New treatment of patellar instability after total knee arthroplasty: A case report and review of literature
2020-04-07XianYueShenJianLinZuoJianPengGaoTongLiuJianLinXiaoYanGuoQin
Xian-Yue Shen, Jian-Lin Zuo, Jian-Peng Gao, Tong Liu, Jian-Lin Xiao, Yan-Guo Qin
Xian-Yue Shen, Jian-Lin Zuo, Jian-Peng Gao, Tong Liu, Jian-Lin Xiao, Department of Orthopedics,China-Japan Union Hospital of Jilin University, Changchun 130033, Jilin Province, China
Xian-Yue Shen, Yan-Guo Qin, Department of Orthopedics, The Second Hospital of Jilin University, Changchun 130041, Jilin Province, China
Abstract BACKGROUND Patellar instability is an uncommon complication after total knee arthroplasty(TKA). Partial lateral patella facetectomy (LPF) with lateral retinaculum release treatment of patellar instability is rarely reported.CASE SUMMARY We present a case of patellar instability 8 mo after primary TKA. Treatment of this complication was adapted to address the cause of the dislocation. To eliminate patellar instability, we restored the vastus medialis and performed LPF with lateral retinaculum release. We achieved normal patellar tracking. Clinical and radiographic evaluations at the 1-year postoperative follow-up were satisfactory.CONCLUSION LPF with lateral retinaculum release represents a promising option to restore central patellar tracking in patients with patellar instability after TKA in cases without component malposition.
Key Words: Total knee arthroplasty; Patellar instability; Lateral patella facetectomy;Complication; Case report
INTRODUCTION
Total knee arthroplasty (TKA) is an effective surgical procedure; however, a range of complications can occur. Patellar instability is a serious complication of TKA that may require revision surgery[1-3]. Patients with patellar instability after TKA present with anterior knee pain, giving-way, and functional limitation. Risk factors for patellar instability after TKA include surgical technique, prosthetic causes, and soft-tissue imbalance[4]. Management of patellar instability after TKA requires surgery[2,5-8].Implant revision is required when patellar instability is related to prosthetic malposition. For soft-tissue imbalance, reconstruction of the medial patellofemoral ligament with lateral retinaculum release represents an effective treatment option.
Reports describing management of patellar instability after TKA using partial lateral patella facetectomy (LPF) with lateral retinaculum release has not been previously reported. Here, we present a case of patellar instability after TKA due to rupture of the vastus medialis that was treated by vastus medialis restoration and partial LPF with lateral retinaculum release. To our knowledge, this is first published report of patellar instability after TKA treated with LPF with lateral retinaculum release.
CASE PRESENTATION
Chief complaints
An 84-year-old female experienced severe anterior right knee pain 8 mo after TKA. In January 2018, the patient was referred to our department for therapy.
History of present illness
The patient was diagnosed with bilateral knee osteoarthritis and underwent right primary TKA in November 2016. Physical examination prior to primary TKA revealed a decrease in range of motion to 15°-50°. Figure 1 shows preoperative anteroposterior and lateral radiographs of the right knee and full-length weight-bearing radiographs of the lower extremities. The patient underwent posterior stabilized TKA with patellar denervation using the medial parapatellar approach. After implantation, functional patellar tracking was assessed by the surgeon (Prof. JLZ) using the “no thumb technique”. Lateral release was not performed. Range of motion and isometric quadriceps exercises were initiated immediately, and weight-bearing was allowed on postoperative day 1. Postoperatively, range of motion improved to 0°-120°. Eight months after surgery, the patient experienced severe anterior right knee pain.
History of past illness
The patient had medical history of hypertension (American Society of Anesthesiologists physical status classification II due to hypertension).
Physical examination
Physical examination revealed patellar instability of the right knee, especially when the knee was in the flexion position, and that quadriceps strength was obviously lower in the right knee compared to the left. Clinical examination showed a limited range of motion.

Figure 1 Primary total knee arthroplasty. A: Preoperative radiographs, anteroposterior view; B and C: Lateral views; and D: Full length weight-bearing of the lower extremities.
Imaging examinations
Radiographs did not demonstrate any obvious fractures or prosthetic malposition.Weight-bearing full length X-rays of the lower extremity demonstrated a well-restored mechanical axis. Skyline view revealed a lateral shift of the patella (Figure 2).
FINAL DIAGNOSIS
As there were no structural imbalances or weakness in the injured knee, we diagnosed lateral patellar dislocation after TKA due to soft-tissue imbalance.
TREATMENT
We intended to stabilize the patella by medial patellofemoral ligament (MPFL)reconstruction combined with lateral retinaculum release. Exposure occurred through the same incision used for primary TKA, and the patella was everted and displaced laterally. During surgery, we found rupture of the vastus medialis, damage to the patella articular cartilage, and osteophyte formation in the lateral patella (Figure 3). In addition, the patella was small and thin and not suitable for patellar resurfacing.Therefore, we tentatively adopted a more targeted surgical method. We restored the vastus medialis, partially resected the lateral patella, and released the lateral retinaculum. Functional patellar tracking was confirmed throughout the range of motion. The operation took about 40 min.
OUTCOME AND FOLLOW-UP
This case shows that LPF with release of lateral retinaculum is effective in the treatment of patellar dislocation after TKA. The patient underwent clinical (Hospital for Special Surgery Clinical Score) and radiographic (anteroposterior, lateral, and skyline views) evaluation during 1-year of follow-up with no complaints of knee pain or subluxation. At the 1-year of follow-up, the patient was able to walk with a crutch,had active range of motion was 0°-110°, and had the Hospital for Special Surgery Clinical Score of 85.

Figure 2 Primary total knee arthroplasty. A: Postoperative radiographs of the right knee, anteroposterior view; B: Lateral view; and C: Skyline view.

Figure 3 Reoperation. A: An intraoperative view of the ruptured vastus medialis; B: Partial lateral facetectomy.
DISCUSSION
TKA is a well-established procedure that is effective for the treatment of advanced knee joint arthritis. Management of the patellofemoral joint in TKA remains controversial but has an important impact on outcomes[9]. Inappropriate management of the patellofemoral joint may lead to a series of complications. Risk factors for patellofemoral joint instability in TKA include component positioning and limb alignment, component design, patellar preparation, and soft-tissue balancing[1].
To our knowledge, we are the first to report on the use of LPF with lateral retinaculum release for the treatment of patellar instability after TKA. In the present case, the patient had a small thin patella; therefore, she had undergone primary TKA with denervation instead of patella resurfacing, which may have led to patellar fracture[10]. Postoperatively, the femoral and tibial components were aligned and stable and tracking of the patella was normal[11-14]. After 8 mo, the patient experienced severe anterior right knee pain. We diagnosed lateral patellar dislocation. We speculated that nonresurfacing of the patella and soft-tissue imbalance contributed to patellofemoral instability in this patient. Seoet al[15]reported no significant clinical and radiological differences in patients with resurfacedvsnonresurfaced patellae; however, several meta-analyses have revealed a higher risk for reoperation in patients with nonresurfaced patellae[9,16-18]. The patient underwent primary TKA by a medial parapatellar approach, which may have damaged the vastus medialis, resulting in soft-tissue imbalance.
MPFL reconstruction and distal realignment of the patella represents an effective treatment option for patellar instability after TKA[2,8,19-21]. Carmontet al[22]and Gotoet al[21]achieved good results using MPFL for patellar dislocation due to rupture of the medial structures after TKA. Similarly, Nakajimaet al[8]reported satisfactory outcomes after adopting an Elmslie-Trillat procedure in combination with extensive lateral release to treat patellar instability after primary TKA in cases without component malposition (Table 1).
In this patient, we tentatively adopted a novel surgical approach to stabilize effectively the patella. We reconstructed the vastus medialis and performed partial LPF in combination with lateral retinaculum release. Patella facetectomy was first introduced by O’Donoghue[23]; subsequently, partial LPF was reported as an effective treatment for patellofemoral osteoarthritis, especially for alleviating anterior knee pain[24-29]. However, clinical evidence supporting the use of this method in the treatment of patellar instability after TKA is lacking. A number of studies showed that lateral retinaculum release is beneficial for correcting patellar maltracking[2,30-33]. The present case provides clinical evidence supporting the use of partial LPF in combination with lateral retinaculum release for the treatment of patellar instability after TKA.
CONCLUSION
In conclusion, to the authors’ knowledge, this report is the first to describe successful treatment of patellar instability after TKA by LPF with lateral retinaculum release. This procedure represents a promising option to restore central patellar tracking in patients with patellar instability after TKA.
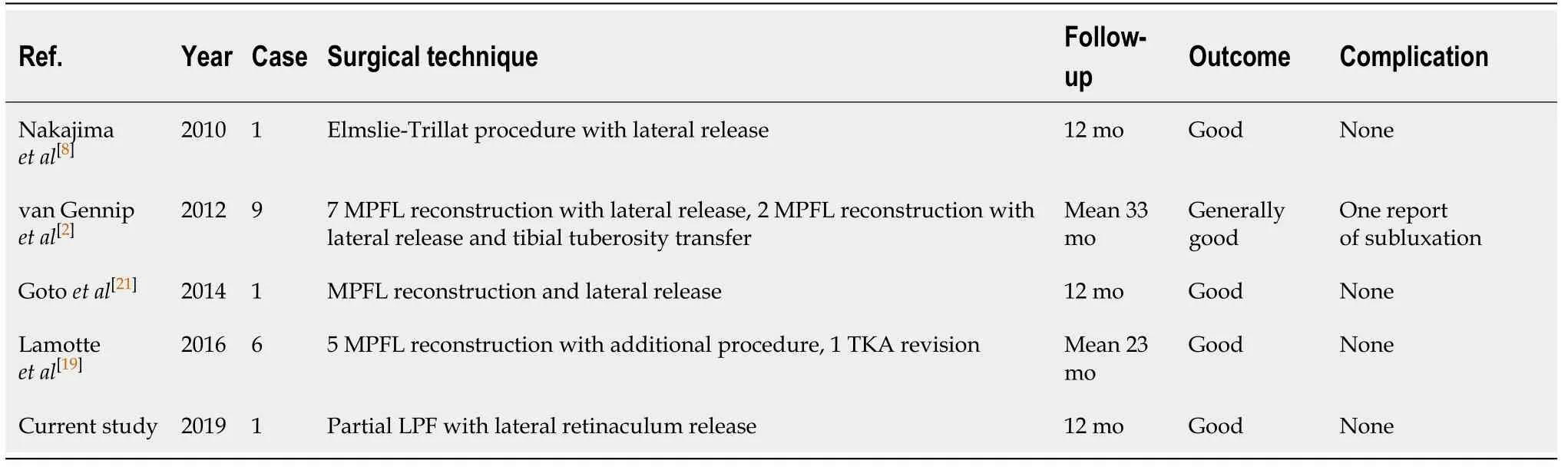
Table 1 Published literature describing treatment for patellar instability after total knee arthroplasty
杂志排行
World Journal of Clinical Cases的其它文章
- Erratum: Author’s Affiliation Correction. Type II human epidermal growth factor receptor heterogeneity is a poor prognosticator for type II human epidermal growth factor receptor positive gastric cancer (World J Clin Cases 2019; Aug 6; 7 (15): 1964-1977)
- Potential protection of indocyanine green on parathyroid gland function during near-infrared laparoscopic-assisted thyroidectomy:A case report and literature review
- Benign symmetric lipomatosis (Madelung’s disease) with concomitant incarcerated femoral hernia: A case report
- Fanconi-Bickel syndrome in an infant with cytomegalovirus infection: A case report and review of the literature
- Incomplete Kawasaki disease complicated with acute abdomen: A case report
- Chinese patient with cerebrotendinous xanthomatosis confirmed by genetic testing: A case report and literature review