Gastrointestinal insights during the COVID-19 epidemic
2020-04-08KaiNieYuanYuanYangMinZiDengXiaoYanWang
Kai Nie,Yuan-Yuan Yang,Min-Zi Deng,Xiao-Yan Wang
Kai Nie,Yuan-Yuan Yang,Min-Zi Deng,Xiao-Yan Wang,Department of Gastroenterology,The Third Xiangya Hospital of Central South University,Changsha 410000,Hunan Province,China
Abstract Coronavirus disease-2019(COVID-19)has so far caused hundreds of mortalities worldwide.Although respiratory symptoms are the main complication in COVID-19 patients,the disease is also associated with gastrointestinal problems,with diarrhea,nausea,and vomiting being primary COVID-19 symptoms.Thus,cancer and inflammatory bowel disease(IBD)management,stool viral tests,and virus exposure are major concerns in the context of COVID-19 epidemic.In patients with colorectal cancer and IBD,the colonic mucosa exhibits elevated angiotensin-converting enzyme 2 receptor levels,enhancing COVID-19 susceptibility.In some cases,positive viral stool tests may be the only indicator of infection at admission or after leaving quarantine.Without supplemental stool tests,the risk of undetected COVID-19 transmission is high.Moreover,viral exposure during the regular or emergency endoscopic examination should be avoided.We carefully discuss key gastrointestinal concerns with regard to COVID-19 and call for more attention to such problems.
Key Words:COVID-19;SARS-CoV-2;Diarrhea;Colorectal cancer;Inflammatory bowel disease;Stool tests
INTRODUCTION
Coronavirus disease-2019(COVID-19),caused by infection with severe acute respiratory syndrome coronavirus 2(SARS-CoV-2),has so far killed hundreds of thousands worldwide.Like SARS-CoV(severe acute respiratory syndrome coronavirus),SARS-CoV-2 enters host cellsviathe interaction of viral spike(S)protein with the human angiotensin-converting enzyme 2(ACE2)receptor.Clinically,COVID-19 patients frequently present with gastrointestinal symptoms,including diarrhea,nausea,and vomiting.Additionally,a significant number of patients are positive for stool viral RNA.A study revealed that ACE2 is abundantly expressed in the small intestine,lung epithelium,and vascular endothelium,indicating multiple human infection routes[1].ACE2 normally localizes on the luminal epithelial cells and may perform its enzymatic activity isolated from the cell membrane[2,3].ACE2 localization offers efficient infection routes through the airway and gastrointestinal tract.Singlecell sequencing analysis indicates that ACE2 is abundant in enterocytes of the mouse small intestine,especially in proximal and distal enterocytes[4].Moreover,COVID-19 patients’ mucosal biopsies revealed viral nucleocapsid protein(NP)in gastric,duodenal,and rectum glandular epithelial cells,but not in the esophagus.Together,such evidence suggests that the gastrointestinal epithelium is a coronavirus infection route[5].
After reviewing reported COVID-19 studies,we formatted several concepts.Gastrointestinal problems may contribute to the complexity and infectivity of COVID-19.Patients with COVID-19 may exhibit uncharacteristic symptoms like diarrhea.Patients with digestive disease bear a relatively high risk of SARS-CoV-2 infection.Stool viral test could help us screen out atypical infectors.Viable virus detected in stool brings a fecal transmission risk.Thus,it is important to discuss several essential gastrointestinal topics about COVID-19.
GASTROINTESTINAL SYMPTOMS IN COVID-19
Holshue made the earliest report of virus nucleic acid detection in a COVID-19 patient stool[6].The risk of gastrointestinal infection by SARS-CoV-2 has attracted attention from gastroenterologists.Here,we conducted an overall COVID-19 case collection study to establish digestive involvement in COVID-19 patients and found 39 studies that included detailed symptom descriptions[5-43](Table 1),excluding case reports and small cohorts.Diarrhea is the most common digestive symptom,with its incidence ranging from 1.2-35%.The overall diarrhea incidence rate in our collection is 6.34%,while in the largest cohort,the diarrhea incidence rate was 3.8%.The cohorts with a patient number > 80 revealed an about 5% incidence.The second most common gastrointestinal symptom is nausea/vomiting,which affected 5.17% of assessed COVID-19 patients.Other gastrointestinal symptoms,including anorexia,belching,abdominal pain,and gastrointestinal bleeding,affected < 1% of the patients.Most critically ill COVID-19 patients experience coagulation disorders,which carry a high risk of gastrointestinal bleeding.Diarrhea diagnosis may differ across centers.Due to a lack of awareness,clinicians may underestimate the value of gastrointestinal symptoms in COVID-19 diagnosis and clinical management.An exhaustive description of COVID-19 gastrointestinal symptoms has been made in two cohorts by Zhanget al[39]and Moet al[41].While respiratory symptoms are the main feature of COVID-19,more attention should be paid to gastroenterology.In some cases,gastrointestinal symptoms,including diarrhea and vomiting,may be the first and sometimes the only signs of COVID-19[8,25].Thus,physicians should consider COVID-19 infection in patients presenting with digestive symptoms in high transmission areas.
RISK TO GASTROINTESTINAL CANCER PATIENTS
A recent study recruited 18 COVID-19 cases with a history of cancer from 575 Chinesehospitals.Of these,three had a history of colorectal cancer(one colonic tubular adenocarcinoma,one rectal carcinoma,and one colorectal carcinoma).That study observed an increased COVID-19 risk to cancer patients,who deteriorated more rapidly than patients without cancer[44].However,other factors,including age,may confound conclusions as older people have a higher cancer and COVID-19 risk[45,46].However,an RNA analysis involving two cohorts of healthy adults and gastrointestinal cancer patients,found elevated ACE2 expression in colorectal cancer patients relative to healthy controls.This finding suggests that gastrointestinal cancer patients may be more susceptible to SARS-CoV-2 infection[47].Thus,there is a concern about greater COVID-19 risk in advanced stage cancer patients or those on immunosuppressants.However,more rigorous studies are required to draw definite conclusions and patients with gastrointestinal cancers should be cautiously managed.To this end,several approaches have been recommended,including multidisciplinary therapy(MDT)involving respiratory physicians,postponement of elective operations with neoadjuvant therapy,and minimizing endoscopic interventions[48,49].
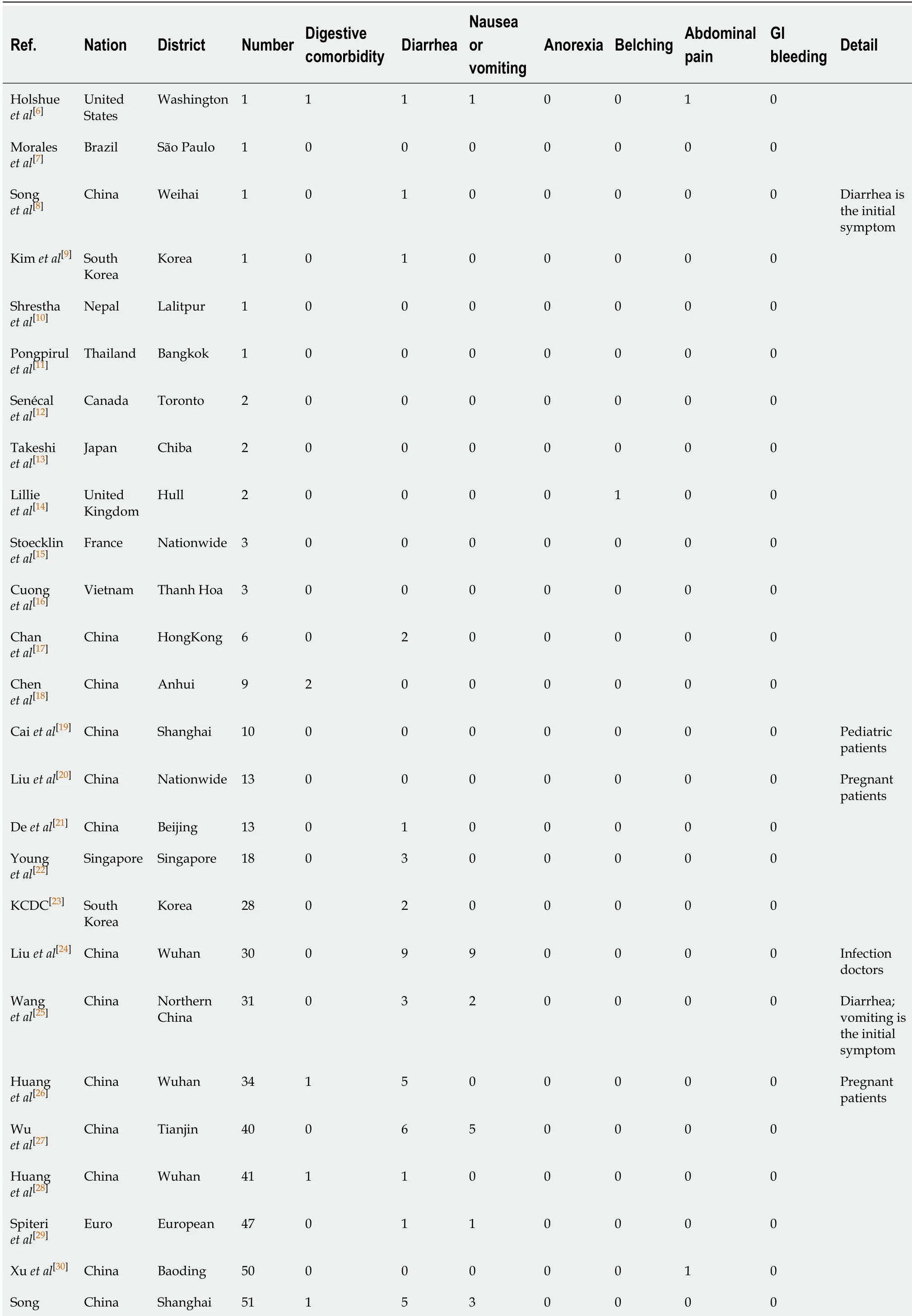
Table 1 Incidence of gastrointestinal symptoms in coronavirus disease-2019 patients
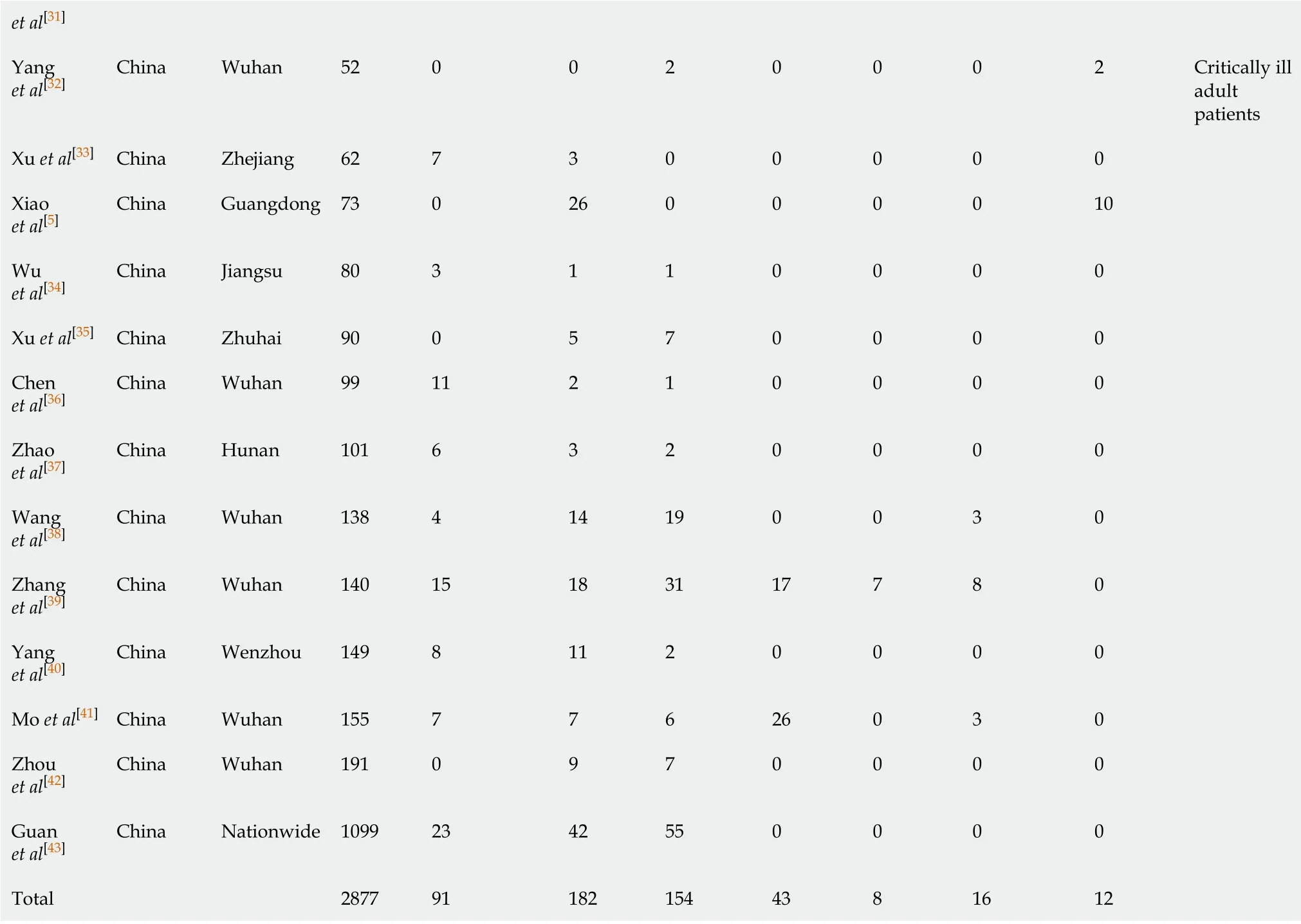
et al[31]Yang et al[32]China Wuhan 52 0 0 2 0 0 0 2 Critically ill adult patients Xu et al[33]China Zhejiang 62 7 3 0 0 0 0 0 Xiao et al[5]China Guangdong 73 0 26 0 0 0 0 10 Wu et al[34]China Jiangsu 80 3 1 1 0 0 0 0 Xu et al[35]China Zhuhai 90 0 5 7 0 0 0 0 Chen et al[36]China Wuhan 99 11 2 1 0 0 0 0 Zhao et al[37]China Hunan 101 6 3 2 0 0 0 0 Wang et al[38]China Wuhan 138 4 14 19 0 0 3 0 Zhang et al[39]China Wuhan 140 15 18 31 17 7 8 0 Yang et al[40]China Wenzhou 149 8 11 2 0 0 0 0 Mo et al[41]China Wuhan 155 7 7 6 26 0 3 0 Zhou et al[42]China Wuhan 191 0 9 7 0 0 0 0 Guan et al[43]China Nationwide 1099 23 42 55 0 0 0 0 Total 2877 91 182 154 43 8 16 12
RISK TO INFLAMMATORY BOWEL DISEASE PATIENTS
Inflammatory bowel disease(IBD)is characterized by impaired mucosal permeability and sustained immune disorder.To date,several cases of SARS-CoV-2 infection in IBD patients have been reported.However,IBD patients on immunosuppressants should be cautious in COVID-19 prevention.Experimental induction of colitis elevated colonic ACE2 expression[50],and plasma ACE2 concentration is reported to be elevated in IBD patients relative to healthy controls[51].Proteomic analysis showed a significant colonic ACE2 elevation in Crohn’s disease relative to ulcerative colitis[52].Thus,IBD may increase susceptibility to SARS-CoV-2.Colonic fibrosis is inversely correlated with mucosal ACE2 expression.IBD patients on RAS inhibitors are less likely to undergo surgery and hospitalization.Taken together,ACE inhibitors should be taken into consideration as a means of decreasing ACE2 levels and improving colonic fibrosis.During the COVID-19 pandemic,IBD patients with hypertension,diabetes,or chronic kidney disease may benefit from ACE inhibitors.Additionally,clinical management of IBD should avoid unnecessarily raising immunosuppressant dosage and optimize treatment with biologics[53].
STOOL VIRAL TEST DURING COVID-19 MANAGEMENT
The positive rate for fecal viral RNA varies from 29%-55%[54,55].In some cases,stool viral RNA may be the only indicator of COVID-19 at admission.Zhanget al[56]reported two COVID-19 cases positive for fecal RNA,but with negative pharyngeal swabs at admission.Additionally,four patients exhibited delayed positive results for stool RNA and persistent negative results in pharyngeal specimens.Additionally,symptomatic and asymptomatic infections may be fecal virus-positive but pharyngeal virusnegative[57,58].A recent case report described a patient with a history of gastrectomy for gastric cancer and diarrhea,who was positive for fecal RNA but negative for pharyngeal RNA[59].Importantly,patients may be stool virus-positive but virusnegative after treatment.Previous retrospective cohorts reported a mean fecal viral shedding duration of 27.9 d after symptom onset,compared to 16.7 d in respiratory samples[59].The longest reported fecal viral shedding duration is 49 d[60].This phenomenon has been attributed to SARS-CoV-2’s affinity for gastrointestinal ACE2,which is abundantly expressed in the small intestines[1].Additionally,COVID-19 patients’ mucosal biopsies revealed viral nucleocapsid protein(NP)in gastric,duodenal,and rectum glandular epithelial cells.Furthermore,the co-existence of ACE2 and SARS-CoV-2 in the enteric epithelium underlies colonic viral shedding[5].Given that false-negatives occur in respiratory viral tests,these stool positive cases highlight the risk of undetected COVID-19 when relying solely on respiratory viral detection in clinical practice.The prolonged stool virus shedding duration may result from a longer duration of gastrointestinal viral infection.Importantly,the presence of viable virus in stool emphasizes the risk of fecal transmission,and need for stool tests in the population[2].Chinese researchers have independently observed viable SARSCoV-2 in COVID-19 patients’ stool(unpublished data).The absence of gastric acid might facilitate gastrointestinal virus infection and induce COVID-19 associated enteritis.Thus,the release from quarantine based on negative respiratory results alone may carry the risk of continued community spread.
RISK OF GASTROINTESTINAL DAMAGE AND VIRAL EXPOSURE
Although evidence on COVID-19 gastrointestinal mucosa damage is limited,a recent endoscopic study on COVID-19 patients did not observe damage in the esophagus,stomach,duodenum,and rectum[5].However,concerns over gastrointestinal bleeding in critically ill COVID-19 patients should be considered as they often have coagulation disorders.Preventive proton pump inhibitors may be considered for specific cases.Gastroenterologists and endoscopists face exposure to the virus during endoscopic operations[61].Thus,regular endoscopic interventions should not be suggested during the pandemic,and emergency bleeding interventions should be performed with sufficient precautions.
CONCLUSION
Physicians should be aware of the COVID-19 risk in patients with gastrointestinal disorders,especially those with colorectal cancer and IBD.Preventions and domiciliary quarantine should be progressed under equal medical advice.Here,we highlight the need for stool viral tests as a supplement to conventional screening tests for COVID-19 in patients with gastrointestinal disorders and people leaving quarantine.In addition to regular respiratory sampling,stool viral tests should be carried out in populations with histories of exposure and travel to epidemic areas,advanced age,obesity,cancer,and cardiopulmonary comorbidities,as well as in pregnant women and children.
杂志排行
World Journal of Clinical Cases的其它文章
- Special features of SARS-CoV-2 in daily practice
- From infections to autoimmunity:Diagnostic challenges in common variable immunodeficiency
- One disease,many faces-typical and atypical presentations of SARS-CoV-2 infection-related COVID-19 disease
- Application of artificial neural networks in detection and diagnosis of gastrointestinal and liver tumors
- Hepatic epithelioid hemangioendothelioma:Update on diagnosis and therapy
- Streptococcus agalactiae:Identification methods,antimicrobial susceptibility,and resistance genes in pregnant women