Neoadjuvant targeted therapy for apocrine carcinoma of the breast:A case report
2020-04-07PingYangShuJiaPengYanMingDongLinYangZhenYuYangXiHuGuoQiangBao
Ping Yang, Shu-Jia Peng, Yan-Ming Dong, Lin Yang, Zhen-Yu Yang, Xi-E Hu, Guo-Qiang Bao
Ping Yang, Shu-Jia Peng, Yan-Ming Dong, Lin Yang, Zhen-Yu Yang, Xi-E Hu, Guo-Qiang Bao,Department of General Surgery, Tangdu Hospital, Air Force Military Medical University,Xi’an 710032, Shaanxi Province, China
Abstract BACKGROUND Apocrine carcinoma of the breast is a special type of invasive ductal carcinoma of the breast that is rare in clinical practice. Neoadjuvant therapy, especially neoadjuvant targeted therapy, has rarely been reported for apocrine carcinoma of the breast.CASE SUMMARY A 63-year-old woman presented with apocrine carcinoma of the left breast underwent core needle biopsy. The patient was diagnosed with apocrine carcinoma by immunohistochemical staining and negative hormone status(estrogen receptor and progesterone receptor) but showed overexpression of human epidermal factor receptor 2 (HER-2). Moreover, positive expression of androgen receptor (approximately 60%) and gross cystic disease fluid protein 15 was observed. The patient was treated with neoadjuvant targeted therapy consisting of the TCH regimen (docetaxel, carboplatin area under curve 6 and trastuzumab) every 21 d. The mass in the left breast was significantly reduced,and pain in the breast and left upper arm also improved.CONCLUSION HER-2 positive apocrine carcinoma of the breast can be improved by neoadjuvant chemotherapy combined with targeted therapy.
Key Words: Breast neoplasm; ErbB-2 receptor; Targeted therapy; Case report; Apocrine gland; Neoadjuvant therapies
INTRODUCTION
Breast cancer is the most common malignant tumor in women worldwide and has become a major threat to women's health[1]. Invasive ductal carcinoma of no-specialtype is the most common type of breast cancer and constitutes up to 75% of all breast carcinomas. The remaining 25% are special histologic types including invasive apocrine carcinoma of the breast, which accounts for 0.4%-4.0% of all breast cancers in women[2-4]. Apocrine carcinoma of the breast is a rare invasive malignant tumor that is mainly composed of apocrine cells, which is defined by the World Health Organization as an invasive carcinoma with cytological features of apocrine cells[5].More strictly, it is characterized by abundant eosinophilic and granular cytoplasm,centrally/eccentrically located nuclei with prominent nucleoli and distinct cell borders, and a distinct steroid receptor profile: Hormone receptor (HR)-negative and androgen receptor (AR)-positive cells[6]. “pure” apocrine carcinoma is defined by apocrine morphology in > 90% of tumor cells and immunohistochemical criteria, and it appears to have a worse disease-free survival rate[3]. So far, the precise significance of AR expression is not completely clear. Niet al[7]showed that androgen stimulated the human epidermal factor receptor 2 (HER2) signaling pathway in estrogen receptor(ER)-negative and HER2-positive breast cancer, and AR blockade in these tumors impaired cell growth. Naderiet al[8]reported similar observations and demonstrated a functional “cross-talk” between androgen and HER2. Unfortunately, it is rarely used clinically at present. Anti-HER2 therapy is still the cornerstone for HR-negative and HER2-positive apocrine carcinoma of the breast. Neoadjuvant therapy is preferred for locally advanced breast cancer, especially HR-negative and HER2-amplified breast cancer. However, there are few reports on the efficacy of neoadjuvant targeted therapy for apocrine carcinoma. Informed content was obtained from the patient.
CASE PRESENTATION
Chief complaints
A 63-year-old woman found a mass in the superior lateral quadrant of the left breast,with no obvious discomfort, and she paid no attention to it.
History of present illness
During the next 2 years, the left breast mass gradually increased in size and was painful. She developed discomfort in the left upper limb and visited a local hospital many times (without an examination report). Surgical treatment was suggested, but the patient refused.
History of past illness
The patient had a free previous medical history.
Personal and family history
The patient has a history of good health, and there is no similar patient in the family members.
Physical examination
Physical examination showed that the skin in the outer upper quadrant of the left mammary gland was obviously sunken, and a hard mass about 5 cm × 6 cm, with an unclear boundary, irregular shape, and poor activity was found on palpation. No obvious enlarged lymph nodes were found in the axilla.
Laboratory examinations
No abnormalities were found in the patient's laboratory examinations.
Imaging examinations
Ultrasound showed a solid hypoechoic mass approximately 3.5 cm × 5.3 cm × 4.5 cm in size at the margin of the gland at 12-3 o'clock in the superior lateral quadrant of the left breast, and several hypoechoic lymph nodes of different sizes were detected in the left axilla. The largest lymph node was about 0.6 cm × 0.6 cm, and the lymphatic hilum structure had disappeared. No abnormalities were found in the right breast. Therefore,chest computed tomography (CT) scanning was performed, and the left breast mass was diagnosed as breast cancer, with no abnormalities in the lungs. Other results,including abdominal ultrasound, bone scan, and laboratory examinations, showed no abnormalities. There was no family history in genetic disorders.
Further diagnostic work-up
The patient underwent core needle biopsy of the left breast mass under ultrasound guidance, and the histopathological diagnosis was apocrine carcinoma.Immunohistochemical analysis showed negative expression of ER and progesterone receptor (PR), but positive expression of HER2 and AR (approximately 60%); gross cystic disease fluid protein 15 (GCDFP-15) was also positive (Figure 1).
FINAL DIAGNOSIS
The final diagnosis of the presented case is apocrine carcinoma of the breast. The clinical stage was T4N1M0 (IIIB).
TREATMENT
Considering that the patient had small breast volume, large breast lesion, late clinical stage, and local advanced breast cancer and her molecular type, neoadjuvant therapy seemed an effective choice. Therefore, after informed consent was obtained from her family members and the patient, neoadjuvant chemotherapy using the TCH regimen[docetaxel, carboplatin area under curve 6 and trastuzumab 8 mg/kg followed by 6 mg/kg every 21 d] and targeted therapy were administered. No significant side effects were observed during the treatment.
OUTCOME AND FOLLOW-UP
After 5 cycles of treatment, the left breast lesion was significantly reduced on CT examination (Figure 2). In November 2019, the patient underwent modified radical mastectomy. During the operation, mild edema and thickening of the left breast skin,unclear boundary of the breast lesions, and irregular morphology were observed, and no capsule or obvious calcified lesions were found in the specimen. The specimen was soaked in formalin solution and sent to the pathology department. Apocrine carcinoma of the breast was confirmed by pathology. The immunohistochemical results were as previously determined, but Ki-67 was reduced to 50%.
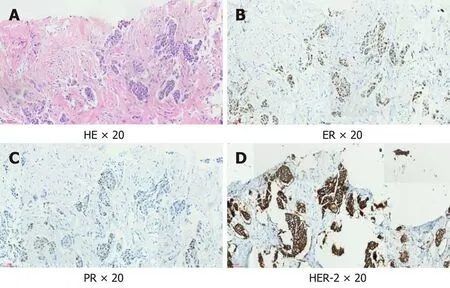
Figure 1 Immunohistochemical examination of the left breast mass. A: Hematoxylin-eosin staining, 20 ×; B: Estrogen receptor, 20 ×; C: Progesterone receptor, 20 ×; D: Human epidermal factor receptor 2, 20 ×. HE: Hematoxylin-eosin; ER: Estrogen receptor; PR: Progesterone receptor; HER2: Human epidermal factor receptor 2.
DISCUSSION
Apocrine carcinoma of the breast remains largely unknown as studies have recruited a small number of patients and did not use well-defined criteria for apocrine carcinoma.“Molecular apocrine” carcinomas exhibit a prognostically poor gene signature with a high-risk recurrence score and a poor 70-gene prognosis signature[9]. Zhanget al[10]analyzed data from the SEER Program and suggested that compared with other invasive carcinomas, overall survival and disease-specific survival (DSS) were both worse in invasive apocrine adenocarcinoma patients than in invasive ductal carcinoma patients. Based on the Kaplan-Meier analysis, the prognosis of apocrine carcinoma is poor. Further study on the risk factors influencing the overall survival and diseasespecific survival by multifactor analysis confirmed that histological grade II/III, tumor size > 2 cm, and positive lymph nodes were associated with poor prognosis and that ER/PR positive breast conserving surgery, and radiotherapy were protective factors in DSS[10]. Nevertheless, Japazeet al[11]suggested that “pure” invasive apocrine carcinoma may be a distinct clinicopathological entity with less aggressive behavior than highgrade no-special-type cancer. In addition, Wuet al[12]identified 366 patients with triplenegative apocrine carcinoma of the breast and 30996 patients with triple-negative breast cancer and invasive ductal carcinoma from the SEER database. Patients with triple-negative apocrine carcinoma had a better prognosis than patients with triplenegative breast cancer, and chemotherapy was associated with survival advantages in patients with triple-negative apocrine carcinoma.
There are some contradictions in the prognostic study of apocrine carcinoma of the breast, which may be related to its unclear definition. In addition, the latest classification of breast tumors by the World Health Organization is equally inaccurate[13].At present, most experts agree that the definition of pure apocrine carcinoma should be based on typical cell morphology and unique immunohistochemical characteristics[14,15], as this profile matches closely the normal apocrine epithelium. Our patient was characterized by typical morphological manifestations and immune combinations.
Mammary apocrine cells have abundant eosinophilic and granular cytoplasm,centrally to eccentrically located nuclei with prominent nucleoli and distinctive cell borders, or less common apocrine cells with a foamy and vacuolated cytoplasm[16]. AR activation and signaling is a hallmark of apocrine differentiation in breast pathology;moreover, AR has been associated with HER2 signaling in apocrine carcinoma[17].HER2 protein is overexpressed in approximately 15% of all breast carcinomas[18], but the rate of HER2 overexpression is approximately 50% in apocrine carcinoma[19].GCDFP-15, identified by Haagensenet al[20]in 1977, is a 15-kDa protein mapped to chromosome 7, and its expression has been associated with apocrine differentiation,including apocrine carcinoma, although its positivity has been confirmed in other breast carcinoma subtypes[20-22]. GCDFP-15 positive patients are associated with local recurrence and distant metastases[23].
At present, clinical and radiological presentations of apocrine carcinoma do not differ from those seen in invasive ductal carcinomas[24]. Clinically, apocrine carcinoma usually presents with a palpable tumor mass, rarely with a bloody discharge from the nipple or as a cyst[25,26]. However, some studies have indicated a higher rate of apocrine carcinoma (and AR expression) in the elderly[26].
With regard to treatment, some studies have indicated a poor response to chemotherapy in patients with apocrine carcinoma[27], although HER2 enriched breast carcinomas tend to have the highest rate of complete response to neoadjuvant chemotherapy. Iizukaet al[28]described a case of triple-negative apocrine carcinoma treated with docetaxel/cyclophosphamide (four courses) and epirubicin/cyclophosphamide (four courses), with a complete pathologic response to neo-adjuvant chemotherapy. However, neoadjuvant targeted therapy for apocrine carcinoma of breast has rarely been reported. The breast mass in our patient was initially up to 5.3 cm in diameter and was locally advanced; thus, she received the neoadjuvant TCH regimen and then underwent surgery after five cycles of treatment, which resulted in partial remission. Therefore, we believe that HER2 positive apocrine carcinoma of the breast can be treated with neoadjuvant targeted therapy.
CONCLUSION
As a rare invasive carcinoma, there is no special treatment at present for apocrine carcinoma of the breast. Appropriate treatment can be given based on immunohistochemical results. For HER2 positive locally advanced apocrine carcinomas of the breast, according to our experience, neoadjuvant targeted therapy is appropriate and can yield desirable results. The predictive role of AR expression and the efficacy of anti-AR therapy in the treatment of breast cancer have not been determined. More clinical evidence is needed.
ACKNOWLEDGEMENTS
The authors thank the patient for agreeing to publish this report.
杂志排行
World Journal of Clinical Cases的其它文章
- Understanding the immunopathogenesis of COVID-19: Its implication for therapeutic strategy
- What is the gut feeling telling us about physical activity in colorectal carcinogenesis?
- Latest developments in chronic intestinal pseudo-obstruction
- Correlation between ductus venosus spectrum and right ventricular diastolic function in isolated single-umbilical-artery foetus and normal foetus in third trimester
- Clinical efficacy of integral theory–guided laparoscopic integral pelvic floor/ligament repair in the treatment of internal rectal prolapse in females
- Treatment of Kümmell’s disease with sequential infusion of bone cement: A retrospective study
