to degrade without releasing toxic substances.However,due to the variability of materials, limited mechanical properties, the risk of transmitting pathogens, and provoking immune reactions, their formulations need to be promoted for stem cell culture[67,68].Synthetic biomaterials, including polymer-based biomaterials (such as polycaprolactone, polylactic acid, poly-lactic-co-glycolic acid,polyglycolide, poly-e-caprolactone, and poly-ethylene glycol) and ceramic-based biomaterials (such as hydroxyapatite, bioactive glass, and calcium phosphate) display a better mechanical property, reproducibility, and electrical conductivity as well as a lower degradation rate[68-70].Furthermore, synthetic biomaterials possess the possibility of optimizing the chemical and physical properties of a scaffold for a particular application[71].Hydrogels, which are networks of hydrophilic polymers, can be manufactured from natural biomaterials (such as collagen, fibrin, proteoglycans, and hyaluronic acid) or synthetic polymers (such as self-assembly peptide molecules or poly-ethylene glycol)[37,72,73].Hydrogels provide tissue-like microenvironments with particular cellular signals, desirable biocompatibility, semi-permeable membranes, and cell delivery vehicles[74].Furthermore, a wide range of nanocomposite biomaterials has been assembled by merging nanomaterials within the polymeric matrix to promote the efficiency of bioactive scaffolds[75].
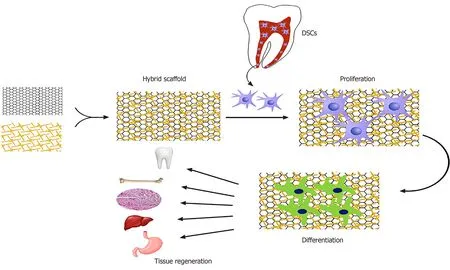
Figure 2 Schematic diagram of seeding dental stem cells on the hybrid scaffold, differentiation capability, and potential clinical applications for the regeneration of different tissues.
The desirable properties of a scaffold for stem cell transplantation are biocompatibility, biodegradability, mimic the 3D biological microenvironment,incorporation of different ECM, pore size, stability, electrical conductivity, porosity,non-immunogenicity, interconnectivity, safety (low or non-toxic) and alignment[70,76,77].Various fabrication techniques have been developed to produce different scaffolds,such as emulsion freeze-drying, electrospinning, thermally-induced phase separation,solvent casting/particular leaching, computer-aided design/computer-aided manufacturing, melt molding, rapid prototyping (3D printing, selective laser sintering,stereolithography, and fused deposition modeling), nanofiber self-assembly, and photolithography[78,79].The basic tissue engineering procedures consist of appropriate scaffold manufacture, hydrogel matrix support, and patterning design.The combination of these approaches promotes the development of the desired complex,both in tissue structure and function[20,80].
Scaffold-based cultures are conventionally applied in two-dimensional (2D)systems.Although 2D systems are a valuable medium for the investigation of basic cell biology and preclinical drug testing, data generated in these systems are insufficient to translate intoin vivoexperimental studies[81].Furthermore, inappropriate cell-to-cell and cell-to-ECM contacts, reduction of polarization, and alteration of key signaling pathways modulate stem cell differentiation ability[81,82].Thus, several 3D scaffold-based cultures have been developed.Although existing 3D cultures are not without limitations, they enhance cell viability, growth, differentiation, and migration and improve cellular communications[82].Combining DSCs with suitable scaffolds offers a promising strategy for cell delivery and transplantation.Two main approaches for this combination are cell-based and cell-free tissue engineering.In the cell-based approach, stem cells are seeded and cultured onto the scaffoldin vitroto produce the desired tissue before transplantation[83].In the cell-free approach, a bioactive scaffold with growth and differentiation factors is embedded in the respective tissues, induces the homing of resident stem cells, and promotes their proliferation and differentiation[84].
Furthermore, the environmental cues, such as various growth factors/morphogens,markedly affect the behavior of DSCs seeded in scaffolds and are vital to the success of regenerative therapies[85,86].Several proteins, such as BMP, sialoprotein, fibronectin,and osteopontin, are able to coat various types of biomaterials and promote the behaviors of DSCs[87].Pre-treatment of biomaterials with the abovementioned proteins could enhance adhesion, differentiation, proliferation, migration, and function of DSCs and improve the formation of new tissues[87,88].
DSCS IN COMBINATION WITH SCAFFOLDS FOR TISSUE RESTORATION
DSCs represent an auspicious cell source for tissue engineering, particularly for tooth,bone, and neural tissue reconstruction.A vast number of these investigations point to the importance of various scaffolds to design effective tissue engineering approaches(Table 2).
TOOTH RECONSTRUCTION
The therapeutic role of DSCs in combination with various scaffolds has been extensively investigated in restoring tooth damage or loss due to caries, periodontal disease, trauma, or genetic disorders[89].The procedure of dentin formation consists of odontoblastic deposition, vascularization, and neuron formation[20].Among multiple approaches to promote dentin formation and teeth tissue regeneration, the application of DSCs with a synthetic pre-designed and optimized scaffold is the most accepted technique for tooth regeneration[90].The appropriate scaffold can be implemented with DSCs and growth factors to induce the generation of dental tissues, which can integrate with the adjacent tissues[16].Scaffolds developed from either synthetic or natural biomaterials have been used for tooth reconstruction.Natural materials, such as collagen[91], chitosan/gelatin[92], silk protein[93], alginate[94], hyaluronic acid[95]as well as synthetic polymers, such as polyglycolate/poly-l-lactate[96], polycaprolactone-poly glycolic acid[97], polylactic acid-co-polyglycolic acid[98], polycaprolactone /gelatin/nano- hydroxyapatite[99], nano-hydroxyapatite/collagen/poly-l-lactide[100]and polyethyl methacrylate-co-hydroxyethyl acrylate[101]were used as scaffold materials for dental restoration and regeneration.Several investigations have indicated the regeneration of vascularized pulp-like tissue after subcutaneous implantation of tooth slices containing DSCs accompanied by an appropriate scaffold, particularly in the presence of growth factors such as dentin matrix protein[102,103].In several experiments,a combination of the abovementioned scaffolds was used to promote cell differentiation, vascularization, and safety as well as to reduce immunological and ectopic complications.The development of a vascularized dentin/pulp tissue in a subcutaneously transplanted human root canal containing a poly-lactic-co-glycolic acid scaffold seeded with DSCs has been reported[104].A scaffold consists of a pulpspecific ECM (an acellular ECM within the hydrogel) and an endothelial ECM(collagen-chitosan hydrogels) to promote odontogenic differentiation of DSCs and induce extensive vascularization in anin vivomodel of a tooth root slice[105].Comparing collagen and gelatin with chitosan, it has been stated that chitosan exerts weaker support for human DSCs growth and differentiation[106].In addition, 3D nano-fibrous gelatin/silica bioactive glass hybrid scaffolds provide a suitable microenvironment that mimics the architecture and composition of a natural dental micromilieu and enhances the growth and differentiation of human DSCs[107].Furthermore, the administration of human DSCs associated with acellular dental pulp resulted in pulplike tissue structures and the maintenance of ECM[108].DSCs seeded in 3D scaffold-free stem-cell sheet-derived pellets promote odontogenic differentiation[109].
The application of combined DSCs with the ECM scaffold can be used for root canal therapy.It has been shown that DSCs are able to differentiate into functional odontoblasts with angiogenic potential[110].Implantation of a 3D scaffold by shapingsheet-like aggregates of DSCs with a thermos-responsive hydrogel into the human tooth root canal generates pulp-like tissues with rich neovascularization without adding growth factors[111].Furthermore, transplantation of human DSCs with 3D hydroxyapatite scaffolds containing peptide hydrogels resulted in vascular ingrowth,osteodentin deposition, and pulp tissue formation in immunocompromised mice[112].Using bioengineered methods, it has been shown that it is possible to achieve functional teeth with entire roots[113].The nanofiber hydrogel PuraMatrix is a synthetic matrix that is used to create a biocompatible, biodegradable, and non-toxic 3D environment for a variety of cells[114].DSCs injected with PuraMatrix into full-length human root canals differentiate into functional odontoblasts; pointing to a novel strategy to facilitate root formation in damaged teeth[115].Severalin vitroandin vivostudies revealed that the addition of various signaling molecules and growth factors[such as granulocyte colony-stimulating factor (G-CSF), stromal cell-derived factor(SDF), basic fibroblast growth factor (bFGF), and VEGF] to different scaffolds (both natural and synthetic) enhances the regeneration of intra-canal pulp-like tissuesviathe promotion of dentine formation, mineralization, neovascularization, and innervation[116].DSCs transplanted with SDF-1 or G-CSF on a collagen scaffold promote pulp reconstruction in an animal pulpitis model[91,117].Autologous DSCs transplanted into a root canal with collagen types I and III associated with SDF-1 after pulpectomy in dogs significantly increased the expression of angiogenic and neurotrophic factors, indicating the potent trophic effects of the combined scaffold and chemokine on neo-vascularization during pulp regeneration[91].In addition, DSCs seeded into peptide hydrogel loaded with FGF-1, TGF-β1, and VEGF differentiated into odontoblasts-like cells and formed a vascularized dental pulp-like tissue inside the dentin cylinder[118].Moreover, TGF-β2 increased the odontogenic differentiation of DSCs isolated from the apical papilla[119].DSCs isolated from adult human tooth pulp and seeded on the surfaces of 3D collagen gel cylinders exhibited significantly increased cellular recruitment when applied with SDF-1α, bFGF, or BMP-7[120].Encapsulating TGF-β1 and FGF-2 in a biodegradable polymer of lactide and glycolide microspheres provides the controlled release of growth factors to human pulp cells[121].Furthermore, scaffold composition plays a key role in determining whether the application of signaling molecules or growth factors is needed.Various growth factors,such as SDF, FGF, TGF-β1, VEGF, and BMP were loaded on different scaffolds, such as peptide hydrogel, collagen, gelatin hydrogel, and alginate hydrogel, to enhance endodontic regeneration of DSCs[122].In addition, a silk fibroin scaffold loaded with bFGF has been described as a promising scaffold for the proliferation and differentiation of DSCsin vitro[123].Implantation of DSCs with poly-ε-caprolactone and hydroxyapatite in association with SDF-1 and BMP-7 generated tooth-like structures(putative periodontal ligament and new bone formation) in the mandibular incisor extraction socket[124].In addition to SDF-1, stem cell factor (SCF), a potent chemokine,enhances the mobilization and trafficking of stem cells[125].SCF promoted neovascularization and new collagen fiber formation after subcutaneous implantation of DSCs with a collagen sponge scaffold in mice.Furthermore, SCF improved DSCs migration, proliferation, and chemotaxisin vitro, possiblyviathe upregulation of ERK and AKT phosphorylation[126].
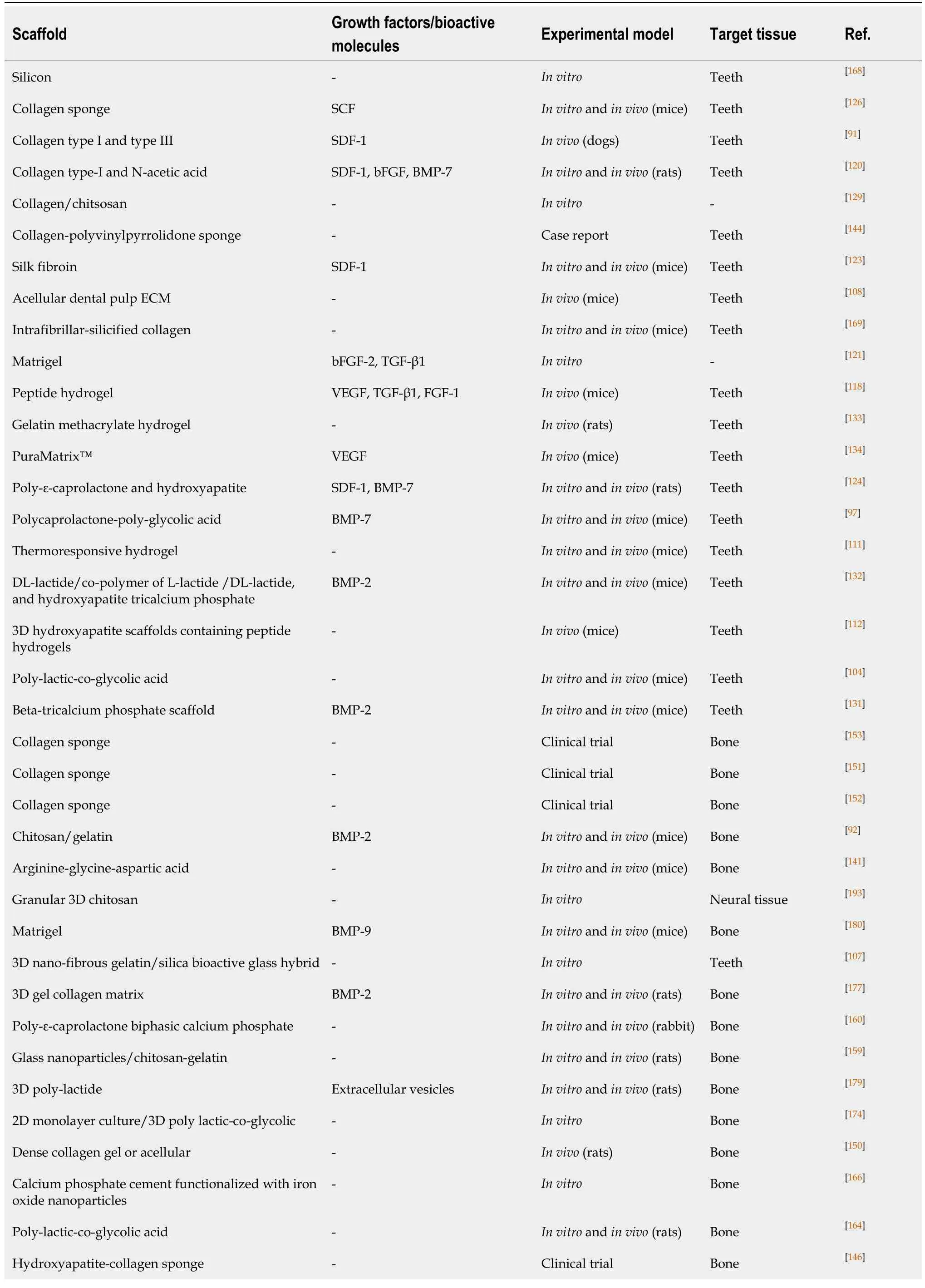
Table 2 A vast number of these investigations indicate the importance of various scaffolds to design effective tissue engineering approaches
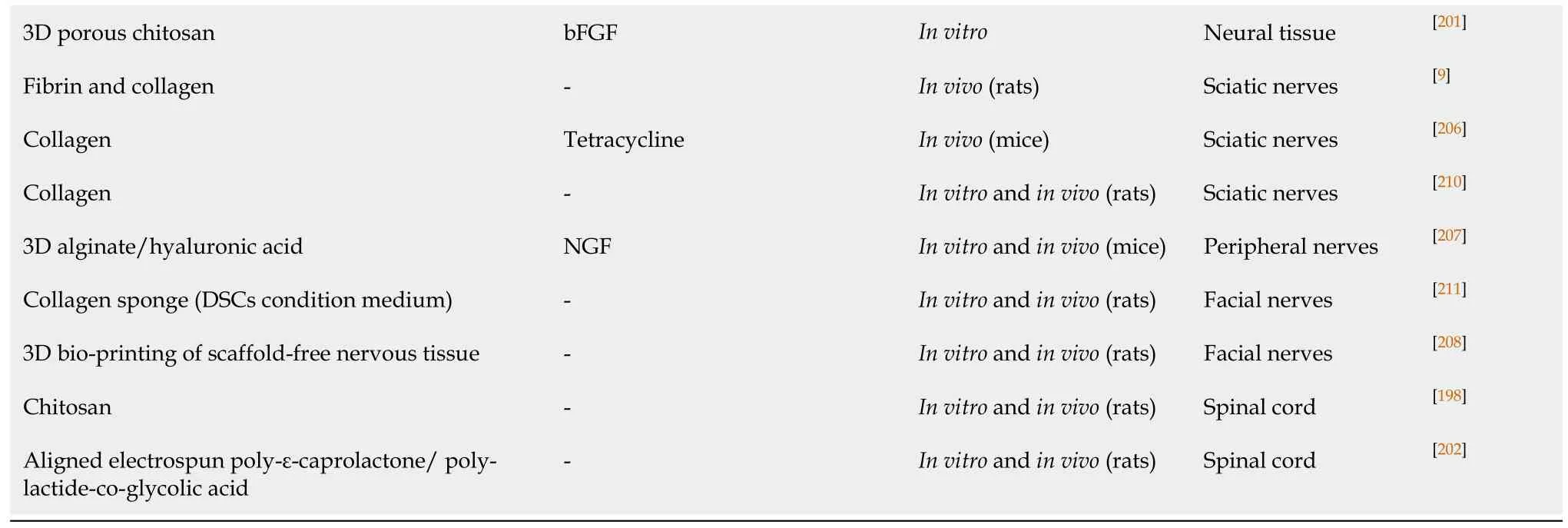
bFGF:Basic fibroblast growth factor; BMP:Bone morphogenetic protein; NGF:Nerve growth factor; SDF:Stromal cell-derived factor; SCF:Stem cell factor;TGF-β:Transforming growth factor beta; VEGF:Vascular endothelial growth factor; DSCs:Dental stem cells; BMP:Bone morphogenetic protein; ECM:Extracellular matrix.
Sialoprotein is a dominant non-collagenous protein in dentin, which plays a role in the induction of dental pulp cell differentiation into odontoblast-like cells and is essential for dental pulp stem cell identity and fate[127,128].Subcutaneous implantation of DSCs seeded on a 3D scaffold containing an acellular ECM embedded in a collagen/chitosan scaffold led to the production of dental pulp-like tissue and the expression of dentin sialoprotein in nude mice[129].The application of DCSs combined with treated dentin matrix, a biological scaffold, has been suggested as a suitable therapeutic approach for the reconstruction of the tooth root[130].Immortalized DSCs exhibited potent odontogenic differentiation ability and secreted dentin sialophosphoprotein when seeded in a beta-tricalcium phosphate scaffold and BMP-2 in nude mice[131].Among three different scaffolds (DL-lactide, co-polymer of L-lactide and DL-lactide, and hydroxyapatite tricalcium phosphate), a copolymer of L-lactide and DL-lactide showed the highest odontogenic regenerative capacity after the addition of DSCs and BMP-2[132].
A few studies have indicated that using a co-culture of DSCs with other stem cells improves neovascularization.The co-culture of DSCs and human umbilical vein endothelial cells with gelatin methacrylate xenogeneic hydrogel resulted in the neovascularization of mouse dental pulp[133].Transplantation of DSCs and human umbilical vein endothelial cells with VEGF seeded into PuraMatrix significantly enhanced vascularization and mineralization of mouse vascularized pulp-like tissue and osteodentin[134].In addition, using silk fibroin scaffolds promoted the ability of human DSCs in attracting vessels, which leads to the improvement of healing and regeneration of damaged tissues[135].Transplantation of DSCs with a tooth fragment/silk fibroin scaffold loaded with SDF-1 resulted in the generation of pulplike tissues with vascularity, organized fibrous matrix formation, and dentin formation in nude mice[136].
BONE RECONSTRUCTION
An enormous number of studies have been carried out to investigate the role of various scaffolds on the bone regeneration capacity of DSCs[137].The osteogenic differentiation ability of DSCs, mostly isolated from dental pulp or periodontal ligament, has been well demonstrated in bothin vivoandin vitrostudies[138].DSCs originating from dental pulp, dental follicle, gingival tissue, and periodontal ligament exert different osteogenic capacity[139], which can be modulated by various types of biomaterial scaffolds[140].For instance, anin vivoinvestigation has shown that DSCs from the periodontal ligament encapsulated in an arginine-glycine-aspartic acid tripeptide scaffold exhibit a greater ability to repair bone defects by promoting the formation of mineralized tissue compared to gingival MSCs[141].In addition, DSCs derived from the dental pulp exhibit great neovascularization potential while differentiating into osteoblasts, which subsequently promote bone restoration[142].
The most common scaffolds used to seed DSCs (particularly isolated from human dental pulp or exfoliated deciduous teeth) for bone tissue engineering in both experimental studies and clinical trials are collagen sponge membrane and hydroxyapatite/tri-calcium phosphate granules ceramic[143].DSCs seeded in collagen sponge scaffolds exhibit strong restoration ability in human mandible bone defects[144].The application of DSCs seeded onto a collagen-polyvinylpyrrolidone sponge scaffold in the left lower premolar region of a patient with periodontal disease increased bone density and decreased tooth mobility, periodontal pocket depth, and the bone defect area[145].Using DSCs with a hydroxyapatite-collagen sponge scaffold to fill the alveolar defect in 6 patients with cleft lip and palate resulted in satisfactory bone regeneration[146].A three-year clinical study revealed that the bone tissue regenerated following the application of human DSCs seeded on collagen scaffolds was uniformly vascularized and compact[147].However, this study revealed that the new bone developed at the implantation sites was compact and different from the normal spongy alveolar bone in the mandibles[147].In contrast, no ectopic bone formation was observed when DSCs were seeded on hydroxyapatite–tri-calcium phosphate scaffolds[148].Furthermore, it should be noted that for any successful cell transplantation approach, the optimal number of DSCs is essential.It has been demonstrated that dense culture conditions improve the mineralized nodule formation of DSCs and promote osteogenic-lineage commitment, possiblyviathe integrin signaling pathway[149].DSCs seeded in dense collagen gel scaffolds exert a higher beneficial effect on the craniofacial bone healing process compared to acellular scaffolds[150].
DSCs isolated from the dental follicle and the periapical papilla have been considered for the regeneration of alveolar bone and were successfully assessed in a few preclinical pilot studies.The application of dissociative dental pulp with a collagen sponge scaffold in patients with deep intrabony defects due to chronic periodontitis led to the effective restoration of defects with significant stability of the gingival margin[151].In addition, the application of DSCs seeded onto collagen sponge in the deep intrabony defects of 29 patients suffering from chronic periodontitis significantly improved clinical outcomes of the periodontal regeneration process[152].Another clinical trial has shown that using DSCs in combination with the collagen sponge scaffold in 6 patients resulted in a well-differentiated bone with Haversian system formation in the tooth extraction site[153].
Scaffold composition and surface properties play a key role in the osteogenic differentiation of DSCs and the process of bone tissue regeneration[142,154].Significantly greater mineralization occurred when DSCs were seeded into a collagen type I matrix[155].Furthermore, DSCs seeded on hyaluronic acid, fibrin, and polyesteramide type-C exhibit higher mineralization compared to standard tissue culture polystyrene[156].
Ceramic scaffolds, such as tri-calcium phosphate, hydroxyapatite, bioactive glass biphasic calcium phosphate, and calcium silicate, have chemical and structural similarities to the native bone and are commonly used as scaffolds to enhance bone regeneration and restoration of DSCs[157].The addition of tricalcium phosphate to the composition of the other scaffolds enhances the differentiation of DSCs into osteoblastlike cells[158].Chitosan/gelatin scaffolds significantly increased DSCs viability and differentiation as well as the formation of hydroxyapatite-rich nanocrystalline calcium phosphate in immunocompromised mice, particularly when cells were pre-treated with recombinant human BMP-2[92].Potent bone formation was observed in the defect area of rat femoral bone after application of DSCs seeded in bioactive glass nanoparticles/chitosan-gelatin bionanocomposite compared to mesoporous bioactive glass nanospheres[159].A combination of poly-ε-caprolactone biphasic calcium phosphate with DSCs increased the newly formed bone regeneration of calvarial defects in rabbit models[160].Furthermore, a combination of poly-lactic-co-glycolic acid with ceramics is usually used to enhance biomimetic potential and promote bone regeneration[161].Anin vitrostudy has revealed that human dental pulp SCs adhesion and proliferation, as well as their differentiation toward the osteogenic lineage, are significantly improved when seeded in hydroxyapatite (a member of the calcium phosphate-based bioceramics) and poly-lactide-co-glycolide[162].Implantation of human DSCs seeded in beta-tri-calcium phosphate scaffolds exerted an antiinflammatory effect and restored periodontal hard tissue defects[163].Greater bone regeneration was also reported when human DSCs were seeded on poly-lactic-coglycolic acid[164]and α- calcium sulfate hemihydrate/amorphous calcium phosphate[165]scaffolds.Calcium phosphate cement functionalized with iron oxide nanoparticles also exhibits a potent effect on the spreading, osteogenic differentiation, and bone mineral synthesis of DSCs, possiblyviaactivation of the extracellular signal-related kinases WNT/β-catenin pathway[166].
Different forms of silicon, particularly the orthosilicic acid form, promote osteoblast proliferation and differentiation, the mineralization process, and collagen production through enhancement of the precipitation of apatite from calcium and phosphatecontaining solutions[167].Semicarbazide-treated porous silicon exerted an appropriate scaffold for DSCs adhesion andin vivocell therapy, whereas silanization with aminopropyltriethoxysilane-treated porous silicon has been suggested as a favorable scaffold for a long-termin vitroculture system for DSCs proliferation and differentiation[168].Intrafibrillar-silicified collagen scaffolds markedly improved the proliferation, osteogenic differentiation, and mineralization capacity of human DSCs compared to non-silicified collagen scaffolds[169].A novel biocompatible nanoengineered osteoinductive and elastomeric scaffold fabricated from a porous nanocomposite of poly-glycerol sebacate and nanosilicates enhanced the physical integrity and mechanical strength of the cellular microenvironment forin vitroosteogenic differentiation and bone regeneration without persistent scaffold-related inflammationin vivo[170].
Hybrid composites are also used as promising biomaterials for bone regeneration.It has been suggested that four different scaffold materials, including porous hydroxyapatite alone or combined with three polymers polylactic-co-glycolic acid,alginate, and ethylene vinylacetate/ethylene vinylversatate, are suitable for DSCs osteogenic differentiation[171].Electrospun nano-ECM nanofibers with fluorapatite scaffolds enhance the growth, differentiation, and mineralization of DSCs[172], possibly mediatedviamodulation of the FGF and VEGF signaling pathways[173].Comparing the behavior of DSCs seeded on a 2D monolayer culture or 3D poly lactic-co-glycolic scaffold, it has been shown that DSCs exerted proper adherence and enhanced osteogenic differentiation on the 3D scaffold cultures[174].Furthermore, it has been suggested that DSCs seeded in hydrogel scaffolds have greater potential for odontogenic differentiation than cells embedded in collagen-I hydrogel scaffolds[175].Various layer-by-layer-modified gelatin sponge scaffolds increased the adhesion and proliferation of DSCs and enhanced their potential for bone tissue regeneration[176].
Several differentiation factors, such as BMP, were used to potentiate DSCs bone formation capacity.A 3D gel-based heparin-conjugated collagen matrix combined with recombinant human BMP-2 improved DSCs differentiation and seeding efficiencyin vitroand promoted the osteogenic differentiation of these stem cells to form ectopic bone formation in a rat model[177].Exfoliated human DSCs significantly increased the expression of BMP-2 and 7, bone and cartilage formation markers, when seeded in carbonate apatite scaffold in anin vivoalveolar bone remodeling model in rats[178].DSCs isolated from human gingival tissues seeded onto 3D poly-lactide scaffolds enriched with extracellular vesicles, small membrane vesicles containing various bioactive molecules, exhibited potent osteogenic inductivityin vitroand showed a marked improvement in bone healing of rat calvaria bone tissuein vivo[179].On the other hand, some biomaterial scaffolds may facilitate biomolecule-induced tissue formation.For instance, 3D matrigel scaffold enriched with DSCs led to enhanced BMP-9-induced osteogenesis and mineralization in ectopic bones in nude mice[180].
Although the majority of studies rely on the application of DSCs alone, several studies have employed co-culture systems (DSCs in combination with other cells)intending to promote bone regeneration, particularly in 3D scaffolds[181].Human DSCs and amniotic fluid stem cells seeded onto fibroin scaffolds resulted in pronounced bone repair associated with neovascularization in critical-size rat cranial bone defects[182].The co-cultured constructs of DSCs and endothelial cells seeded in 3D polycaprolactone blended with poly-L/D-lactide revealed a significantly higher upregulation of genes related to osteogenesis and angiogenesis[183].
NEUROLOGICAL DISORDERS
DSCs derived from dental pulp and oral mucosa display high expression of various neural crest-related and developmental genes[184].DSCs can be differentiated into the neuron-, Schwann-, glia-, and oligodendrocyte-like cells[185].Due to the high proliferative capacity and propensity to differentiate into neural stem cells, DSCs are attractive candidates for developing a human neuronal lineage for the treatment of various disorders[186].The role of DSCs in cell transplantation therapy of traumatic and hypoxic-ischemic injuries of the central or peripheral nervous system as well as neurodegenerative diseases has been extensively investigated[187].DSCs are promising sources for cellular transplantation-based therapeutic strategies for neurological disorders[188].The seeding of DCSs into different scaffolds promotes cell viability and differentiation towards neuronal-like cells[189,190].Scaffolds can be designed to provide biological growth factors for neuronal tissues and to accurately adjust the diffusion rate of these essential biomolecules and enzymes[187].
The application of combined DSCs with various scaffolds promotes the function of injured neural tissues and reduces the inflammatory responses.The most common scaffolds applied for neural tissue regeneration and repair include chitosan, heparinpoloxamer, silicone tubes, poly-ε-caprolactone/poly-lactide-co-glycolic acid, and electrospun neuro-supportive scaffolds[191].Different scaffolds were used to enhance neural differentiation and promote their neuronal characteristics.DSCs can be seeded in the biodegradable electrospun neuro-supportive scaffold, which is amended by different 3D coatings, for enhancedin vitroandin vivorecovery of neuronal damage[192].The granular 3D chitosan scaffolds provide an appropriate microenvironment for attachment, proliferation, and neural differentiation of DSCs[193].Furthermore, a 3D floating sphere culture system has been shown to provide a suitable micromilieu for human DSCs to retain their neuronal characteristics compared to myogenic and osteogenic properties[194].Using an acellular ECM scaffold has been shown to promote DSCs to obtain a neuronal-like organization, including a central body associated with long cytoplasmic extensions that follow the underlying fibers, with high cell-matrix adhesion properties[195].Some scaffolds can support the neurotrophic release of DSCs for the subsequent survival and differentiation of neural stem cells as well as neural cells.For instance, DSCs promoted the survival and differentiation of adult murine neural stem cells on ethyl acrylate and hydroxyethyl acrylate copolymer scaffold through the enhancement of neurotrophic factor secretion[196].
Transplantation of DSCs with a chitosan scaffold markedly enhanced the recovery of motor function and suppressed inflammatory responses, possiblyviathe secretion of neurotrophic factors, such as glial cell-derived neurotrophic factor and brainderived neurotrophic factor, in experimental models of spinal cord injury.Furthermore, the combination of DSCs with scaffolds inhibited cell injury and death through the reduction of caspase activity[197].A significant functional recovery of hindlimb locomotor activities has also been observed following the transplantation of DSCs seeded in chitosan scaffolds in a spinal cord injury animal model[198].Solubilized forms of acellular ECM from dentine, bone, and spinal cord have discrete structural,mechanical, and functional properties.Human DSCs exhibited a strong positive response to spinal cord ECM hydrogels by the greater expression of neural lineage markers.This ECM scaffold markedly enhanced the differentiation of DSCs to a neural lineage; indicating the importance of site-specific tissues in the promotion of stem cell behavior for constructive spinal cord regeneration[24].A combination of DSCs with heparin-poloxamer, a desirable thermosensitive hydrogel forin vivoapplications,loaded with various growth factors, such as bFGF and nerve growth factor (NGF),markedly promoted functional recovery, cellular regeneration, and tissue repair in a rat model of spinal cord injury[187], possiblyviamodulation of the MAPK/ERK,PI3K/Akt and JAK/STAT3 signaling pathways[199].Indeed, both bFGF and NGF play an essential role in the neural differentiation of DSCs[200].Chitosan scaffolds in combination with bFGF exerted a synergistic facilitating effect on DSCs differentiation to neural cells, possiblyviaactivation of the ERK signaling pathway[201].It has been shown that DSCs can proliferate efficiently on an aligned electrospun poly εcaprolactone/poly lactide-co-glycolic acid scaffold and restore defects in rat spinal cord.Furthermore, these cells contribute to remyelination by the expression of oligodendrogenic lineage markers[202].
Multiple studies have assessed the effects of DSCs with various scaffolds on various experimental models of peripheral nerve injury.DSCs seeded into a polylactic-glycolic acid scaffold significantly improved the regeneration of injured facial nerve and promoted functional recovery compared to autografts[203].Schwann-like cells derived from DSCs and grown in collagen scaffolds facilitated axonal outgrowth and myelination in both 2D and 3Din vitromodels of peripheral nerve injury[204,205].Furthermore, oligodendrocyte progenitor cells induced by differentiation of human DSCsviagene transfection in combination with collagen or collagen and fibrin scaffolds improved axonal outgrowth and myelination in an animal sciatic nerve injury model[9,206].Human DSCs isolated from the periodontal ligament and gingival tissues and encapsulated in 3D alginate/hyaluronic acid scaffolds in the presence of NGF improved the proliferation and differentiation of DSCs toward the formation of neural tissues[207].DSCs seeded on poly-lactic-co-glycolic acid collagen enhanced the interconnections of injured axons in a model of facial nerve injury[203].When cultured under either 2D- or 3D-collagen scaffolds, human DSCs originating from gingival tissue have shown a greater capability of differentiating into neurons and Schwannlike cells in a 3D collagen scaffold compared to the 2D culture system.Furthermore,these cells with a 3D scaffold improved regeneration and functional recovery of neural tissues in rat facial nerve defects[208].It has been shown that collagen scaffolds in the presence of different growth factors, such as bFGF, exhibited favorable mechanical properties and improved facial nerve regeneration[209].Human DSCs expressing STRO-1, c-Kit, and CD34 markers and seeded in a collagen scaffold engrafted into rat sciatic nerve defects improved axonal regeneration from proximal to distal stumps[210].Interestingly, the administration of serum-free conditioned medium from DSCs plunged in a collagen sponge into the gap caused by rat facial nerve transection,induced axonal regrowth and restored the neurological deficits[211].
THE IMPACT OF DIFFERENT SCAFFOLDS USED IN DSCS CELL THERAPY
Using an appropriate scaffold can promote the proliferation, differentiation, migration,and functional capacity of DSCs and can optimize and preserve the cellular morphology to build tissue constructs for a specific purpose[63].Although the application of DSCs alone could yield promising outcomes in cell replacement therapy in particular conditions[212], an appropriate scaffold provides a viable microenvironment to boost the development of DSCs towards new tissue formation,especially in tissues or organs with extensive defects[213].The optimal number of DSCs is essential to develop tissue and organ substitutes and to restore organ function[149].In addition to establishing definitive protocols for DSCs preparation, appropriate carrier scaffolds play a crucial role to increase the number of cells for implantation(Figure 3)[214].
A crucial and challenging demand for an appropriate scaffold design is recapitulating the dynamic nature of the native tissue[215].Although each polymer scaffold has its pros and cons and favorable tissue engineering applications, collagen and fibrin, alone or by forming hybrid scaffolds, provide an adequate pulp connective tissue formation associated with marked vascularization, particularly when loaded with active biomolecules[117,118,216].Collagen is the main component of the ECM and is expressed widely in bone, teeth, and the brain.A collagen scaffold provides excellent biocompatibility and controllable biodegradability, particularly for bone tissue engineering[217,218].However, collagen has poor mechanical, chemical, and thermal stability and degrades fast at an uncontrolled rate.Fibrin is a non-toxic biomaterial scaffold that can attach various biological surfaces to regenerate tissues, such as bone and nervous tissues, with a low inflammatory response[219].However, low mechanical stiffness of fibrin scaffolds limits tissue diffusion and direct implantation of cells to the damaged tissues[220,221].Different bioceramic scaffolds exhibit excellent biocompatibility and osteoconductivity due to their chemical and structural similarity to native bone,which is characterized by high mechanical stiffness and low elasticity[158,222].Furthermore, bioceramic scaffolds improve stem cell differentiation and osteogenesis[222].The main disadvantages of bioceramic scaffolds are brittleness and slow biodegradation in the crystalline phase[218].Soft polymers with highly aqueous hydrogels, such as collagen, share a resemblance to neural tissues, play an important role as a possible internal filler for neural conduits and increase the quality of peripheral nerve regeneration[223].
Furthermore, the scaffold should be porous and spongy to be able to deliver sufficient DSCs to injured tissues and to allow the stream of ECM and the formation of neovascularization[165,166].However, some of the currently available biomaterials do not fully imitate the essential functions of natural ECM and fail to provide an appropriate scaffold[224].Among the different biomaterials, the self-assembly of monodisperse cells into 2D or 3D complex structures that produce more extracellular matrix and promote intercellular communication possess the characteristics of the ideal approach[225].Although both 2D and 3D cell culture systems provide appropriate methods for stem cell replacement transplantation, 3D systems seem to be more effective at mimicking the ECM in native tissues[226,227].In general, 3D culture systems have been shown to be more beneficial in providing a template for the reconstruction of defects and cell-tocell interactions as well as for improving cell adhesion, proliferation, ECM generation,maintenance of cell polarity, and restoration of various tissues[228,229].In addition, 3D scaffolds enhance the sensitivity of stem cells towards drugs and biomolecules[230].The optimization of 3D scaffold pore sizes may lead to better tissue regeneration through the enhancement of mechanical strength[231].The dimension of the defect is a key factor in selecting a scaffold for tissue or organ regeneration[232].For instance, in the reconstruction of cleft lip and palate, the amount of bone formation may not be enough to fill the bone defect[233], a problem that may be solved by the application of 3D cell culture systems[234].In this regard, higher osteogenic differentiation of DSCs and MSCs has been observed in 3D than in 2D cell culture[174,235].
In addition to an appropriate scaffold, using bioactive molecules, such as growth and angiogenic factors, has been suggested as a promising strategy for the improvement of DSCs transplantation.Bioactive molecules, such as VEGF, have a short half-life and need to be encapsulated in degradable materials to regulate their release and promote their effects[236].Scaffolds provide a purposeful approach for better incorporation between stem cells and biomolecules to improve tissue regeneration[26].The interpolation of active biomolecules with the scaffold is essential for their transport into the injured tissues and for their efficacy to promote the colonization of DSCs and their matrix deposition[123].DSCs and various scaffolds transplanted together with bioactive molecules, such as G-CSF, BMP, and bFGF, can fill the entire pulp or bone defect as well as develop new dentin or bone formation[92,93,118].Biomolecules, such as SDF-1, SCF, and G-CSF, help to summon DSCs and enhance the number of cells in the implantation site, and other factors, such as VEGF, can enhance the formation of new blood vessels in regenerative tissues[26,237].
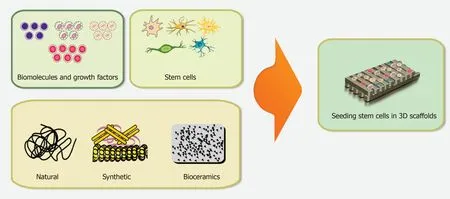
Figure 3 Schematic overview of the optimal biomimetic environment for application in tissue engineering.
On the contrary, a few investigations have suggested that transplantation of DSCs without scaffold may have more beneficial effects on tissue regeneration.To prevent the inflammatory response, immune rejection, or infections, a few studies have indicated that transplantation of stem cells without scaffolds (such as 3D stem cell spheroids) may be an alternative option for DSCs transplantation[238].Transplantation of DSCs without a scaffold for injured tooth tissues in 26 patients led to the regeneration of 3D pulp tissue which contained blood vessels and sensory nerves 12 months after therapy[239].Despite these studies, it seems that the simple injection of competent DSCs inside organ defects is poorly regenerative[123].
A few decades of intense basic studies and clinical trials on DSCs are essential to translate knowledge gained on these cells into the implementation of defined and reproducible therapeutic approaches to cure or alleviate diseases.In addition to the application of an ideal scaffold, the success of cell transplantation therapy using DSCs also relied greatly on designing methodologies for isolation and purification, a sufficient number of stem cells, and effective and safe differentiation into different lineages[240,241].The development of an accurate immunomodulatory strategy for injectable and implantable biomaterials is of particular importance to facilitate the grafting of DSCs at inflamed sites[242,243].
CONCLUSION
This study describes the main scaffolds, both natural and synthetic, used in DSCs transplantation and evaluated the advantages and disadvantages of various types of scaffolds.Most of the existing studies concerning the development of novel therapeutic approaches for restoration of damaged tissues have been limited toin vitroandin vivoDSCs testing, with a small number of clinical trials.Although the coapplication of biomolecules with an appropriate scaffold seems to be crucial for effective cell transplantation therapy with DSCs, there is still much to learn about the dynamics of these molecules as well as their interactions with the ECM and DSCs to allow planning of appropriate therapeutic approaches.Further advances in tissue engineering need to focus on innovative combinations of biopolymers and biomolecules to promote the capability of DSCs for novel and effective therapeutic approaches (Figure 3).
杂志排行
World Journal of Stem Cells的其它文章
- Human mesenchymal stem cells derived from umbilical cord and bone marrow exert immunomodulatory effects in different mechanisms
- Mass acquisition of human periodontal ligament stem cells
- Perspectives on mesenchymal stem/progenitor cells and their derivates as potential therapies for lung damage caused by COVID-19
- Stem cell treatments for oropharyngeal dysphagia:Rationale,benefits, and challenges
- Mechanisms of action of neuropeptide Y on stem cells and its potential applications in orthopaedic disorders
- Senescent mesenchymal stem/stromal cells and restoring their cellular functions
