Nafamostat mesylate-induced hyperkalemia in critically ill patients with COVID-19: Four case reports
2020-04-07MasakiOkajimaYoshinoriTakahashiTakaakiKajiNaohikoOgawaHideyukiMouri
Masaki Okajima, Yoshinori Takahashi, Takaaki Kaji, Naohiko Ogawa, Hideyuki Mouri
Masaki Okajima, Hideyuki Mouri, Intensive Care Unit, Kanazawa University Hospital, Kanazawa 920-8641, Ishikawa, Japan
Yoshinori Takahashi, Department of Rheumatology, Kanazawa University Hospital, Kanazawa 920-8641, Ishikawa, Japan
Takaaki Kaji, Department of Nephrology, Kanazawa University Hospital, Kanazawa 920-8641,Ishikawa, Japan
Naohiko Ogawa, Department of Respiratory Medicine, Kanazawa University Hospital,Kanazawa 920-8641, Ishikawa, Japan
Abstract BACKGROUND Nafamostat mesylate (NM) may prove to be one of the key drugs effective against coronavirus disease 2019 (COVID-19) because of its anti-viral properties and the potential to manage coagulopathy. However, NM tends to increase serum potassium levels.CASE SUMMARY We observed hyperkalemia immediately after NM administration (200 mg/d) in four consecutive patients who were admitted to the Kanazawa University Hospital with severe COVID-19 pneumonia. Urinary potassium excretion decreased after NM administration in three patients who underwent urinalysis.CONCLUSION NM is likely to produce hyperkalemia in patients with COVID-19. Therefore, it is necessary to monitor serum potassium values closely after NM initiation in COVID-19 patients who need respiratory support.
Key Words: COVID-19; Nafamostat; Hyperkalemia; Disseminated intravascular coagulation; Respiratory insufficiency; Case report
INTRODUCTION
The pathophysiology of coronavirus disease 2019 (COVID-19) is still unclear; however,coagulopathy, an important mechanism of severe respiratory failure, has been observed in many severe COVID-19 cases and is associated with high mortality[1].Therefore, managing coagulopathy is an important therapeutic target in severe COVID-19 cases.
Nafamostat mesylate (NM) is a serine protease inhibitor that inhibits proteolytic enzymes, such as thrombin, plasmin, and trypsin, and has been used for several decades in Japan for disseminated intravascular coagulation (DIC) and pancreatitis treatment.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has been reported to enter epithelial cellsviatransmembrane protease serine 2 (TMPRSS2), which is inhibited by NM[2]. Additionally, coagulopathy in COVID-19 is characterized by enhanced fibrinolysis, which is treatable with NM[3]. Therefore, NM is anticipated to be a key drug against COVID-19.
However, NM has several side effects, with the most frequently observed side effect being hyperkalemia. We observed hyperkalemia immediately after NM administration in four consecutive patients who were admitted to the Kanazawa University Hospital between April 15 and April 27, 2020 with severe COVID-19 pneumonia and were treated with NM 200 mg/d for intravascular coagulopathy.
CASE PRESENTATION
Chief complaints
Patient 1 suffered from fever, dyspnea and diarrhea. Patient 2 had cough and sore throat. Patient 3 gradually developed cough, loss of appetite and malaise. Patient 4 suffered from fever, cough, sore throat, dyspnea and diarrhea.
History of present illness
As described above.
History of past illness
Patient 2 had hypertension and patient 4 had diabetes mellitus. Others had no history of past illness.
Personal and family history
As described above.
Physical examination
Not applicable.
Laboratory examinations
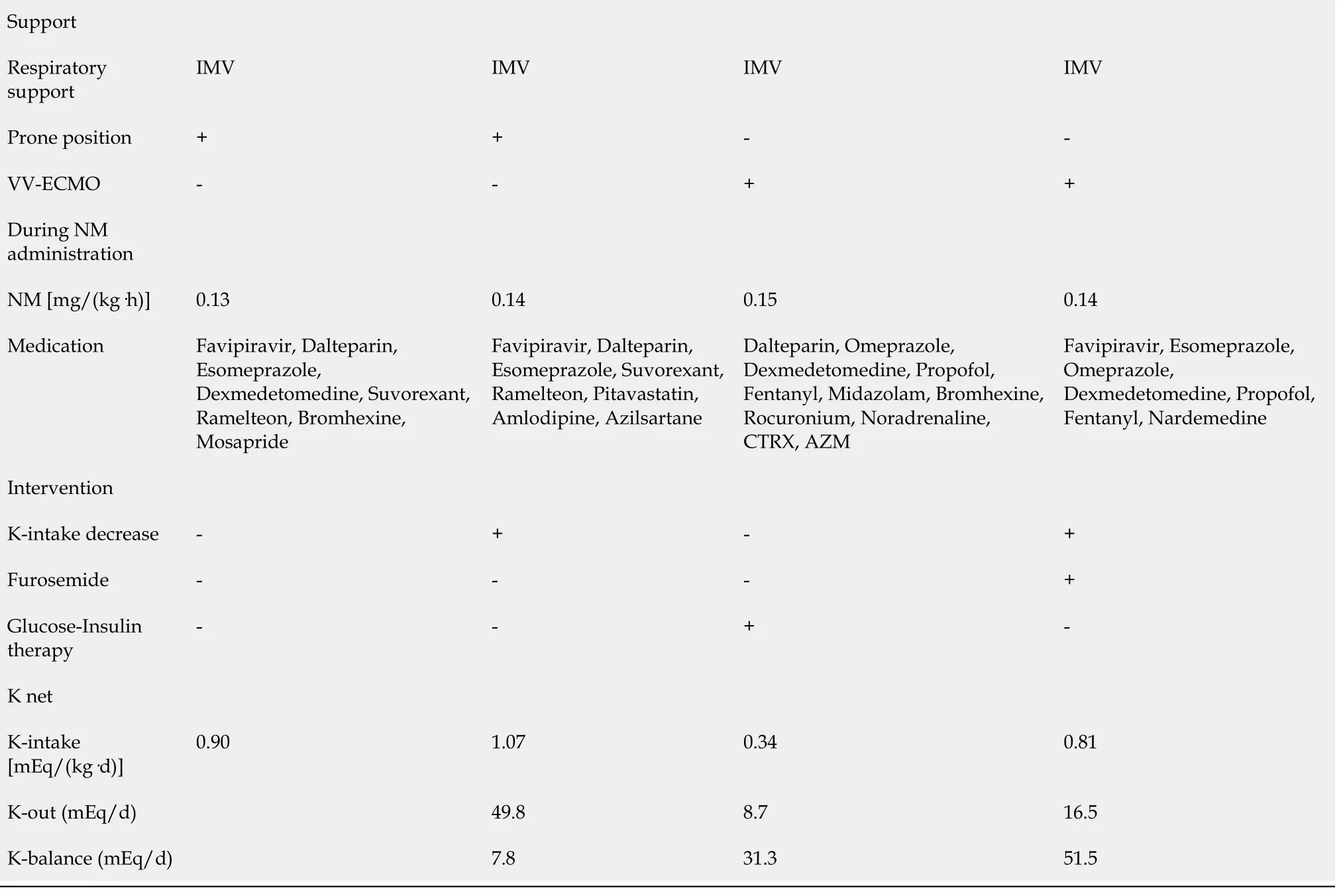
Their characteristics before NM administration are shown in Table 1. Levels of fibrin degradation products, fibrin degradation product D-dimer, and fibrinogen were elevated in all the patients. All required invasive mechanical ventilation, while twopatients additionally required veno-venous extracorporeal membrane oxygenation after several days. No patient had chronic kidney disease and diarrhea; one patient was administered an angiotensin II receptor blocker, which is a potent drug that increases serum potassium levels. All four patients developed hyperkalemia (> 6 mEq/L in two patients) immediately after NM administration, without any acute kidney injuries (Figure 1). Three patients underwent urinalysis, and the urinary potassium levels were found to be relatively low; their potassium balance was positive, considering serum potassium levels were high in all of them. In the fourth patient, the transtubular potassium gradient was examined and found to be low (< 6).
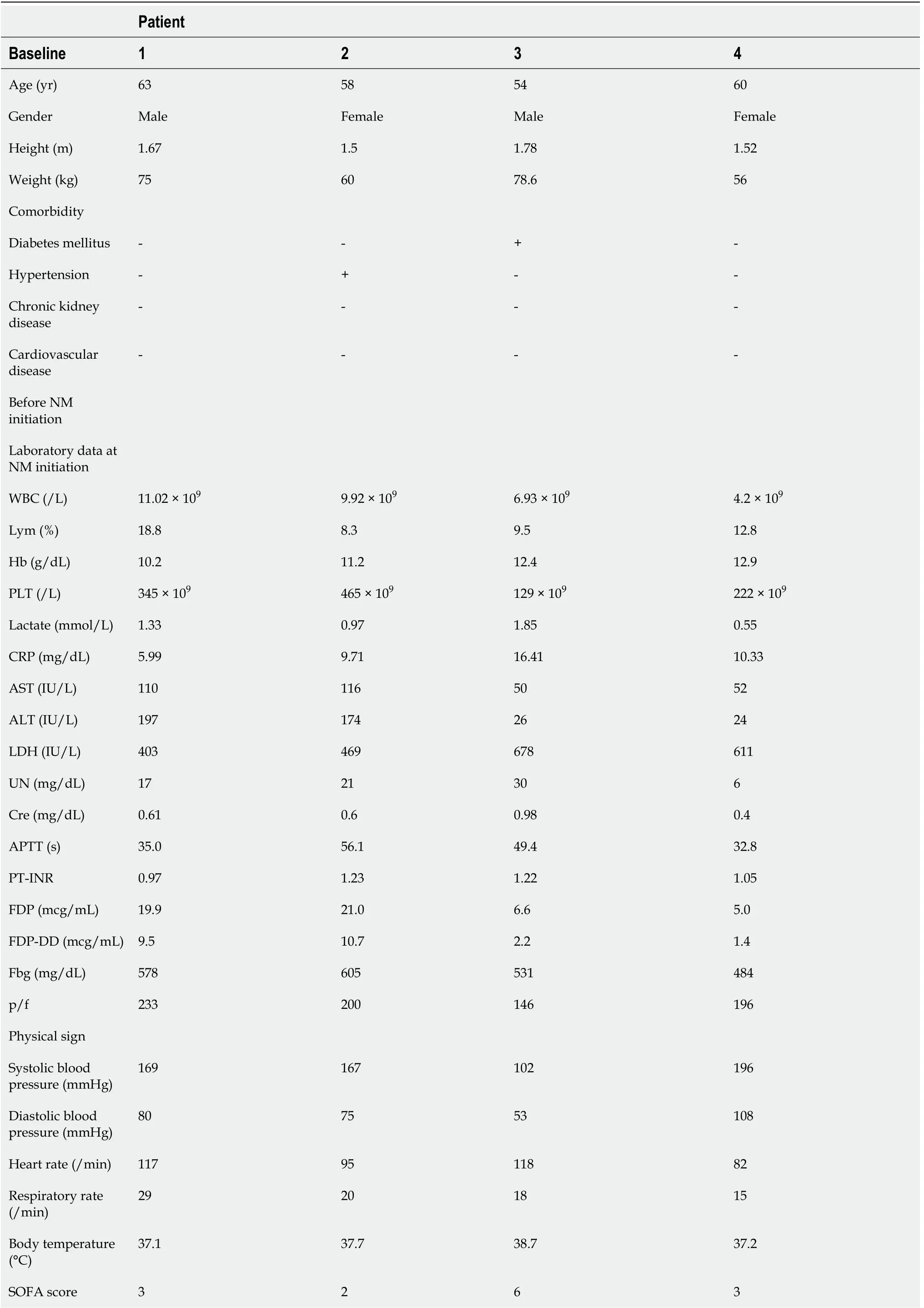
Table 1 Characteristics at baseline, before and during nafamostat mesylate administration
WBC: White blood cell; Lym: Lymphocytes; Hb: Hemoglobin; PLT: Platelet; CRP: C-reactive protein; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; LDH: Lactate dehydrogenase; UN: Urea nitrogen; Cre: Creatinine; APTT: Activated partial thromboplastin time; PT-INR: Prothrombin time and normalized ratio; FDP: Fibrin degradation products; FDP-DD: Fibrin degradation product D-dimer; Fbg: Fibrinogen; p/f: PaO2/FiO2; SOFA:Sequential organ failure assessment; VV-ECMO: Veno-venous extracorporeal membrane oxygenation; NM: Nafamostat mesylate; K: Potassium.
Imaging examinations
Not applicable.
FINAL DIAGNOSIS
All four patients were diagnosed with NM-induced hyperkalemia.
TREATMENT
As indicated in Table 1, all patients required antihyperkalemic therapy including potassium intake reduction, furosemide administration, and glucose-insulin therapy.
OUTCOME AND FOLLOW-UP
Serum potassium levels were normalized after administration of NM was stopped in all patients.
Figure 1 Changes in serum potassium and creatinine levels before and during nafamostat mesylate administration. Serum potassium levels increased in all four patients on the third day of NM administration without acute kidney disease. A: Serum potassium; B: Serum creatinine. Cre: Creatinine; NM:Nafamostat mesylate; K: Potassium.
DISCUSSION
NM may be suitable against COVID-19 infection as it can effectively block the SARSCoV-2 entryviainhibition of TMPRSS2, and possesses antifibrinolytic qualities that may treat intravascular coagulation with enhanced fibrinolysis observed in COVID-19 patients. However, NM tends to increase serum potassium levels. Generally, NM causes hyperkalemia in 0.19% of patients with pancreatitis and in 4.75% with DIC. The required dose of NM is higher for DIC patients [0.06-0.20 mg/(kg·h)] than pancreatitis patients (10-20 mg/d)[4]. Our four patients received NM at a dose of 0.13-0.16 mg/(kg·h), which is equivalent to the dose used for DIC. However, we observed hyperkalemia immediately after NM administration in all four patients, which is a higher rate than has been previously reported.
NM and its metabolites have been reported to cause hyperkalemia by inhibiting aldosterone, Na-K ATPase activity in urinary tubules, and amiloride-sensitive sodium conductance in the cortical collecting duct, resulting in the reduction of urinary potassium excretion[5]. Our findings also indicate a decrease in urinary potassium excretion after NM administration. SARS-CoV-2 has been reported to be excreted in the urine and exists in the urinary tubules of patients with severe COVID-19[6].Therefore, SARS-CoV-2 could enhance NM-induced hyperkalemia by inhibiting Na-K ATPase activity or amiloride-sensitive sodium conductance, especially in patients with severe COVID-19 who need respiratory support.
CONCLUSION
This is the first report to suggest that NM is likely to produce hyperkalemia in patients with COVID-19. Therefore, we need to monitor serum potassium values closely after NM initiation in COVID-19 patients.
ACKNOWLEDGEMENTS
We would like for the following collaborating author names from COVSAT-KUH(Special Assistant Team against COVID-19 at the Kanazawa University Hospital)Study Group to be searchable through their individual PubMed records: Endo I,Takashima S, Okada H, Oishi M, Yoshio T and Takago S.
杂志排行
World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system