High serum lactate dehydrogenase and dyspnea:Positive predictors of adverse outcome in critical COVID-19 patients in Yichang
2020-04-08
Xiao-Ting Lv,Yong-Xu Jin,Hai-Bo Ding,Cai-Yun Wang,Gong-Ping Chen,Department of Respiratory and Critical Care Medicine,the First Affiliated Hospital of Fujian Medical University,Fuzhou 350005,Fujian Province,China
Xiao-Ting Lv,Institute of Respiratory Disease,Fujian Medical University,Fuzhou 350005,Fujian Province,China
Yong-Ping Zhu, Department of Cardiovascular Surgery,Fujian Medical University Attached Union Hospital,Fuzhou 350001,Fujian Province,China
Ai-Guo Cheng,Department of Critical Medicine,the Third People's Hospital of Yichang,Yichang 443000,Hubei Province,China
Shu-Yu Zhang,Qing-Quan Chen,Department of Laboratory Medicine,Fujian Medical University,Fuzhou 350004,Fujian Province,China
Qi-Cai Liu,Department of Reproductive Medicine Centre,First Affiliated Hospital of Fujian Medical University,Fuzhou 350005,Fujian Province,China
Abstract BACKGROUND Coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) outbreak in China,constitutes a Public Health Emergency of International Concern. It is well known that COVID-19 patients may have increased serum lactate dehydrogenase (LDH) levels in the early stage. The clinical changes in LDH may have predictive value in disease evolution and prognosis in critically ill COVID-19 patients.AIM To examine serum LDH and clinical characteristics in patients with COVID-19 and their predictive value for prognosis. METHODS This retrospective study analyzed the clinical data of forty-seven critical COVID-19 patients in the intensive care unit of the Third People's Hospital of Yichang City from January 27 to March 25,2020 and divided them into survivors and nonsurvivors. The patients were diagnosed according to the World Health Organization interim guidance and critical cases met any one of the following criteria:Respiratory failure and required mechanical ventilation,the occurrence of shock,and the combined failure of other organs that required intensive care unit monitoring and treatments,according to the diagnostic criteria of critical COVID-19. Clinical data including symptoms,detection of SARS-CoV-2,chest computed tomography (CT) images,changes in serum LDH in different clinical phases,and prognosis were collected. Statistical analysis of the data was performed.Continuous variables were expressed as median (interquartile range) and compared with the Mann-Whitney U test. Categorical variables were compared with the Chi-square test. Survival data were analyzed using Kaplan-Meier survival curves and log-rank tests.RESULTS According to chest CT images,we observed the alveolitis and fibrosis stages in all critical patients in this study. Most non-survivors died in the fibrosis stage. Nonsurvivors had fewer days of hospitalization,shorter disease duration,shorter duration of alveolitis and fibrosis,and had dyspnea symptoms at disease onset (P= 0.05). Both first and lowest LDH values in the alveolitis stage were more pronounced in non-survivors than in survivors (449.0 U/L vs 288.0 U/L,P =0.0243; 445.0 U/L vs 288.0 U/L,P = 0.0199,respectively),while the first,lowest and highest values of serum LDH in non-survivors were all significantly increased compared to survivors in the fibrosis phase (449.0 U/L vs 225.5 U/L,P= 0.0028; 432.0 U/L vs 191.0 U/L,P = 0.0007; 1303.0 U/L vs 263.5 U/L,P = 0.0001,respectively). The cut-off points of first LDH values in the alveolitis and fibrosis phase for distinction of non-survivors from survivors were 397.0 U/L and 263.0 U/L,respectively. In the fibrosis stage,non-survivors had more days with high LDH than survivors (7.0 d vs 0.0 d,P = 0.0002). Importantly,patients with high LDH had a significantly shorter median survival time than patients with low LDH in the alveolitis phase (22.0 d vs 36.5 d,P = 0.0002),while patients with high LDH also had a significantly shorter median survival time than patients with low LDH in the fibrosis phase (27.5 d vs 40.0 d,P = 0.0008). The proportion of non-survivors with detectable SARS-CoV-2 until death in the alveolitis stage was significantly increased compared with that in the fibrosis stage (100% vs 35.7%,P = 0.0220).CONCLUSION High LDH and dyspnea symptoms were positive predictors of an adverse outcome in critical COVID-19. The rapid progressive fibrosis stage was more perilous than the alveolitis stage,even if SARS-CoV-2 is undetectable.
Key Words: COVID-19; SARS-CoV-2; Lactate dehydrogenase; Pulmonary fibrosis;Dyspnea; Overall survival
INTRODUCTION
The large-scale new coronavirus disease pneumonia (coronavirus disease 2019,COVID-19) broke out in Wuhan City,China and the basic reproductive number was 2.68 (95%CI:2.47-2.86)[1,2]. Millions of cases have been reported worldwide,and the fatality rate was up to 7%[3]. The pathogen,officially named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),was confirmed to be related to Middle East respiratory syndrome and severe acute respiratory syndrome (SARS)[3-6]. However,the prognosis of critically ill and severe patients is extremely poor. It is well known that some patients have increased lactate dehydrogenase (LDH) levels in the early stage of COVID-19[7]and predictors of poor outcome in SARS were increased age,comorbidities and high LDH in 2003[8]. Whether serum LDH can be used as a marker related to COVID-19 treatment response as well as SARS is inconclusive.
Computed tomography (CT) images and pathological findings of critical COVID-19 patients have characteristic manifestations in the alveolitis and fibrosis stages. Chest CT images are characterized by multiple ground-glass opacities (GGO) and early infiltration in the acute alveolitis stage. Furthermore,critical cases often subsequently progressed to the fibrosis stage and showed consolidation,reticular pattern,and other fibrosis patterns on chest CT[7,9-11]. In addition,autopsy results in critical COVID-19 patients who died within 14 d demonstrated typical pathological changes of acute respiratory distress syndrome such as desquamation of pneumocytes,hyaline membrane formation,interstitial monocytes and lymphocytes inflammatory infiltrates[12],while pathological findings of patients who died within 17-19 d showed lighter exudation of alveolar fluid and cellulose,less hyaline membrane,obvious changes in the proliferation of type II alveolar epithelial cells and alveolar fleshy change and interstitial fibrosis[13]. The pathological findings were in accordance with CT images in the different stages of COVID-19. Early recognition and isolation of critical COVID-19 patients in the alveolitis and fibrosis stages are crucial in controlling this outbreak.
The aim of this study was to describe the clinical characteristics,and to examine the clinical changes in LDH in the alveolitis and fibrosis stages according to the CT findings in critically ill COVID-19 patients in the intensive care unit (ICU) and their predictive value for clinical prognosis.
MATERIALS AND METHODS
Study design and participants
A total of 47 patients in the ICU of the Third People's Hospital of Yichang City (one of the highly impacted epidemic areas in China) from January 27 to March 25,2020 were enrolled in this study. The Third People's Hospital of Yichang is a teaching hospital affiliated to Sanxia University and is also an infectious disease specialist hospital responsible for the treatment of COVID-19 patients as assigned by the government.The patients were diagnosed according to the World Health Organization interim guidance[14]and critical cases met any one of the following criteria:respiratory failure and required mechanical ventilation,the occurrence of shock,and the combined failure of other organs that required ICU monitoring and treatments,according to the diagnostic criteria of critical COVID-19[7]. The protocols for the study and informed consents were approved by the ethics committee of First Affiliated Hospital of Fujian Medical University [Approval No. (2020) 153]. All survivors were discharged following two negative nucleic acid tests of throat swab samples[7].
Data collection
General information included the gender,age,days of hospitalization,disease duration,duration of viral shedding,days from illness onset to hospital admission,duration of alveolitis and fibrosis phases,the complications of chronic obstructive pulmonary disease,hypertension,coronary heart disease,cerebrovascular disease,diabetes,renal dysfunction,malignant tumors and other underlying diseases,the numbers of complications,the initial symptoms such as fever,cough,dyspnea,fatigue and so on were obtained. Chest CT images were used to make a distinction between the alveolitis and fibrosis phases.
Laboratory analyses
The serum concentrations of LDH were detected using an appropriate detection Kit(No. A0701) ordered from Sichuan Chengdu New Health City Biological Co.,Ltd.(China),according to the manufacturer’s instructions. The recommended reference range for the normal population is (109-245) U/L. Throat swab samples were collected from the patients and fluorescent polymerase chain reaction was used to detect the ribonucleic acid (RNA) of SARS-CoV-2 using the new coronavirus 2019-nCov nucleic acid detection kit (No. DA0930-DA0932) provided by Sun Yat-sen University Daan Gene Co.,Ltd. (China). Patients with positive detection of SARS-CoV-2 RNA were identified as confirmed cases.
Statistical analysis
Statistical analysis was performed using the Statistic Package for Social Science 18.0 software package (Statistic Package for Social Science Inc.,Chicago,IL,United States).Continuous variables were expressed as median (interquartile range) and compared using the Mann-Whitney U test. Categorical variables were compared using the Chisquare test. Survival data were analyzed using Kaplan-Meier survival curves and the log-rank test. For all tests,P< 0.05 was considered statistically significant.
RESULTS
Clinical characteristics of patients with critical COVID-19
Forty-seven COVID-19 patients were divided into non-survivors (n= 17) and survivors (n= 30). The baseline characteristics of the patients with critical COVID-19 are summarized in Table 1. Non-survivors had fewer days of hospitalization,shorter disease duration and more dyspnea symptoms than survivors (P= 0.01). There was no significant difference between the two groups in terms of age (P= 0.595),gender (P=0.330),days from illness onset to hospital admission (P= 0.689),duration of viral shedding (P= 0.118),complications as well as the number of complications (P= 0.139).
According to chest CT images,we observed the alveolitis and fibrosis stages in all critical patients included in the study. Chest CT images of the alveolitis stage showed that patients with critical COVID-19 had bilateral lung involvement,mainly with peripheral and diffuse distribution and focal GGO. Following progression to the fibrosis stage,chest CT showed consolidation and pulmonary interstitial fibrosis changes such as the air bronchogram sign,bronchiectasis and reticular pattern. Some non-survivors showed more consolidation lesions than the survivors (Figure 1).According to the imaging findings,we found that the duration of inflammation and fibrosis was shorter in non-survivors than in survivors (P= 0.020 and 0.016).
High serum LDH levels were positively related to poor prognosis of patients with critical COVID-19
The results (Figure 2) showed that both first and lowest LDH values in the alveolitis stage were more pronounced in non-survivors than in survivors (449.0 U/Lvs288.0 U/L,P= 0.0243; 445.0 U/Lvs288.0 U/L,P= 0.0199,respectively). No difference at the highest value of serum LDH between non-survivors and survivors in this stage was found (499.0 U/Lvs349.0 U/L,P= 0.1360). The cutoff point of the first serum LDH concentration in the alveolitis stage for differentiating non-survivors from survivors was 397.0 U/L,according to receiver operating characteristic curve analysis. The ratio of days with high LDH (more than 397.0 U/L) to disease duration in non-survivors was markedly higher compared to survivors (0.14vs0.00,P= 0.0284),although the days with high LDH was not statistically significant between the two groups in the alveolitis stage.
In the fibrosis phase,the first,lowest and highest values of serum LDH in nonsurvivors were all significantly increased compared to survivors (449.0 U/Lvs225.5 U/L,P= 0.0028; 432.0 U/Lvs191.0 U/L,P= 0.0007; 1303.0 U/Lvs263.5 U/L,P=0.0001,respectively). The cutoff value of serum LDH for differentiating non-survivors from survivors was 263.0 U/L. Non-survivors had more days with LDH above 263.0U/L than survivors (7.0vs0.0 d,P= 0.0002) in the fibrosis phase. Moreover,the ratio of days with high LDH to disease duration in non-survivors was higher than that in survivors (0.31vs0.00,P= 0.0001). Our results revealed that serum LDH was increased in non-survivors,and the elevated levels of serum LDH were positively related to adverse outcome in the acute alveolitis and fibrosis phases.
High serum LDH was correlated with worsening overall survival in patients with critical COVID-19
Kaplan-Meier analysis and the log-rank test showed that patients with high LDH (≥397.0 U/L) had a significantly shorter median survival time compared to those with low LDH (< 397.0 U/L) in the alveolitis phase (22.0 dvs36.5 d,P= 0.0002) (Figure 3A).In addition,patients with high LDH (≥ 263.0 U/L) also had a significantly shorter median survival time compared to those with low LDH (< 263.0 U/L) in the fibrosis phase (27.5 dvs40.0 d,P= 0.0008) (Figure 3B).
Proportion of non-survivors with detectable SARS-CoV-2 until death in the alveolitis and fibrosis stages
All non-survivors who died in the alveolitis stage had detectable SARS-CoV-2 until death,but only some patients (35.7%) who died in the fibrosis stage had detectable SARS-CoV-2. The proportion of non-survivors with detectable SARS-CoV-2 until death in the alveolitis stage was significantly increased compared to that in the fibrosis stage (P= 0.0220) (Figure 4).
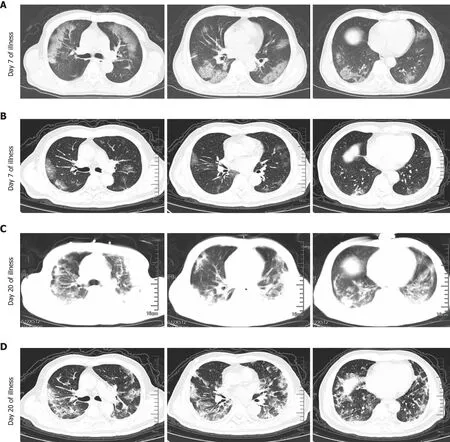
Figure 1 Chest computed tomography of critical coronavirus disease 2019 patients with different severity. A:Chest computed tomography(CT) of a 71-year-old man (non-survivor,case 1) showed multifocal and bilateral ground-glass opacities (GGO) in the alveolitis stage (Day 7 of illness); B:Chest CT of a 73-year-old male patient (survivor,case 2) exhibited slight GGO in the alveolitis stage (Day 7 of illness); C:Classified into the fibrosis stage (Day 20 of illness)and Chest CT (case 1) showed bilateral massive shadows of high density and GGO,accompanied by the air bronchogram sign and reticular pattern in the fibrosis stage; and D:Chest CT (case 2) showed that bilateral and multifocal lesions were observed with a combination of mixed GGO,reticular pattern,bronchiectasis and few consolidation (Day 20 of illness).
DISCUSSION
Our results showed that fewer days of hospitalization,shorter course of disease,shorter duration of alveolitis and fibrosis,and more dyspnea symptoms at disease onset were positively associated with adverse outcome in critical COVID-19. In addition,the first and lowest values of LDH in the alveolitis and fibrosis phase,the highest LDH value in the fibrosis phase of non-survivors were higher than those in survivors,together with more days with high LDH (≥ 263.0 U/L) in the fibrosis phase and the higher ratio of days with high LDH levels (≥ 397.0 U/L) in the alveolitis phase and ≥ 263.0 U/L in the fibrosis phase,respectively,to disease duration. The elevated levels of first LDH in the acute alveolitis and fibrosis phases were correlated with worsening overall survival. The rapid progressive fibrosis stage may be more perilous than the alveolitis stage,even if SARS-CoV-2 is undetectable.
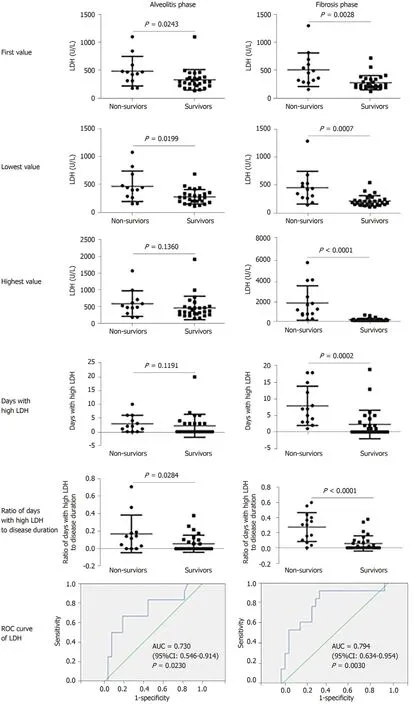
Figure 2 The relationship between serum lactate dehydrogenase levels and the prognosis of patients with critical coronavirus disease 2019. The first,lowest and highest values of serum lactate dehydrogenase (LDH),together with the days with high LDH (≥ 397.0 U/L in the alveolitis phase and ≥263.0 U/L in the fibrosis phase according to the receiver operating characteristic curve analysis,respectively) and the ratio of the days with high LDH to disease duration were analyzed by the Mann-Whitney U test between non-survivors and survivors in the alveolitis phase and fibrosis phase. P < 0.05 was considered statistically significant. LDH:Lactate dehydrogenase.
It was reported that older age was correlated with unfavorable outcomes in COVID-19,SARS and Middle East respiratory syndrome[15-18]. A previous study confirmed that SARS-CoV-infected aged macaques developed an exacerbated innate host response with an increased expression of genes associated with inflammation[18]. The current study showed that there was no significant difference between non-survivors and survivors in terms of the age of patients in Yichang,and the median age of survivors with critical COVID-19 was greater than COVID-19 survivors in Wuhan (67.0 yearsvs52.0 years)[15]. These results supported that older age may be a predictor of death in patients with critical COVID-19. In addition,there was no significant difference between the two groups in terms of gender as well as the median number of days from illness onset to hospital admission,similar to COVID-19 patients in Wuhan[15].
The median number of days from illness onset to hospital admission (5.0 d) was similar in survivors and non-survivors,and this value in Wuhan patients was 11.0 d.The concerns related to COVID-19 in Wuhan city helped patients receive earlier recognition and treatment in Yichang. Our results indicated that shorter disease course,shorter duration of alveolitis and fibrosis were associated with death in Yichang,which suggested non-survivors had more rapid progression,irrespective of disease stage.
Based on chest CT appearance,critical patients had diffuse GGO in the alveolitis phase,and massive consolidation lesions in the fibrosis phase. Fewer GGO and consolidation lesions were found in survivors than in non-survivors. Most nonsurvivors in our study died in the fibrosis phase (14/17),and few died in the alveolitis phase (3/17). It was reported that the virus was continuously detectable until death in all non-survivors[15]. Our study demonstrated that the alveolitis phase was significantly associated with detectable SARS-CoV-2 in non-survivors and only 35.7% of nonsurvivors had detectable SARS-CoV-2 until death in the fibrosis phase. The replicated SARS-CoV injured alveolar epithelial cells,leading to alveolitis and fibrotic lesions[19].Combined with shorter duration of the fibrosis stage in non-survivors,the rapid progressive fibrosis stage may be more perilous than the alveolitis stage,even if SARSCoV-2 is undetectable. Accumulating evidence suggests that a subgroup of patients with severe COVID-19 might have cytokine storm syndrome[20],and it was difficult for those who died in the alveolitis stage to eradicate the virus,and duration of viral shedding in these patients may be longer.
In addition,dyspnea symptoms at disease onset were associated with fatal outcome in the COVID-19 patients in our study. Dyspnea was also an independent clinical factor for H1N1 pneumonia[21]. There are many possible causes for dyspnea. On the one hand,pathological findings in COVID-19 patients showed pulmonary edema and hyaline membrane formation[12]. Aquaporin 5 (AQP5) and AQP1,located in the endothelial cells and secretory cells of terminal bronchioles and the alveolar type I cells,play an important role in water clearance in lungs. It was reported that porcine reproductive and respiratory syndrome virus infection usually caused pulmonary inflammation and edema in the infected lungs[13]. The expression of AQPs and Na,Kadenosine triphosphatase may be downregulated,causing lung edema with apoptosis of alveolar epithelial cells in porcine reproductive and respiratory syndrome virus infection. The replicated SARS-CoV may cause alveolitis and fibrotic changes,leading to acute lung injury that may develop into life-threatening acute respiratory distress syndrome[18,19]. On the other hand,a substantial portion of SARS patients had evidence of respiratory muscle weakness leading to air trapping,whereas inspiratory muscle weakness may lead to atelectasis,as at least 40% of patients suffered from acute respiratory failure requiring supplemental oxygen[22]. Respiratory muscle weakness may be one cause of dyspnea.
LDH has been reported to be a useful inflammatory biomarker of community acquired pneumonia,Mycoplasma pneumoniaepneumonia,and complicated pneumonia[23-25]. Our findings indicated that COVID-19 was associated with high levels of LDH,and elevated serum LDH could be used as a severity and poor prognosis indicator in patients with critical COVID-19 at different stages. Moreover,the best threshold of LDH level for predicting COVID-19 in the alveolitis and fibrosis phase was 397.0 U/L and 263.0 U/L,respectively. Among non-survivors,the first and lowest values of LDH in the alveolitis and fibrosis phase,and the highest LDH value in the fibrosis phase were higher than those in survivors,together with more days with high LDH (≥ 263.0 U/L) in the fibrosis phase and a higher ratio of days with high LDH levels (≥ 397.0 U/L in the alveolitis phase and ≥ 263.0 U/L in the fibrosis phase,respectively) to disease duration. Laboratory results showed that increases in LDH(28.3%) were more common in patients with COVID-19[3]. The level of LDH in severe patients was significantly higher than those in mild patients in Wuhan[15,26].
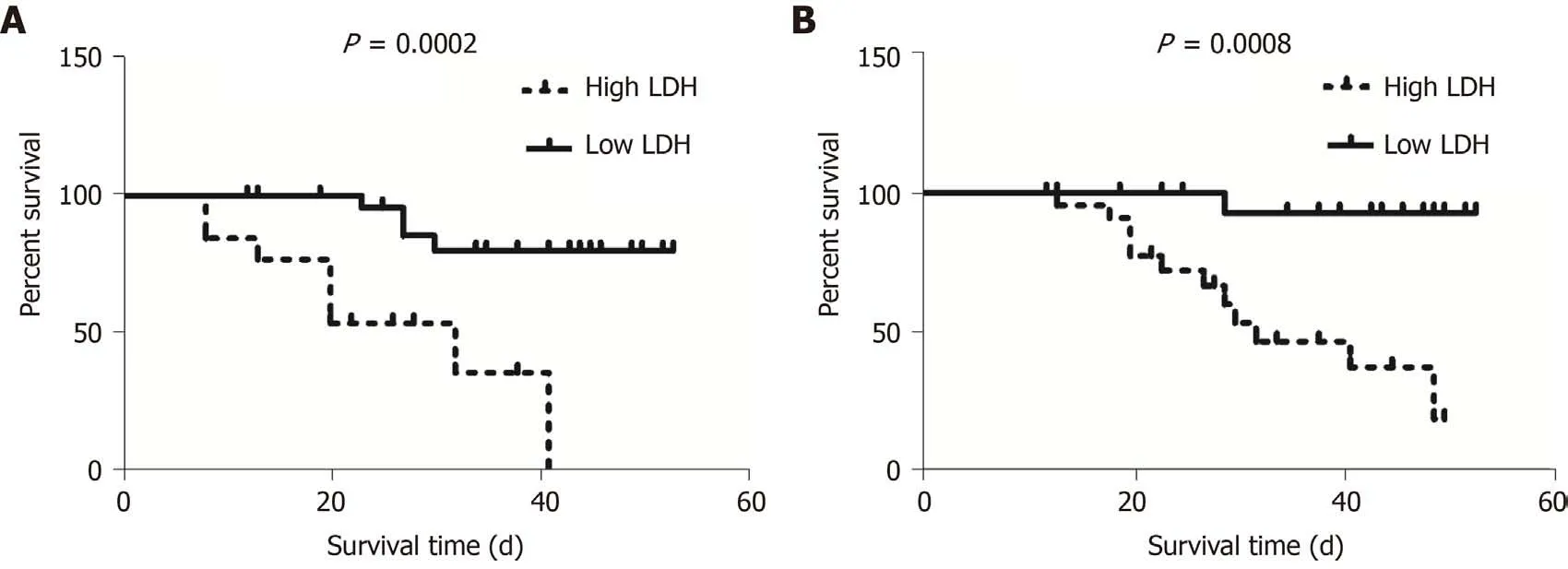
Figure 3 Association between the first value of serum lactate dehydrogenase and survival time of patients with critical coronavirus disease 2019. Kaplan-Meier analysis and the log-rank test were performed to analyze the association between the first values of serum lactate dehydrogenase(LDH) and the survival time of patients with critical coronavirus disease 2019. A:Patients with high LDH (≥ 397.0 U/L) had a significantly shorter survival time compared to those with low LDH (< 397.0 U/L) in the alveolitis phase; B:Patients with high LDH (≥ 263.0 U/L) also had a significantly shorter survival time compared to those with low LDH (< 263.0 U/L) in the fibrosis phase. LDH:Lactate dehydrogenase.
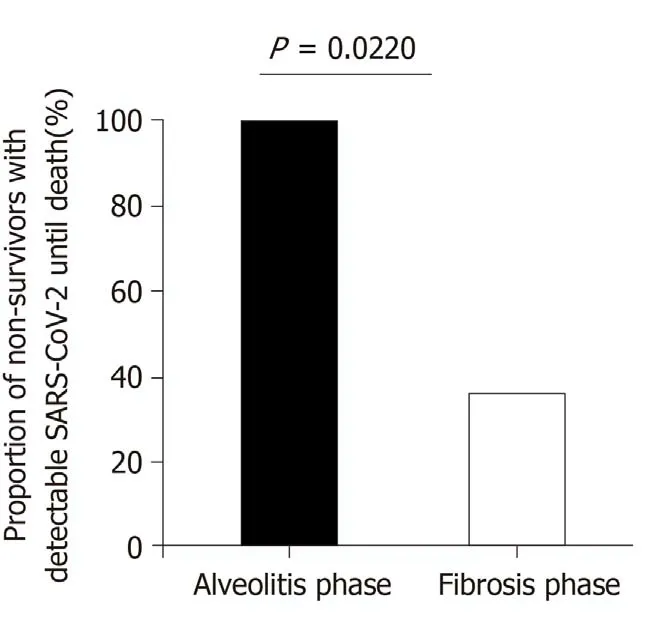
Figure 4 Proportion of non-survivors with detectable severe acute respiratory syndrome coronavirus 2 until death in the alveolitis and fibrosis phase. All non-survivors (100.0%) who died in the alveolitis stage had a persistent positive test for severe acute respiratory syndrome coronavirus 2 until death. Only 5 patients (35.7%) who died in the pulmonary fibrosis stage had positive virus nucleic acid test results. SARS-CoV-2:Severe acute respiratory syndrome coronavirus 2.
Possible sources of elevated serum LDH levels during infection may be immunologic changes after SARS-COV-2 infection of the upper and lower respiratory tract which result in an early acute respiratory inflammatory response with consequent release of pro-inflammatory cytokines,including interleukin-1β,followed by inflammasome activation and production of active mature interleukin-1β which is a mediator of lung inflammation and fibrosis[27]. High levels of serum LDH were also reported to be associated with the severe form of H1N1 influenza,and serum LDH level above 500 U/L was significantly more common in patients with pneumonia[21,28].Lung parenchymal cells and/or local inflammatory cells may be potential sources of elevated LDH in serum[29,30]and elevated serum values of LDH indirectly indicate lung tissue damage[31,32]. Therefore,the best LDH threshold for predicting COVID-19 in the acute alveolitis phase was higher than that in the fibrosis phase. The first,lowest and highest values of LDH in the alveolitis and fibrosis phase,together with more days with high LDH and a higher ratio of days with high LDH levels,were important for predicting the severity of critical COVID-19. As critical COVID-19 in the ICU is often combined with bacterial infection,LDH can convert pyruvate to lactate and might be the key enzyme for pneumococcal pyruvate metabolism and thus pneumococcal survival in blood[33].
CONCLUSION
High serum LDH and dyspnea symptoms in the early stages of infection may predict the severity and poor prognosis in patients with critical COVID-19. The disease in nonsurvivors developed rapidly in both the alveolitis stage and fibrosis stage,and the progressive fibrosis stage may be more perilous than the alveolitis stage,even if SARSCoV-2 is undetectable.
ARTICLE HIGHLIGHTS
Research background
Millions of new coronavirus disease pneumonia (coronavirus disease 2019,COVID-19)cases have been reported worldwide. Moreover,the prognosis of critically ill and severe COVID-19 patients is extremely poor.
Research motivation
COVID-19 patients may have increased serum lactate dehydrogenase (LDH) levels in the early stage. The clinical changes in LDH may have predictive value in disease evolution and prognosis in critically ill COVID-19 patients.
Research objectives
To describe the clinical characteristics and examine the clinical changes in LDH in the alveolitis and fibrosis stages according to computed tomography findings in critically ill COVID-19 patients and their predictive value for clinical prognosis.
Research methods
We analyzed the clinical data of forty-seven critical COVID-19 patients in the intensive care unit of the Third People's Hospital of Yichang City and divided them into nonsurvivors and survivors. Clinical data including symptoms,detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),chest computed tomography images,changes in serum LDH in different clinical phases,and prognosis were collected.
Research results
Most non-survivors died in the fibrosis stage. Non-survivors had fewer days of hospitalization,shorter disease duration,shorter duration of alveolitis and fibrosis,and had dyspnea symptoms at disease onset. Both first and lowest LDH values in the alveolitis and fibrosis stage were more pronounced in non-survivors than in survivors.Importantly,patients with high LDH had a significantly shorter median survival time in the alveolitis and fibrosis phase.
Research conclusions
High serum LDH and dyspnea symptoms in the early stages of infection were positive predictors of severity and poor prognosis in patients with critical COVID-19. The rapid progressive fibrosis stage was more perilous than the alveolitis stage,even if SARSCoV-2 is undetectable.
Research perspectives
The immunologic mechanism of elevated serum LDH during SARS-COV-2 infection requires further investigation.
ACKNOWLEDGEMENTS
Thanks to all the medical teams that went to Hubei province to battle the COVID-19 epidemic in China. The authors thank Yujie Lin for reviewing and editing the article.
杂志排行
World Journal of Clinical Cases的其它文章
- COVID-19:A review of what radiologists need to know
- Holistic care model of time-sharing management for severe and critical COVID-19 patients
- Bioequivalence of two esomeprazole magnesium enteric-coated formulations in healthy Chinese subjects
- Osteoprotegerin,interleukin and hepatocyte growth factor for prediction of diabetes and hypertension in the third trimester of pregnancy
- Risk factors analysis of prognosis of adult acute severe myocarditis
- Sonographic features of umbilical vein recanalization for a Rex shunt on cavernous transformation of portal vein in children
