Large leiomyoma of lower esophagus diagnosed by endoscopic ultrasonography-fine needle aspiration:A case report
2020-04-08
Min Rao,Qing-Qing Meng,Department of Hepatology and Gastroenterology,The Second Part of First Hospital of Jilin University,Changchun 130021,Jilin Province,China
Pu-Jun Gao,Department of Hepatology,The First Hospital of Jilin University,Changchun 130021,Jilin Province,China
Abstract BACKGROUND Benign esophageal tumors are rare accounting for < 1% of esophageal tumors;two-thirds of which are leiomyomas. Esophageal leiomyoma is a benign tumor derived from mesenchymal tissue that is completely muscularly differentiated.Most esophageal leiomyomas are < 5 cm. Esophageal leiomyomas > 5 cm are rare.We describe a case of a large esophageal leiomyoma involving the cardia and diaphragm.CASE SUMMARY A 35-year-old woman presented to the doctor because of a choking sensation after eating. Physical examination showed no positive signs. Gastroscopy indicated an uplifted change in the cardia. Enhanced computed tomography revealed spaceoccupying lesions in the lower part of the esophagus and cardia,which were likely to be malignant. Positron emission tomography-computed tomography showed increased metabolism of soft tissue masses in the lower esophagus and near the cardia. Malignant lesions were considered,and mesenchymal tumors were not excluded. Endoscopic ultrasonography was performed to examine a hypoechoic mass in the lower esophagus,which was unclear from the esophageal wall. Clinical evaluation suggested diagnosis of esophageal and cardiac stromal tumors. Finally,histological specimens obtained by endoscopic ultrasonographyfine needle aspiration suggested leiomyoma. The patient underwent laparoscopic local resection of the tumor. The postoperative pathological diagnosis was leiomyoma.CONCLUSION Endoscopic ultrasonography-fine needle aspiration is necessary for the diagnosis of gastrointestinal leiomyomas. It provides a strong basis for diagnosis of gastrointestinal tumors of unknown nature and origin.
Key Words:Esophageal tumor; Leiomyoma; Endoscopic ultrasonography; Fine needle aspiration; Endoscopic ultrasonography-fine needle aspiration; Case report
lNTRODUCTlON
Benign esophageal tumors are rare accounting for < 1% of esophageal tumors; twothirds of which are leiomyomas[1-3]. Leiomyomas are the most common benign esophageal tumors. Leiomyoma is common in middle-aged patients with a male to female ratio of 2:1. Leiomyomas < 5 cm are mostly asymptomatic and discovered accidentally. The larger the leiomyoma,the more likely it is to show symptoms,such as dysphagia and chest pain. Most leiomyomas do not need treatment,but regular follow-up observation; if large leiomyomas cause symptoms,resection is required.
The pathology of leiomyoma is characterized by intersecting spindle cells with rich cytoplasm,and the malignant potential is low. In immunohistochemical examination,the specific signs of leiomyoma are diffuse positivity for desmin and smooth muscle actin (SMA) and negativity for CD34 and CD117. Abdominal computed tomography(CT) and endoscopic ultrasound (EUS) can diagnose most upper gastrointestinal leiomyomas,but there are still some difficulties in the diagnosis of atypical lesions,which can easily be misdiagnosed as stromal tumors and other malignant lesions.Tumor histological specimens can be obtained through EUS-fine needle aspiration(FNA),which provide a strong basis for the diagnosis of gastrointestinal tumors of unknown nature and origin.
Here we report a case of large esophageal leiomyoma. The CT and endoscopic findings of this case were close to those of stromal tumors. However,through EUS-FNA examination,the final diagnosis was leiomyoma.
CASE PRESENTATlON
Chief complaints
A 35-year-old woman with hiccups and belching for > 30 years presented at the hospital because of choking and foreign body sensation during eating over the past 10 d. Abdominal CT and gastroscopy had not previously been performed.
History of present illness
The patient has experienced choking and foreign body sensation during eating over the past 10 d.
History of past illness
Patient has no relevant past medical history.
Personal and family history
Patient has no relevant family history.
Physical examination
There were no positive signs.
Laboratory examinations
No abnormalities were found by blood biochemical examination.
Imaging examinations
Gastroscopy showed uplifted changes in the cardia. Contrast-enhanced CT of the stomach (Figure 1) indicated space-occupying lesions in the lower esophagus and cardia,which were likely to be malignant. Positron emission tomography-CT(Figure 2) showed increased metabolism of soft tissue masses in the lower esophagus and near the cardia. Malignant lesions were considered,and mesenchymal malignant tumors were not excluded. EUS (Figure 3) examined the lower part of the esophagus near the cardia,and a hypoechoic mass was seen close to the esophageal wall growing outward. The internal echo was uneven,and there was no echo in some parts. Blood flow signals were seen inside. The mass was close to the liver and diaphragm,and the longest diameter of the section was approximately 4.9 cm. EUS diagnosed a hypoechoic mass in the lower esophagus with an unclear boundary with the esophageal wall. Combined with the above examinations,preoperative assessment was a probable stromal tumor. The tumor was large and involved the diaphragm and liver,thus making surgery difficult. Preoperative FNA examination was recommended to determine the treatment plan.
FlNAL DlAGNOSlS
Postoperative pathological diagnosis was leiomyoma.
TREATMENT
The patient agreed to undergo EUS-FNA examination. Under EUS,a puncture needle was placed in the lower part of the esophagus near the cardia and pierced the center of the tumor. A strip of tissue was obtained and sent for pathological examination(Figure 4A). Pathological examination showed a large amount of mucus-like tissue that included a small amount of smooth muscle tissue (Figure 4B). Immunohistochemistry showed:SMA (+),desmin (+),H-caldesmon (+),CD117 (-),Dog-1 (-),S-100 (-),CD34 (-),CKpan (-),SDHB (+) and Ki-67 (+ < 1%) (Figure 4C). Histological and immunohistochemical results suggested that the tumor was leiomyoma. Laparoscopic local resection of the mass was performed (Figure 5A). The postoperative pathological diagnosis was leiomyoma (tumor volume 8.0 cm × 6.0 cm × 3.5 cm) (Figure 5B).Immunohistochemistry showed:CD34 (-),desmin (+),H-caldesmon (+),Ki-67 (+1%),SDHB (+),SMA (+),CD117 (-),Dog-1 (-) and S-100 (-) (Figure 5C). These findings were consistent with the results of EUS-FNA before surgery.
OUTCOME AND FOLLOW-UP
The patient recovered well after the operation,and there is no information for review at present.
DlSCUSSlON
Benign esophageal tumors are rare accounting for < 1% of esophageal tumors; twothirds of which are leiomyomas[1-3]. The rest are mostly cysts (20%),polyps (5%),gastrointestinal stromal tumors (< 5%) and lipomas (< 1%)[4,5]. Leiomyoma is the most common benign tumor of the esophagus. Esophageal leiomyomas are common in middle-aged patients,and the male to female ratio is 2:1[2,6]. Leiomyomas < 5 cm are mostly asymptomatic and discovered accidentally. The larger the leiomyoma,the more likely it is to show symptoms,such as dysphagia and chest pain[7-10]. The pathology of leiomyoma is characterized by intersecting spindle cells with rich cytoplasm,and the malignant potential is low. In immunohistochemical examination,the specific signs of leiomyoma are diffuse positivity for desmin and SMA and negativity for CD34 and CD117[11,12].
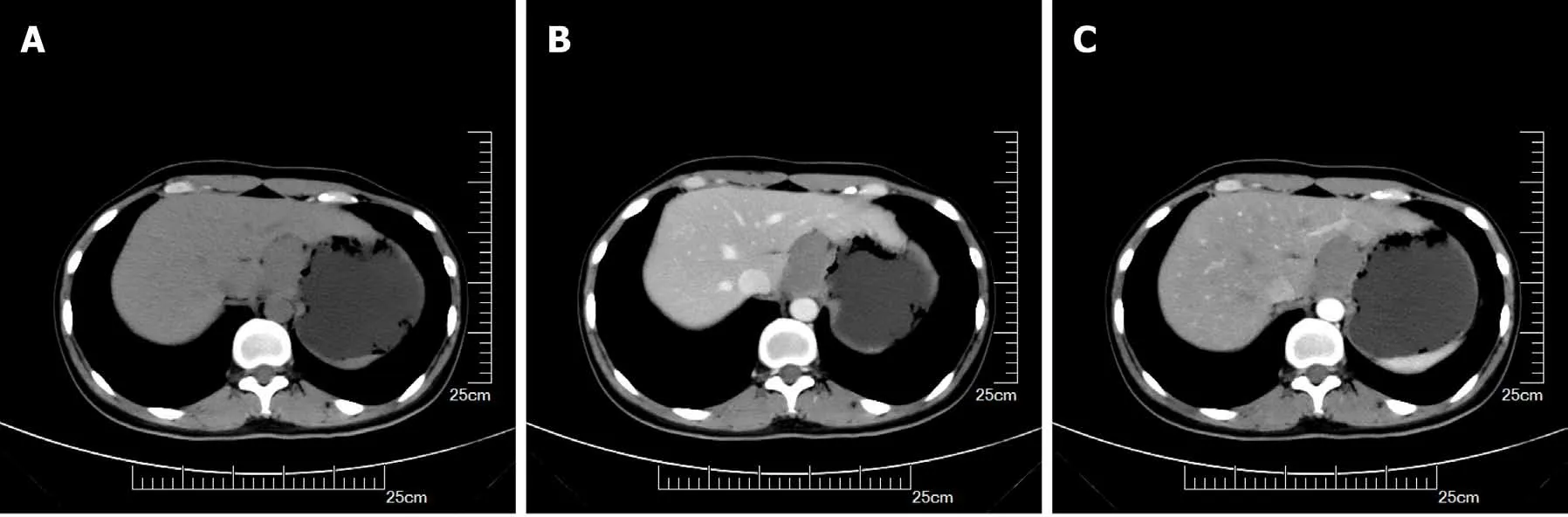
Figure 1 Stomach computed tomography images. A:Plain scan; B:Arterial phase; C:Venous phase.
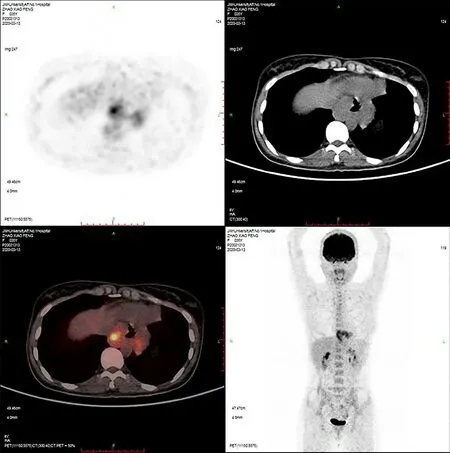
Figure 2 Positron emission tomography-computed tomography image.
For most esophageal leiomyomas,the most common imaging test is upper gastrointestinal barium meal or esophagography because it is the least invasive,simplest and most common examination method[13-15]. As a noninvasive investigation method,CT examination has high diagnostic accuracy for space-occupying lesions of the digestive system and can make an accurate assessment of the exact location,size,range and distribution of blood vessels of the lesion. The CT findings of leiomyomas are soft tissue masses with clear boundaries. The tumors are of various shapes. The common growth patterns are intracavitary and transmural inside and outside the cavity. The mass density is uniform on CT scan,and enhanced scanning shows mild to moderate uniform enhancement. Compared with stromal tumors,leiomyomas have fewer ulcers[12].
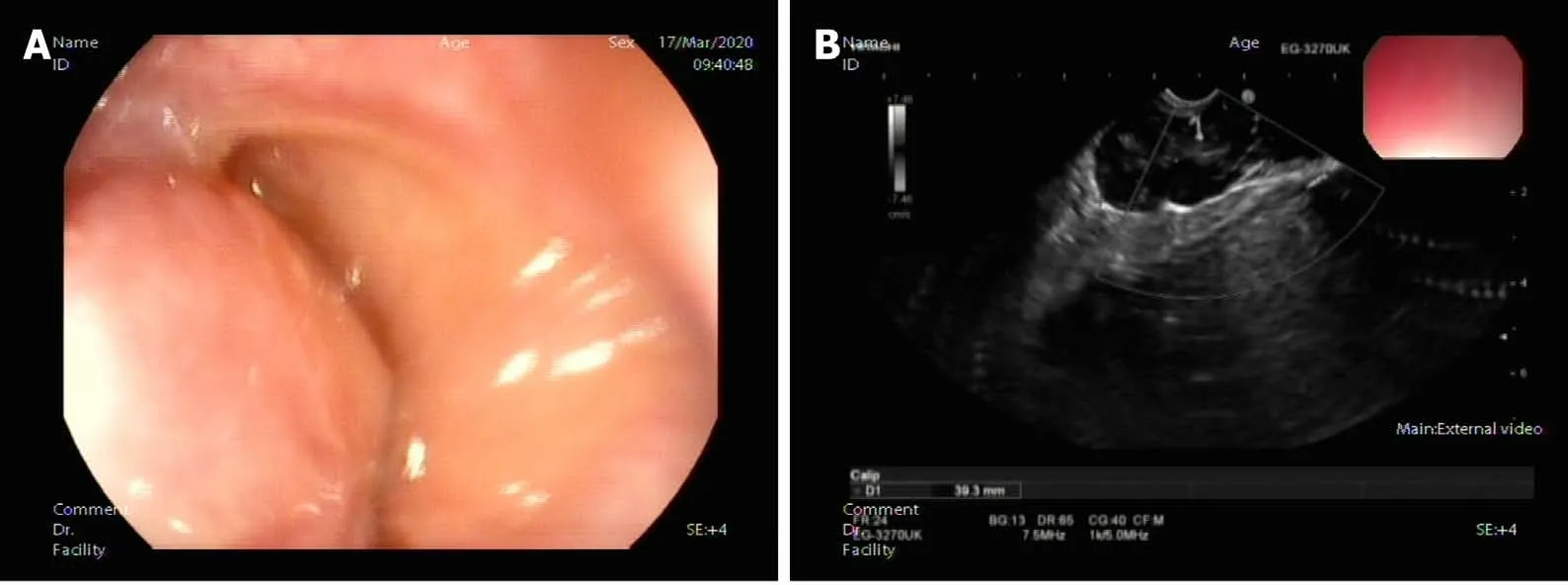
Figure 3 Endoscopic ultrasound examined the lower part of the esophagus near the cardia,and a hypoechoic mass was seen close to the esophageal wall growing outward. A:Large uplift of the cardia under endoscopy; B:Endoscopic ultrasonography image.
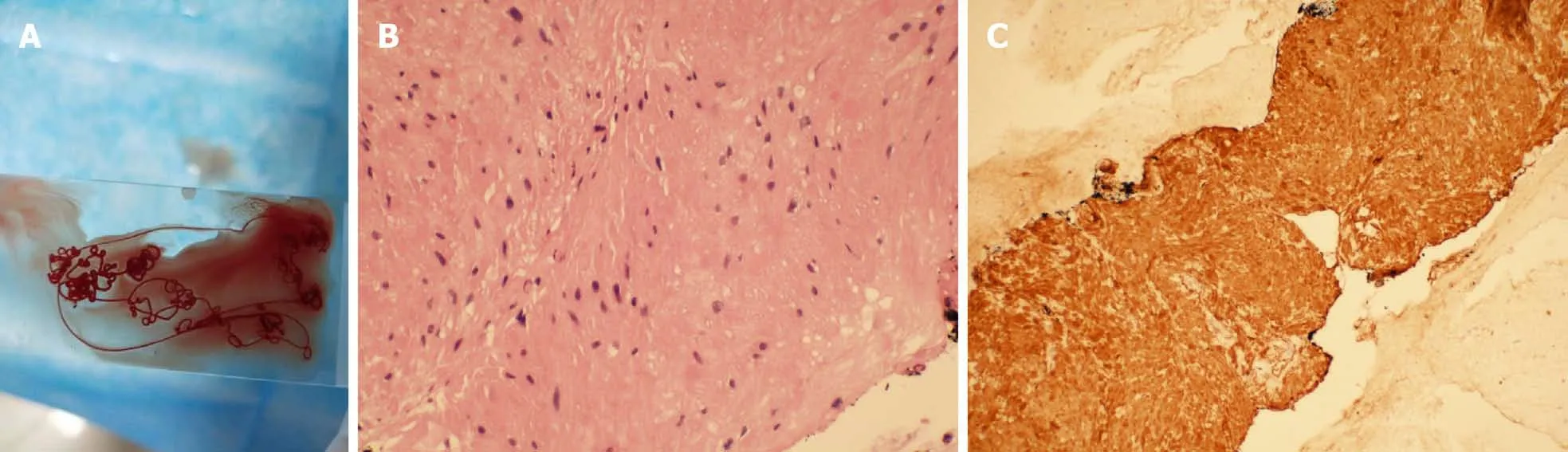
Figure 4 Pathological examination. A:Tissue specimen aspirated by endoscopic ultrasonography-fine needle aspiration (FNA); B:Cytological examination of FNA biopsy of tumor (hematoxylin and eosin staining,400 ×); C:Immunohistochemical staining of FNA biopsy of tumor.
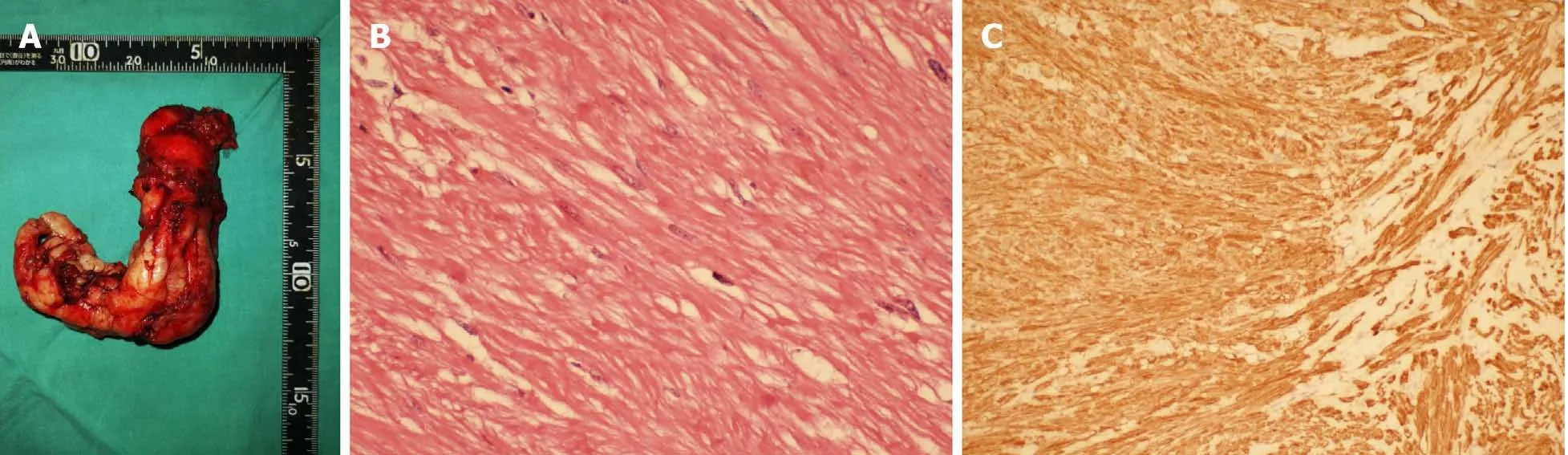
Figure 5 Laparoscopic local resection of the mass was performed and pathological examination. A:Postoperative whole tumor tissue specimen;B:Cytological examination of the whole tumor (hematoxylin and eosin staining,400 ×); C:Immunohistochemical staining of the tumor.
EUS is currently an important diagnostic method for esophageal leiomyoma. Under EUS,leiomyomas mostly originate in the muscularis mucosa with smooth surface mucosa and mostly show uniform hypoechoic lesions. EUS is more accurate for diagnosis of lesions derived from the muscularis mucosa and muscularis propria.Previous studies have suggested that EUS makes a diagnosis based on factors such as the location,level of origin,size,echo intensity,uniformity,boundary and relationship with surrounding organs of the submucosal mass,and its specificity is 80%-88%[16,17].Esophageal lesions from the muscularis mucosa or the muscularis propria are mainly leiomyomas,and only a few lesions derived from the muscularis propria are stromal tumors. The proportion of esophageal stromal tumors is < 7%[18]. Although EUS provides important information for identifying submucosal masses in the upper gastrointestinal tract,it still has some limitations. The main problem is that judgment of the origin level of the tumor does not match the actual situation. This may be related to incorrect operation and subjective misjudgment of the operator.
For atypical upper gastrointestinal tumors,pathological diagnosis is still the gold standard when CT and EUS imaging findings are uncertain. EUS-FNA examination not only finds submucosal lesions and accurately determines their origin,size and echogenicity,but also directly punctures larger lesions to obtain materials for histological and cytological examination and immunohistochemical staining. It is reported in the literature that the diagnostic accuracy of EUS-FNA for upper gastrointestinal submucosal masses is 95.6%,and its accuracy,sensitivity and specificity in distinguishing benign from potentially malignant lesions are 94.2%,92.4% and 100.0%,respectively. Combined with immunohistochemical staining,the diagnostic accuracy rate can reach 98%[19-21]. This shows that EUS-FNA is an effective means to accurately diagnose this type of tumor.
For most upper gastrointestinal leiomyomas,diagnosis is not difficult by barium meal imaging,CT,EUS and other methods. However,the leiomyoma in the present case had the following characteristics. The tumor was large,wide,started from the lower esophagus,involved the cardia and reached the abdominal cavity next to the diaphragm and liver. The boundary with the diaphragm was unclear and the tumor grew outward. Enhanced scanning showed different degrees of enhancement; the echo was not uniform with an abundant blood flow signal within the tumor. These clinical features are more likely to be the characteristics of stromal tumors and other malignant lesions and are less common in leiomyomas. If EUS-FNA is not performed,histological specimens cannot be obtained,which may cause misdiagnosis and miss the opportunity for surgical treatment. Through this case,we have gained more understanding of large leiomyoma of the upper digestive tract and have provided more clinical indicators for diagnosis and treatment of the disease.
CONCLUSlON
Abdominal computed tomography and EUS have high diagnostic accuracy for most upper gastrointestinal leiomyomas,but there are still difficulties in the diagnosis of atypical lesions,which can be misdiagnosed as stromal tumors and other malignant lesions. For the diagnosis of such lesions,EUS-FNA is necessary. EUS-FNA examination provides a strong basis for the diagnosis of gastrointestinal tumors of unknown nature and origin. The results are consistent with surgical pathological examination and provide good clinical indicators for final diagnosis and treatment.
杂志排行
World Journal of Clinical Cases的其它文章
- COVID-19:A review of what radiologists need to know
- Holistic care model of time-sharing management for severe and critical COVID-19 patients
- Bioequivalence of two esomeprazole magnesium enteric-coated formulations in healthy Chinese subjects
- Osteoprotegerin,interleukin and hepatocyte growth factor for prediction of diabetes and hypertension in the third trimester of pregnancy
- High serum lactate dehydrogenase and dyspnea:Positive predictors of adverse outcome in critical COVID-19 patients in Yichang
- Risk factors analysis of prognosis of adult acute severe myocarditis
