Clinical value of needleless sling in treatment of female stress urinary incontinence
2020-04-08YuGuoChenYaoGuangZhangWeiZhangXinLiXiaWang
Yu-Guo Chen,Yao-Guang Zhang,Wei Zhang,Xin Li,Xia Wang
Yu-Guo Chen,Dressing Room of Surgical Outpatient,Beijing Hospital,National Center of Gerontology;Institute of Geriatric Medicine,Chinese Academy of Medical Sciences,Beijing 100730,China
Yao-Guang Zhang,Wei Zhang,Department of Urology,Beijing Hospital,National Center of Gerontology;Institute of Geriatric Medicine,Chinese Academy of Medical Sciences,Beijing 100730,China
Xin Li,Xia Wang,Nursing Department,Beijing Hospital,National Center of Gerontology;Institute of Geriatric Medicine,Chinese Academy of Medical Sciences,Beijing 100730,China
Abstract BACKGROUND Stress urinary incontinence(SUI)is a common disease in women.The emergence of the needle-free sling has led to a new clinical treatment for SUI in women.AIM To explore the clinical value of the needleless sling without acupuncture in the treatment of SUI in women.METHODS From February 2017 to November 2018,according to the order of admission,44 patients(mid-suspension group)were treated by tension-free transobturator urethral suspension,and 44 patients(non-acupuncture group)were treated with a needleless non-acupuncture band.The clinical effects of the two treatments were evaluated.RESULTS There was no significant difference between the two groups in the total clinical effectiveness rate(P = 0.374),but intraoperative blood loss and visual analogue scale score at postoperative day 1 were significantly lower in the non-acupuncture suspension group than in the middle urethral suspension group(P = 0.396).The incidence of complications in the needle-free sling group was significantly lower than that in the middle urethral suspension group(P = 0.025).CONCLUSION The clinical effectiveness of acupuncture-free suspension in treating SUI in female patients is better than that of traditional tension-free transobturator mid-urethral suspension.
Key Words:No needle sling;Female stress urinary incontinence;Mid-urethral suspension;Controlled study;Complications;Application value
INTRODUCTION
Stress urinary incontinence(SUI)is a common disease in women[1,2].It is mainly characterized by the involuntary overflow of urine when there is a sudden rise in abdominal pressure caused by actions such as coughing,laughing,and exertion,and it does not persist in daily life[3].According to an epidemiological analysis,female SUI mainly occurs in middle-aged and elderly women.The current global incidence of female SUI is approximately 12.5%-22.5%,while the incidence of female SUI in China is 18.9-28.0%,which is higher than the international average[4].
The severity of SUI varies;patients with mild cases only have very little urine overflow,which leads to a small impact on daily life,but some severe urinary incontinence cases lead to more urine overflow,which seriously affects patients’ daily life.At present,there are many methods available for treating stress incontinence,such as life feedback training and pelvic floor muscle function exercises.However,these kinds of treatment are time-consuming and have highly variable curative effects[5].
Tension-free mid-urethral suspension is a common surgical treatment,but some scholars have pointed out that there are some potential risks of the surgical treatment,such as puncture site injuries,hematomas,and long-lasting inguinal area pain;in addition,patients generally develop severe pain after the operation,and the clinical applications are also limited[6,7].With advancements in medicine,the emergence of the needle-free sling has led to a new clinical treatment for SUI in women.However,there are relatively few clinical reports on this treatment.Thus,the clinical value of the needle-free sling is further analyzed in this paper.
MATERIALS AND METHODS
Basic information
Eighty-eight women with SUI were admitted to our hospital during the period from February 2017 to November 2018.All the patients were diagnosed with and treated for SUI in accordance with the guidelines(2017)formulated by the gynecological pelvic floor study group of the Chinese Medical Association.According to the standards for diagnosis and treatment,patients were listed in the order of admission,and patients receiving an even number were included in a needleless sling group.Forty-four patients who were treated by tension-free transobturator urethral suspension were included in a mid-suspension group.The basic characteristics of the two groups were not significantly different,and the corresponding data and test values are shown in Table 1.The study was approved by the Ethics Committee of our hospital.
Inclusion and exclusion criteria
The inclusion criteria were as follows:(1)Cough,laughter,and other abdominal pressure rise leading to a large amount of urine leakage;(2)Positive finger pressure test result;(3)Urine blood test result confirming that bladder detrusor function is not abnormal;(4)Absence of urethral infection;and(5)Provision of informed consent for the treatment plan,with a form that was voluntarily signed.
The exclusion criteria were as follows:(1)Pelvic floor muscle function training was underway before admission;(2)History of vaginal surgery or pelvic surgery;(3)Urinary incontinence caused by bladder outlet obstruction;(4)Mixed urinary incontinence or neurogenic urinary incontinence;and(5)Incomplete baseline data.
Methods
In the middle segment urethral suspension group,the patients were placed the lithotomy position,and general anesthesia or lumbar hard combined anesthesia was induced.The anterior vaginal wall was cut,tissue scissors were used to separate the vaginal wall to the side of the urethra,it was separated to the lower pubic branch,and a 0.5 cm incision was made at the inner angle of the closed hole on both sides.The wing guide was inserted at the upper part of the incision of the urethral orifice,and the puncture needle passed through the side space of the pubic branch-closed holeinguinal incision.In the needleless sling group,the patients were placed in the lithotomy position,and general anesthesia or waist hard joint anesthesia was induced.An incision was made in the urethral mouth measuring 1 cm,the vaginal forearm was cut,the blunt separation was performed along the line at 10 o'clock and 12 o' clock,and the lower pubic branch was separated.The bending forceps were used to clamp the T-type pocket without the needle sling,passing through the completed separation gap from the 10 o'clock direction,reaching the posterior edge of the lower pubic branch.The bending forceps were opened to perform the T-type pocket position,and sling-tie fixation was completed in the internal closed hole muscle.The above operation was repeated along the side from the 2-clock direction.The position of the Ttype pocket was adjusted on both sides,and the blue line of the middle sling was aligned with the middle line.After the calibration line was removed,the surgical incision was cleaned and sutured.
Curative effect evaluation and observation indexes
The treatment was considered highly effective when the SUI symptoms basically disappeared and the cough-leak urine test result was negative.It was considered effective when pressure urinary incontinence symptoms were still present and the cough-leak urine test result was positive but the volume of urine leakage was reduced by less than 50% compared with before treatment.The treatment was considered invalid when the urinary incontinence symptoms were still present and the volume of urine leakage was reduced by < 50%.The total clinical effectiveness rate was calculated as(number of cured cases + number of valid cases)/total number of cases ×100%.
A one-year follow-up was conducted to assess the quality of life of the patients before and 12 mo after the operation.The evaluation tools used were the ICIQ-SF questionnaire and the IIQ-7 questionnaire.
The pain assessment was performed at postoperative day 1 by using the visual analogue scale(VAS)with a total score of 0 to 10 points,which was proportional to the degree of pain.The incidence of urinary retention,infection,hematomas,and other complications was calculated.
Statistical analysis
SPSS 23.0 software was used to analyze the data.Continuous data(± SD)were analyzed using thettest,and count data(%)were analyzed using the chi-squared test.P< 0.05 indicated statistical significance.
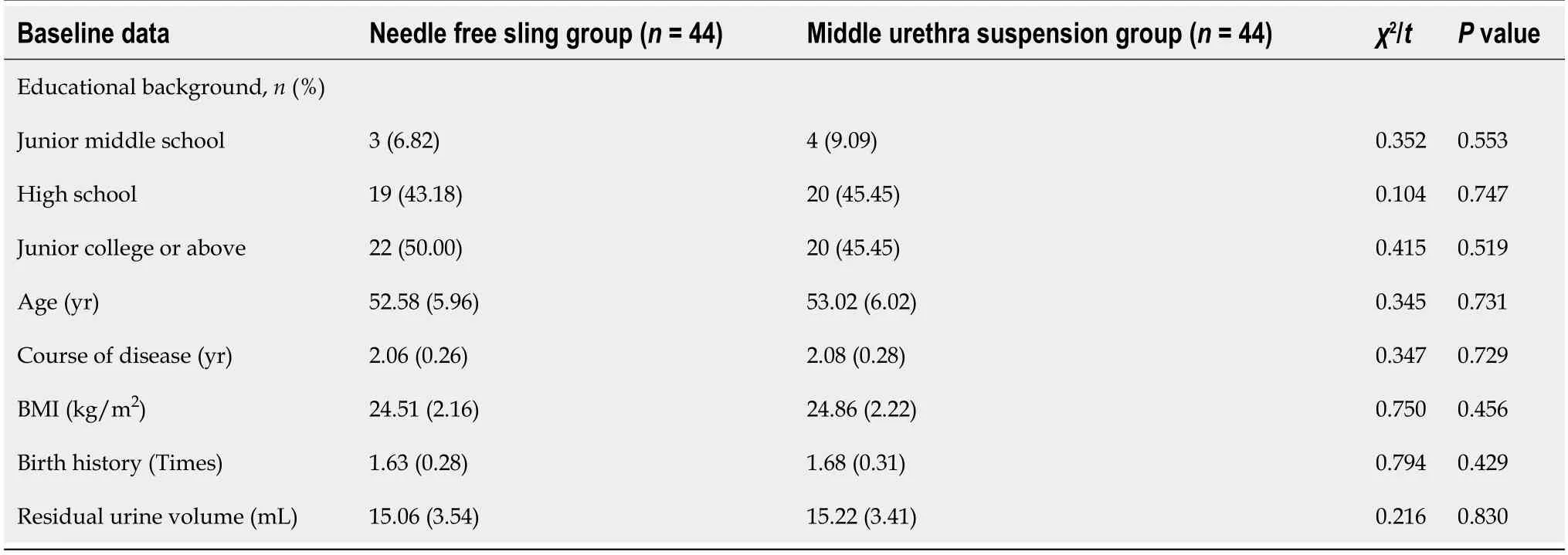
Table 1 Comparison of baseline data between the two groups
RESULTS
Comparison of clinical curative effect between the two groups
There was no statistically significant difference in the total clinical efficiency between the needle-free sling group and the urethral mid-suspension group(P= 0.374),and the data are shown in Table 2.
Comparison of complications between the two groups
The incidence of complications in the needle-free sling group was significantly lower than that in the middle segment of the urethra suspension group(P= 0.025),as shown in Table 3.
Comparison of perioperative observation indexes between the two groups
The volume of blood loss was significantly smaller,the operative time was significantly shorter,and the 1 d VAS score was significantly lower in the needleless sling group than in the middle urethral suspension group(P= 0.001,0.001,and 0.001,respectively).However,the total length of stay was not statistically significant between the two groups(P= 0.225),as detailed in Table 4.
Comparison of quality of life scores between the two groups
According to the data shown in Table 5,at 12 mo after the operation,the ICIQ-SF and IIQ-7 scores decreased significantly in both groups compared with those before the operation,but the scores were not significantly different between the two groups(P=0.713,0.628,0.859,and 0.396,respectively).
DISCUSSION
According to physiological anatomy,the female urethra is shorter than the male urethra and is more prone to SUI,which is mainly characterized by the uncontrolled overflow of urine under conditions such as coughing and laughing[8].Clinical studies have suggested that related factors that can induce SUI include a decline in urethral sphincter function caused by aging,pelvic floor muscle group injury caused by fertility,and pelvic organ prolapse[9].In view of the impact of this disease on women's daily life,there is no effective intervention,and long-term complications include lower abdomen pain,pudendal skin ulceration,bladder lithotomy,urinary system infection,and other serious complications;thus,timely and effective treatment is required[10].
At present,the commonly used treatment methods include routine pelvic floor muscle rehabilitation exercises and biofeedback training,which can improve the symptoms of SUI by restoring pelvic floor muscle function.However,in clinical practice,these kinds of conservative treatment should be carried out for a long time,and some patients cannot continue to perform these exercises for a sufficiently long time for the treatment to be effective[11].Surgical treatment is another common optionfor the clinical treatment of SUI in these patients.
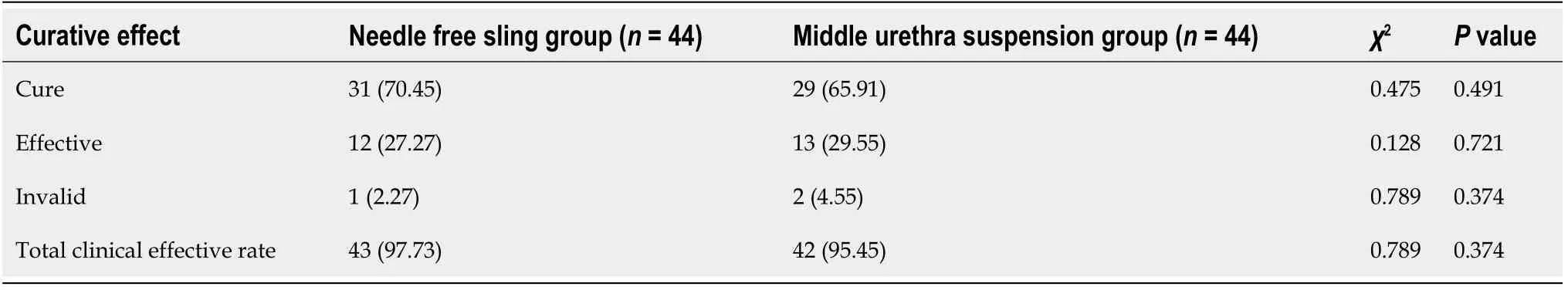
Table 2 Comparison of therapeutic effect between the two groups,n(%)
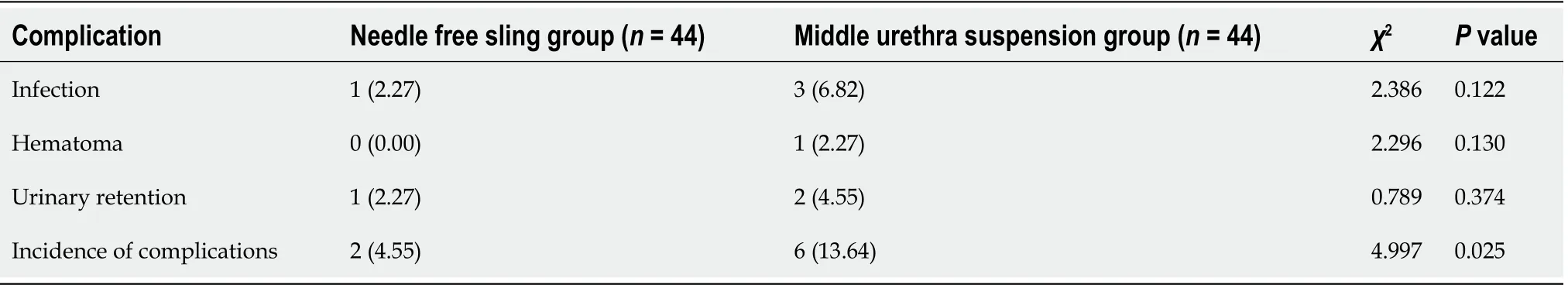
Table 3 Comparison of complications between the two groups,n(%)
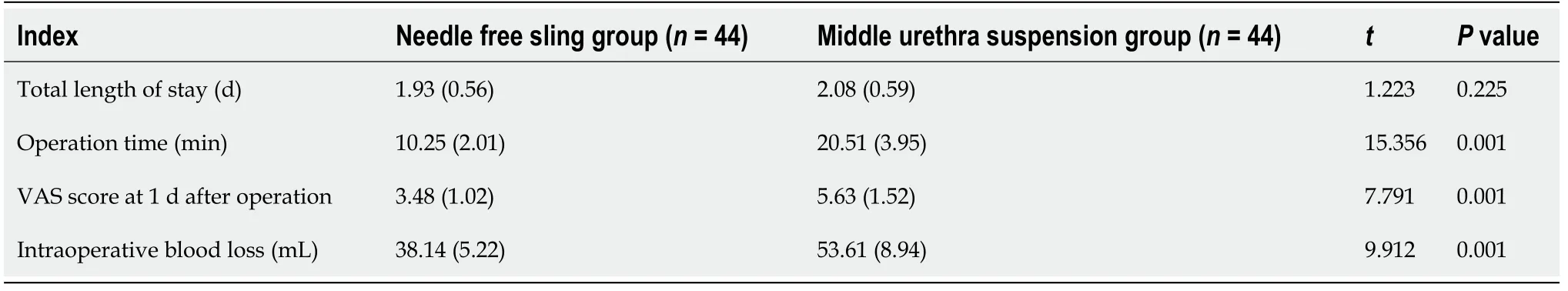
Table 4 Comparison of several perioperative observation indexes between the two groups
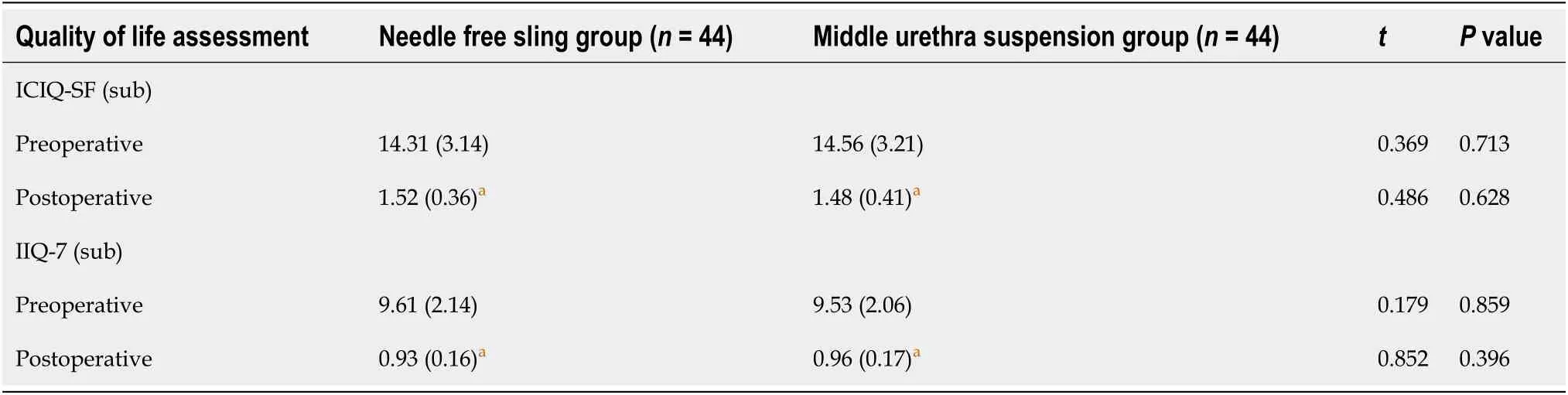
Table 5 Comparison of quality of life scores between two groups
Studies conducted outside of China have suggested that the pubic ligament and pubic tail muscle are similar to the hammocks in the female middle urethra.When the structure is destroyed,the abdominal pressure may rise,that is,urinary incontinence may occur.In clinical treatment,the reconstruction of a hammock structure can effectively treat urinary incontinence.Tension-free urethral mid-suspension(TVT)is based on this theory[12].TVT has been used widely in clinical practice,with favorable curative effects,and the success rate of the operation is as high as 86%-99%.However,a follow-up study showed that patients need to undergo bladder examinations,which can easily cause bladder perforation,hematomas,and complications such as dysuria after the operation.The treatment has been improved to include an improved puncture path,and the improved treatment is referred to as tension-free transobturator urethral suspension(TVT-O).Essentially,the puncture is performed through the obturator rather than the traditional puncture path,and the posterior pubic region is avoided.Compared with the TVT operation,TVT-O significantly reduces the risk of bladder perforation,but it can increase the severity of inguinal pain in patients during the puncture,and there are some limitations in the application[13].Single incision slinging(SIMS)was developed to improve the TVT-O operation[14].It does not require punctures through the posterior space or obturator,but the total area of the sling is 6.5 cm2,which is much lower than the area of the TVT and TVT-O slings(16.5 cm2).In clinical practice,there are limitations of using short slings and a relatively small area of support,which can easily lead to a decline in the sexual quality of life of patients and vaginal perforation[15,16].
Needleless straps,as a product of modern medical advancements,have been designed by Spanish doctors to further improve the technique[17].The two ends of a Ttype bag are used for the needle-free sling and as a whole are considered a "worker"type;the length of the sling is 11.4 cm,the width of the pockets at both ends is 2.2 cm,and the width of the middle of the sling is 1.2 cm.The non-knot knitting technique used in the needleless sling can prevent the formation of a dead cavity after implantation with knots,as is common with the traditional sling,resulting in a large number of bacterial propagation and infection defects;in addition,the nonwoven structure gives the sling a certain degree of freedom inside the soft tissue of the patients,which can significantly reduce discomfort in patients after the sling is implanted and prevent a decline in their sexual quality of life[18].In addition,the large aperture design used in sling knitting enables growth and fast recovery after implantation,and its contact area is 16.08 cm2larger than twice the support area of SIMS.In recent years,the needleless sling has gradually been accepted by patients,and the acceptance by clinicians is high[19].
Overall,needleless straps have the advantages of SIMS and TVT-O,and the T-type pocket without needle straps can be directly fastened to the obturator muscle of the patient.The area of the straps is larger and the support effect is stronger with the needleless technique compared with SIMS,and the effect of urinary incontinence treatment is similar to that of TVT-O.The use of SIMS with the single-section approach can effectively prevent the occurrence of bladder perforation,nerve injury and other adverse events,and it can also effectively reduce the risk of postoperative dysuria,pain,decline in patients’ sexual quality of life,and other complications[20].In this study,there was no significant difference in the total effectiveness rate and the quality of life score on the questionnaire between the needleless and middle urethra suspension group at 12 mo after the operation.The results showed that the effect of needleless suspension and TVT-O in the treatment of female SUI was basically the same,but the VAS score at postoperative day 1,intraoperative blood loss,and postoperative complications were better than those in the middle urethra group.There was no significant difference in the total length of hospital stay between the two groups.The results showed that the two procedures were minor and the patients recovered rapidly,so the total length of hospital stay was not significantly different.
Changet al[19]compared the results of the clinical treatment of female SUI by the needleless sling and conventional TOT(TVT-O).The results of the perioperative time,VAS score at postoperative day 1,intraoperative blood loss,and hospitalization time were better in the needleless group than in the TOT group.There was no significant difference between the two groups in the ICIQ-SF scores or the average quality of life between the two groups.According to Xuet al[2],the results showed that the incidence of postoperative complications in the observation group was significantly lower than those in the control group(TVT-O),but there was no significant difference in the total clinical efficiency or quality of life scores between the two groups.However,the number of patients included in this study is small,and the results of the study may be affected by the small sample size;however,the differences were large,and future studies with larger sample sizes need to be conducted.
In summary,the clinical effectiveness of the two treatment options,TVT-O and the needleless sling,are basically the same in the clinical treatment of SUI in women,but the needleless sling has the advantages of fewer complications,shorter operative time,and milder postoperative pain in patients.
ARTICLE HIGHLIGHTS
Research background
The emergence of the needle-free sling has led to a new clinical treatment for stress urinary incontinence in women.
Research motivation
Explore the new treat in stress urinary incontinence.
Research objectives
Analyzed the clinical value of the needle-free sling is further in this paper.
Research methods
Choose 44 patients in the mid-suspension group treated by tension-free transobturator urethral suspension,and 44 patients in the non-acupuncture group.
Research results
There was no significant difference between the two groups in the total clinical effectiveness rate,but the intraoperative blood loss and the postoperative 1 d visual analogue scale score were significantly lower in the non-acupuncture suspension group than in the middle urethral suspension group.The incidence of complications in the needle-free sling group was significantly lower than that in the middle urethral suspension group.
Research conclusions
The needleless sling had the advantages of fewer complications,a shorter operative time and milder postoperative pain in patients,which could be actively promoted.
Research perspectives
The concept of minimally invasive and people-oriented should be widely used in clinical nursing.
杂志排行
World Journal of Clinical Cases的其它文章
- Special features of SARS-CoV-2 in daily practice
- Gastrointestinal insights during the COVID-19 epidemic
- From infections to autoimmunity:Diagnostic challenges in common variable immunodeficiency
- One disease,many faces-typical and atypical presentations of SARS-CoV-2 infection-related COVID-19 disease
- Application of artificial neural networks in detection and diagnosis of gastrointestinal and liver tumors
- Hepatic epithelioid hemangioendothelioma:Update on diagnosis and therapy