Strategies and challenges in the treatment of chronic venous leg ulcers
2020-04-07ShiYanRenYongShengLiuGuoJianZhuMengLiuShaoHuiShiXiaoDongRenYaGuangHaoRongDingGao
Shi-Yan Ren, Yong-Sheng Liu, Guo-Jian Zhu, Meng Liu, Shao-Hui Shi, Xiao-Dong Ren, Ya-Guang Hao, Rong-Ding Gao
Shi-Yan Ren, Department of General Surgery and Vascular Surgery, Aviation General Hospital,China Medical University, Beijing 100012, China
Yong-Sheng Liu, Department of Dermatology, Aviation General Hospital, Beijing 100012,China
Guo-Jian Zhu, Department of General Surgery, Taian Communications Hospital, Taian 271000,Shandong Province, China
Meng Liu, Department of Surgery, Tianjin Hexi Hospital, Tianjin 300202, Tianjin, China
Shao-Hui Shi, Department of Orthopaedic Surgery, Aviation General Hospital, China Medical University, Beijing 100012, China
Xiao-Dong Ren, Department of Surgery, Wanquanqu Zhongyi Hospital, Zhangjiakou 076250,Hebei Province, China
Ya-Guang Hao, Department of Medical Administrative, Aviation General Hospital, China Medical University, Beijing 100012, China
Rong-Ding Gao, Department of General Surgery, Aviation General Hospital, China Medical University, Beijing 100012, China
Abstract Evaluating patients with chronic venous leg ulcers (CVLUs) is essential to find the underlying etiology. The basic tenets in managing CVLUs are to remove the etiological causes, to address systemic and metabolic conditions, to examine the ulcers and artery pulses, and to control wound infection with debridement and eliminating excessive pressure on the wound. The first-line treatments of CVLUs remain wound care, debridement, bed rest with leg elevation, and compression.Evidence to support the efficacy of silver-based dressings in healing CVLUs is unavailable. Hydrogen peroxide is harmful to the growth of granulation tissue in the wound. Surgery options include a high ligation with or without stripping or ablation of the GSVs depending on venous reflux or insufficiency. Yet, not all CVLUs are candidates for surgical treatment because of comorbidities. When standard care of wound for 4 wk failed to heal CVLUs effectively, use of advanced wound care should be considered based on the available evidence.Negative pressure wound therapy facilitates granulation tissue development,thereby helping closure of CVLUs. Autologous split-thickness skin grafting is still the gold standard approach to close huge CVLUs. Hair punch graft appears to have a better result than traditional hairless punch graft for CVLUs. Application of adipose tissue or placenta-derived mesenchymal stem cells is a promising therapy for wound healing. Autologous platelet-rich plasma provides an alternative strategy for surgery for safe and natural healing of the ulcer. The confirmative efficacy of current advanced ulcer therapies needs more robust evidence.
Key Words: Chronic venous leg ulcers; Debridement; Compression; Negative pressure wound therapy; Autologous split-thickness skin grafting; Hair punch graft; Platelet-rich plasma; Advanced wound care therapies
INTRODUCTION
Leg ulcer refers to areas of epidermal discontinuity in lower limbs with causes of venous, arterial, diabetic, pressure, traumatic, allergic, or inflammation (Figure 1).Chronic venous leg ulcers (CVLUs) are defined as leg ulcers persisting for 4 wk or more due to chronic venous insufficiency[1,2]and account for up to 70% of all chronic leg ulcers. CVLUs have an overall prevalence of up to 2% in the general population of western countries with significant morbidity and a negative socioeconomic impact[3-6].
CVLUs are susceptible to microbial invasion and can cause serious complications,such as delayed healing, cellulitis, increasing ulcer size, debilitating pain, and deeper wound infections causing systemic illness[7]. It is critical to assess and manage patients with effective approaches. Yet, there are some controversies on the treatment of patients with CVLUs; therefore, we review in this article the most recent literature on the management of patients with CVLUs to provide valuable and practical information for clinical workers.
TENETS IN THE TREATMENT OF CVLUS

Figure 1 Patient received minimally invasive surgery for varicose veins, the small incision was closed by adhesive strap on November 4,2019. A: An allergic blister was found on postprocedure day 4; B: The skin was peeled while removing the strap; C: The wound was unhealed on November 12, 2019 as the patient failed to follow-up on schedule for wound care.
A systematic assessment of patient and CVLUs is essential to find the underlying etiology. The basic principles in managing CVLUs are to remove the etiological causes,to evaluate the wound and artery pulses, and to manage systemic conditions and wound infection with debridement, and to reduce excessive pressure on the wound.The first-line treatments of CVLUs are bed rest with leg elevation, wound care,debridement, and compression. Surgical approaches remain a high ligation with or without stripping or ablation of the great saphenous veins (GSVs) depending on venous reflux or insufficiency; not all CVLUs are suitable for surgery due to comorbidities[1,2,8]. Standard wound care should be used for an initial period of 4 wk and can fail to heal approximately 25% of CVLUs. Even advanced therapies do not heal > 60%. Wound failing to heal 50% ulcer area at 4 wk should be reevaluated and then considered for advanced therapies in the absence of underlying disease[3-6]. When standard care of wound for 4 wk failed to heal CVLUs effectively, advanced wound care should be considered to use based on the available evidence. Unfortunately, many advanced approaches for CVLUs do not have strong evidence or a randomized prospective study to evaluate the efficacy.
ASSESSMENT OF THE PATIENTS AND WOUNDS
Most CVLUs are not an isolated disorder but the manifestation of underlying conditions, such as hypertension, diabetes, and peripheral vascular conditions. History of comorbidities should be carefully consulted to make a confirmed diagnosis[3].

Figure 2 This 70-year-old female patient had suffered from chronic venous leg ulcers on both lower extremities for 40 years. Thirty years ago, a skin graft was harvested from her thigh without any anesthesia expecting for better survival of the graft. Unfortunately, the skin graft failed to grow, and she refused any skin harvest for skin graft. At this current time, her wound was prepared well enough for skin graft. A: Chronic venous leg ulcers on both lower extremities; B: Prepared for skin graft.
On consulting with a patient, the location, size, and number of ulcers, the color of the exudates, offensive odor from the wound exudates if any, and arterial pulses in the limbs should be examined initially. The survival ability and the extent of skin around the ulcer should be judged, and a photograph should be taken with a ruler adjacent to the ulcers. The offensive odor or increasing pain in a chronic wound usually indicates the presence of ulcer infection(Figure 2).A swab swept from the wound bed is usually cultured to guide the further selection of antibiotics against infection, a negative culture guarantees no bacterial infection in the wound due to the skill of sampling, the process of a sample, or test techniques. A biopsy should be considered for any patients with a history of atypical chronic refractory ulcers to exclude skin cancer (e.g.,squamous cell carcinoma)[9](Figure 3). X-ray film may demonstrate if there is an involvement of the bone or inflammation of tissue underneath or around the ulcers(Figure 4). Patients with leg edema, healed or active ulcers, especially with a history of deep venous thrombosis (DVT), should be examined with duplex ultrasound for iliocaval venous obstruction. Loss of respiratory variation in the common femoral vein or reversed flow in the superficial epigastric vein on duplex ultrasound should be referred for ascending venogram (Figure 5) or computed tomography (CT) to assess the venous insufficiency or valve failure[10-12]. In patients with complicated CLUVs, CT angiography for artery in limbs to confirm the presence and degree of arterial occlusion is a wise choice.
DEBRIDEMENT
Microbial biofilms in the wound cause non-healing and infection due to their increased resistance to antibiotics. The microbial-host environment and the pathophysiology of venous hypertension in the lower extremities demand a multimodality approach for closing CVLUs. In addition to systemic and topical antibiotics, wound bandages, compression therapy, and wound debridement and restoring blood supply to the wound help sustain the infection and healing the wound[7].
The types of debridement include mechanical debridement, autolytic debridement,and enzymatic debridement[13]. Surgical debridement is performed for extensive devitalized or necrotic tissue, severe infection of skin or cellulitis, infected bone or sepsis that causes the risk of poor wound healing,osteomyelitis,generalized infection,and sepsis. Frequent mechanical debridement of a chronic ulcer is essential to reduce the necrotic burden and achieve healthy granulation[14]. The edge of the granulation tissue looks white and should be preserved instead of being removed (Figure 6),especially in patients with diabetes and peripheral vascular disease.
DRESSINGS

Figure 3 The patient had chronic venous leg ulcers for approximately 20 years. The pathological study of a biopsy from the wound indicated squamous cell carcinoma.
A variety of dressings for the management of CVLUs include hydrocolloids,hydrogels, alginates, foam, and antimicrobial dressing[15]. Foam dressings containing hydrophilic foam can be used for exuding CVLUs. Alginate dressing is suitable for wound with a cavity or complicated ulcers; when it contacts with exudates, a gel will be formed to facilitate wound rehydration[16]. Hydrogel dressing consists of crosslinked insoluble polymers and is easier to remove than alginate dressing and is suitable for dry wounds[17]. Unfortunately, no robust evidence is available to favor one dressing over another for CVLUs[18,19]. It is worthwhile to remind that selection of wound dressings is sometimes influenced by advertisement instead of evidence[20,21].
A common concern for ulcers is pain on changing dressings or at night that can be relieved with pain killer. Preclinical data support a role for dextrose prolotherapy in promoting tissue repair that is required for healing chronic wounds and ameliorating the associated pain. Five percent dextrose can cause the production of growth factors that have critical roles in repair[4]. Furthermore, numerous clinical trials report proreparative effects of dextrose prolotherapy in joint diseases, tendon and ligament damage, and painful musculoskeletal issues[4].
COMPRESSION BANDAGING OR STOCKINGS
An adequate arterial supply must be ensured initially before compression therapy. A graduated compression bandage (two to four layers) or stocking is the most effective management of CVLUs and should be started as early as possible to relieve the symptoms of venous insufficiency. Stockings are more welcomed than bandages because of their uniform pressure on the skin, comfort, and cosmetic reasons. The patients should be warned to prevent a band or rope-like structure in the edge of the bandage or stockings around the leg to avoid unnecessary injury to the skin. The patients should be educated to walk and elevate the legs if possible. CVLUs heal faster with compression than without[20,21].
TOPICAL-USE PRODUCTS
The topical use of cadexomer iodine is recommended for CVLUs. The comprehensive use of silver-containing dressings is not substantiated by scientific evidence. The primary use of silver-containing products is to reduce bacterial infection, but no data are available to favor the effect of wound closure[22]. The results of a randomized controlled trial (RCT) demonstrated that a microorganism-binding dressing is more effective than a silver-containing hydrofiber dressing in controlling the bacterial loads of infected CVLUs in terms of bacterial reduction rate (73.1%vs41.6%,P< 0.00001)[23].Besides, the role of povidone-iodine, peroxide-containing products for healing CVLUs cannot be concluded until an additional qualified study is performed[22].

Figure 4 The male patient had varicose vein and venous insufficiency for 15 years and ulcers for 1.5 years. A: Redness, warmth, pain, and edema with two ulcers were noticed on admission; B: The inflation of the skin was relived after initial treatment; C and D: X-ray showed calcification of the tissue around ulcers.
Hydrogen peroxide (H2O2) is an endogenous reactive oxygen species that contributes to oxidative stress directly as a molecular oxidant and indirectly through the free radical generation. It is commonly used to irrigate wounds because of its hemostatic and antiseptic properties. However, H2O2should be used with caution due to its oxidant adverse effects. Low H2O2concentrations cause only transient symptoms(blanching and blistering), but exposure to 9%-45% H2O2can cause more severe skin damage, including epidermal necrosis, leading to erythema and bullae, toxicity to keratinocytes and fibroblasts, oxygen embolism demonstrated intracranial air trapping in the right frontal lobe, and multiple cerebral infarction foci in postoperative computed tomography[24,25].
PHARMACOTHERAPY AND ANTIBIOTICS
Micronized purified flavonoid fraction (MPFF), pentoxifylline, and sulfoxide are reported to improve CVLU healing and recommended as an effective adjunct to compression therapy for CVLUs[26,27]. MPFF counteracts the pathophysiologic mechanism of venous insufficiency and is the only venoactive drug to control the inflammatory reaction induced by venous hypertension[26-28].
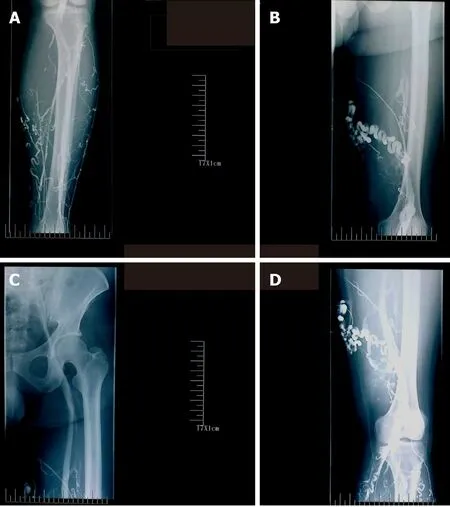
Figure 5 Ascending venogram shows the varicosities at lower leg and thigh, patency of femoral and iliac veins, and the degree of reflux while performing venography. A: Lower leg; B and D: Thigh; C: Femoral and iliac veins.

Figure 6 The edge of the ulcer appears white, a sign for the development of granulation tissue. This tissue should be preserved rather removed during debridement.
Systemic antibiotics can only be used for patients with evidence of clinical infection rather than bacterial colonization; it is not recommended to use antibiotics locally in ulcers[22]. One study reported that oral administration of low doses of doxycycline 20 mg twice daily for 3 mo could improve extracellular matrix functioning, and its immunomodulating and anti-inflammatory actions through the inhibition of matrix metalloproteinase provided a possible solution to support wound healing[6]. Another study[29]compared 10 patients who received doxycycline 20 mg twice daily with another 10 patients who received doxycycline 100 mg twice daily; the results indicated that higher dosage may improve the healing rate of recalcitrant leg ulcers[29]. A casecontrol study showed that topical 0.5% timolol maleate improves the healing of chronic leg ulcers[30].
HONEY AND MALTODEXTRIN/ASCORBIC ACID
Honey has been used as a traditional medicine for centuries by different cultures for the treatment of wounds. However, not all honey exhibits equal antimicrobial potency,and only a few meet the criteria for clinical usage. A prospective cohort study and a case series study support the use of honey[31,32]; the average wound area of 25 patients with CVLUs decreased significantly following the use of honey.Overall,72%(18/25)patients experienced a decrease in reported pain levels, and 80% patients were satisfied with honey treatment[32]. One trial (108 participants) showed that 44% (24/54)ulcers were closed with honeyvs33% (18/54) with hydrogel (P= 0.037); another trial supported the use of honey over hydrogel in healing ulcers (P< 0.001)[19]. However,three RCTs that evaluated healing CVLUs with honeyvsstandard wound therapy arrived at contradictory conclusions. One showed better outcomes, one showed equivalent outcomes but more adverse effects, and the third showed a non-significant reduction in bacterial colonization. Overall, the clinical bottom line is that there is no conclusive evidence that honey improves outcome in patients with CVLUs; its benefit should be considered unproven until more robust trials results are available[31].
It is hypothesized that maltodextrin or ascorbic acid treatment could stimulate tissue repair of chronic wounds by changing the stage of inflammation and modifying collagen turnover directly through fibroblast response. Patients with CVLUs treated with maltodextrin and ascorbic acid were found to have decreased microorganism population and improved wound repair, with almost four-fold CVLUs closure during 12 wk in comparison with those treated with zinc oxide[33]. Nevertheless, the clinical effects of this treatment need to be approved with further clinical trials.
OXYGEN THERAPY
Hyperbaric oxygen therapy has been successfully used for patients with hypoxic diabetic ulcers and CVLUs[34,35]and has demonstrated no significant risk of cell damage caused by a high concentration of oxygen[34].A retrospective study of 200 patients with chronic wounds treated with hyperbaric oxygen showed that their wounds were healed or reduced (62.0%) compared to those with acute wounds[35,36]. Topical oxygen therapy can stimulate chronic wounds to heal. After oxygen therapy for over 25 d, 83%wound area reduction and 47% wound closure were observed in CVLUs patients[36].
SURGERY
Marstonet al[37]reported that patients with CVLUs treated with saphenous stripping had less ulcer recurrence (15%) than those treated with compression therapy (34%); no statistical significance in ulcer healing between compression plus surgery (ligation and stripping) group and compression alone group (82%vs76%) was observed. Most patients with varicose veins and leg ulcers are treated with endovenous thermal ablation (EVTA), and ulcers recurred in a minority of CVLUs patients after EVTA.Patients with varicose veins who have no deep venous reflux and undertake both phlebectomy and EVTA have experienced less ulcer recurrence. Thus, it is suggested to perform both phlebectomy and EVTA for patients with varicose veins and CVLUs if possible[37].
Treatment of superficial venous reflux has been shown to reduce the rate of ulcer recurrence[1,2,38]. Endovenous laser ablation of superficial venous reflux early resulted in faster closure of CVLUs and more time free from ulcers than deferred endovenous ablation[1,39]. Patients with CEAP 5 venous ulcers healed faster with EVLT and compression therapy than with compression alone[40]. Although the ablation of the GSV appears to help reduce ulcer recurrence, there was no impact of combined superficial and perforator ablations on ulcer recurrence rates. The role of incompetent perforating veins ablation alone or concomitant with GSV treatment needs further RCT study to be performed[39].
Correction of both superficial truncal vein reflux and deep vein stenosis contributes to the healing of CVLUs[1,2,38]. Patients with iliofemoral DVT have a high chance to develop post-thrombotic syndrome. Patients who fail to heal their CVLUs after superficial and perforator ablation should examine the iliocaval system to find hemodynamically significant stenoses or occlusions amenable to stenting[41]. Iliac vein stenting can significantly help improve clinical outcomes in patients with venous stenosis or obstruction. Venous duplex ultrasound in diagnosing iliac vein stenosis with 2.5 s can predict ≥ 50% iliac vein stenosis. Stent placement and pentoxifylline were associated with ulcer healing and reduced risk of venous ulcer recurrence[42]. The endovascular iliocaval and infrainguinal venous stenting help to improve clinical symptoms, improve 1-year patency rate, and heal recalcitrant venous ulcers. Clinical outcomes in patients with IVC filters were improved significantly after removing the filter compared to those in which the filter could not be removed (100%vs17%;P<0.01)[11,12].
SKIN GRAFTING
Skin grafting helps expedite the closure of CVLUs. Currently available grafts are taken from the patient's normal skin, preserved animal’s skin, human cadaveric dermis,porcine dermal, or a sheet of bioengineered skin grown from donor cells. Most grafts have an acellular collagen scaffold, providing room for neovascularization or tissue incorporation[43]. A porcine dermal matrix (Permacol) was reported to be used successfully for a woman with a complex and infected abdominal wall defect wound.One year after discharge, the patient was pain-free with complete wound healing[43].
Currently, autologous split-thickness skin grafting (STSG) is still the first choice to treat huge CVLUs or diabetic ulcers[44]and has greater success rates in CVLUs than in other types of wounds[45,46]. A study assessed the effectiveness of skin autografting at 6 mo after grafting[47], and large CVLUs (> 50 cm2) in 67.5% elderly patients (> 60 years) were closed within 2-3 wk by skin grafting, compared to the conservative group, and maintained closure up to 6 mo[47].
In a retrospective, descriptive study of outpatients with CVLUs, diabetic foot ulcers,surgical, or traumatic wounds were treated with a meshed, partial-thickness,cryopreserved human skin allograft. The results favored the use of allograft skin for chronic wounds[48].
Double layer dermal substitute is composed of a superficial silicon layer and a three-dimensional collagen structure and can be placed within the ulcers to boost tissue regeneration. Nevelia®is a new collagen dermal template substitute to treat chronic venous or arterial ulcers and facilitates tissue formation and angiogenesis[49,50].Furthermore, 11 trials comparing a variety of grafts with standard care concluded that bilayer artificial skin, used in conjunction with compression bandaging, increases venous ulcer healing compared with a simple dressing plus compression. Further research is needed to assess whether other forms of skin grafts increase ulcer healing[51].
HAIR FOLLICLE SCALP GRAFTS
The hair follicle is a large reservoir of progenitor cells; the hair bulge in a hair follicle has epithelial and melanocytic stem cells that can produce the interfollicular epidermis, hair follicle structures, and sebaceous glands and reconstitute in an artificialin vivosystem to a new hair follicle[52,53]. The isolated bulge epithelial stem cells can increase the hair density in patients with androgenetic alopecia[54]. Gentileet al[52,55]performed a placebo-controlled, randomized, evaluator-blinded, half-head group study that showed that hair regrowth with micrografts containing hair follicle mesenchymal stem cells may represent a safe and viable treatment alternative against hair loss.
Hair follicle-derived cells play a role as a wound-healing promoter in epidermal wound closure. Hair punch grafting is a minimally invasive surgical procedure for CVLUs[56,57]. An RCT with an intraindividual comparison of hair follicle scalp grafts and hairless skin grafts transplanted in parallel into two halves of the same ulcer was performed. Autologous transplantation of terminal hair follicles by scalp punch grafts led to better healing than hairless punch grafts. The average percentage reduction of ulcer area at 18 wk post-grafting was significantly higher in the hair follicle graft group than in the hairless grafts (75.15 %vs33.07%,P= 0.002). Hair punch graft appeared to have a better result than traditional hairless punch graft for CVLUs;epithelialization, neovascularization, and dermal reorganization were improved histologically[53,57,58].
NEGATIVE PRESSURE WOUND THERAPY
The viability of new skin grafting in chronic ulcers is a major concern due to bacterial infection, chronic inflammation, tissue edema, and low oxygen in CVLUs. Negative pressure wound therapy (NPWT) has been used to manage a variety of wounds by granulation tissue formation, wound drainage, and preparation for delayed ulcer closures or grafting. It facilitates the sustaining and incorporation of skin grafts or flaps onto the recipient wound bed[59-62].A combination of NPWT with irrigation of oxygen loaded fluid can raise the partial pressure of oxygen of the skin around the wounds effectively, enhance the transition of macrophages from type I to type II, and may promote the growth of granulation tissue, leading to a better recipient for skin grafting or epithelization[63].
However, an RCT study of 46 patients comparing NPWT with hydrocolloid dressings over 5 d following autologous grafting on CVLUs failed to show the benefit of NPWT associated with skin graft over traditional dressings. This could be due to the limited number of cases enrolled[64].
NPWT with topical wound solution instillation (NPWTi) helps with wound preparation prior to STSG. NPWTi in a porcine model showed improved tissue oxygenation, granulation tissue, and clearance of wound debris. NPWT after STSG promoted graft catch through reducing shear forces, fluid acquisition, and neovascularization. STSG for massive CVLUs is better than standard compression therapy in terms of less pain, early time to walk, less outpatient visits, and times of dressings required and ulcer healing rate[59-62,65-67]. In a study including 10 patients with CVLUS, the average length of time ulcers was 38 mo (3-120 mo) on admission, and 10 patients received inpatient NPWT with NPWTi for 7d, then STSG with NPWT over the graft for 4 d. Overall, eight patients experienced complete CVLU closure by 6 mo after NPWTi with STSG[62].
MESENCHYMAL STEM CELLS
Mesenchymal stem cells (MSCs) are multipotent progenitor cells that are capable of directly differentiating into various mesenchymal cell lineages and facilitate wound healing by regulating immune response and inflammationin vivo. The sources of MSC include autogenous, such as bone marrow or adipose tissue-derived stem cells, and allogeneic (e.g., placenta-derived stem cells). MSCs are immune-privileged due to lacking cell surface antigens. MSCs have been used clinically and are reported as a promising and compelling therapy for CVLUs[68].
Placental tissues, including the chorion, the umbilical cord, the amnion, and the amnionic fluid, are full of MSCs, are readily available, and have no ethical concerns for embryonic stem cells[69]. Placental-derived MSCs possess paracrine, metabolic, and immunomodulatory properties while keeping the immune-privileged status[69].Placental or amniotic membranes (AMs) prepared from fresh cesarean section donors were used for wound healing were used. AMs were initially used for corneal ulcers for many years[69-71].
Placental tissue is beneficial in healing chronic wounds[45]. AMs are available in the cryopreserved state or as dehydrated human amnion/chorion membrane (dHACM)allograft for direct implantation[72-74]. Overcoming the difficulties of fresh transplantation, some cryopreserved AM products are commercially available in a micronized formulation to be used topically or hydrated for injection into wounds or other inflamed tissues to shorten wound closure time[75,76]. Further studies should be undertaken to determine if there is a distinction between different amniotic matrices regarding efficacy in wound repair[77].
ADIPOSE-DERIVED MSCS
Adipose-derived MSCs (ADSCs) as well as bone marrow MSCs are the most widely studied cell types[78,79]and display similar results in terms of tissue growth[80].Adiposederived stromal vascular fraction (AD-SVFs) and ADSCs warrant careful preparation of the harvested adipose tissue. Gentileet al[80,81]described the procedures to isolate and prepare the ADSCs and platelet-rich plasma as well as the application of ADSCs in practice.
ADSC strategy provides a great opportunity for the treatment of chronic wounds not responding to the standard treatment. ADSCs are easy to obtain due to lower morbidity during the harvesting procedure[78,80], can be implanted at the wound site immediately following debridement, and promote a new tissue formation rich in vascular structures and remodeling collagen[82]. As an additional treatment to primary surgical therapy for CVLUs[83], one study showed that it does not shorten the venous recovery period but decreases the 1-year recurrence rate[83]. However, preclinical and observational RCT reports indicate that centrifuged adipose tissue containing progenitor cells is safe and may accelerate healing time in CVLUs and reduce wound pain[84].ADSCs enriched, high-density lipoaspirate (HDL) with topical timolol was used for the healing of CVLUs. A 63-year-old patient with CVLUs and venous stasis for 30 years underwent stripping of varicose veins, the standard of care, and anticoagulation. ADSCs-enriched, HDL on wound matrix and compression therapy was used for her medial ulcer, and, as a control, compression therapy following debridement was applied for the lateral ulcer. Daily topical timolol was used for both ulcers for 1 mo. After 3 mo, the medial ulcer was closed completely and maintained healed for over 15 mo. In contrast, healing signs of lateral ulcers in the leg were minimal[85].
The stromal vascular fraction (SVF) of adipose tissue consists of cellular subpopulations with distinct regenerative potential. A prospective clinical pilot study showed that SVF cells could be used safely for the treatment of CVLUs and mixed arterial-venous ulcers even in multimorbid patients, but one-time application of the used amounts of SVF cells was not sufficient in the majority of cases with larger predominantly ischemic mixed arterial-venous ulcers and comorbidities[86,87].
AUTOLOGOUS PLATELET-RICH PLASMA AND GROWTH FACTOR
Autologous platelet-rich plasma (PRP) containing fibrin and growth factors can stimulate tissue regeneration with the potential to enhance the healing of chronic wounds. PRP is easily accessible, is relatively inexpensive and safe, and can be injected into or dressed topically over the ulcers. It is an alternative to surgery for a safe and natural healing ulcer[78,80,88,89].
Gentileet al[88]in Italy described the meticulous preparation approach for PRP.Cervelliet al[90]reported that post-traumatic leg ulcers treated with enhanced SVF and PRP combined with fat grafting healed better than those treated with hyaluronic acid(HA). De Angeliset al[91]reported that PRP plus HA treatment showed stronger regenerative potential in terms of epidermal proliferation and dermal renewal than with HA alone. A total of 182 patients with chronic ulcers (diabetic and vascular)treated with PRP plus HA within 80 d showed stronger re-epithelialization than another 182 patients in the control group treated with HA alone (98.4%, 1.3%vs87.8%,4.1%,P< 0.05)[91]. Two RCTs results showed PRP injection enhances the healing of CVLUs more than PRP application and compression therapy in terms of healing rate,healing time, and ulcer area reduction[92,93].
The overall quality of evidence of PRP for treating chronic ulcers remains low. PRP may boost the healing of diabetic foot ulcers, but this conclusion is based on low quality evidence from two small RCTs. Well designed and adequately powered clinical trials are needed to show convincingly the efficacy of autologous PRP in the healing of CVLUs and other chronic wounds[94-96].
The efficacy of recombinant granulocyte-macrophage colony-stimulating factor in the treatment of CVLUs remains insignificant clinically[97]. An open-label, prospective,multicenter RCT shows that human fibroblast-derived dermal substitute and compression therapy have no benefit over compression therapy alone in terms of healing time, healing rate, and adverse effects for CVLUs[98].
DEHYDRATED HUMAN AMNION/CHORION MEMBRANE ALLOGRAFT
An RCT compared dHACM allograft with multilayer compression only for CVLUs. Of 47 patients without complete healing during the initial study, wound size of ≥ 40%decreased in 20 (45.4%) patients; < 40% ulcer area decreased in 24 (55%) patients. All 47 patients were treated with dHACM allograft for a mean of 46 d. Eighty percent(16/20) patients in the ≥ 40% group had ulcer closure (P= 0.0027), and 33.3% (8/24)patients in the < 40% group experienced ulcer closure at a mean of 103.6 d (P=0.0023)[72]. Besides, dHACM allograft can be used as an adjunct to immunosuppressive therapy to reduce pain and heal the pyoderma gangrenosum ulcer in a patient with multiple comorbidities, including venous insufficiency and diabetes mellitus[73].
An RCT studied patients with nonhealing full-thickness CVLUs, and the ulcers treated weekly with dHACM allograft healed more significantly than those with standard wound care and compression (60%vs35% at 12 wk,P= 0.0128; 71%vs44%at 16 wk,P= 0.0065)[74]. Another RCT study enrolled 84 participants, and venous leg ulcers (n= 53) treated with allograft for 4 wk had significant healing compared with multilayer compression therapy alone (n= 31) (48.1%vs19.0%)[99]. A retrospective study showed that the average time to healing leg ulcers with dHACM grafts was less than that with conservative treatment (33 dvs87 d)[100].Another two retrospective cohort studies showed all wounds (venous, diabetic foot ulcers) were closed effectively after the use of dHACM allograft[101,102].
CRYOPRESERVED HUMAN PLACENTAL MEMBRANE GRAFTS
Viable cryopreserved human placental membrane (vCHPM) is an effective therapy for CVLUs refractory to standard of care. Adjunctive therapy with human viable wound matrix (hVWM) provides superior healing rates in refractory CVLUs[45]. A retrospective review describes patients with chronic wounds that had failed standard of care treatments for more than 4 wk and were subsequently treated with weekly use of vCHPM grafts. All ulcers reached full closure in 4-5 wk with no complication[103].After using hVWM of cryopreserved placental tissue, 53% (16/30) of CVLUs refractory to standard therapy healed completely. CVLUs were reduced in size by half more with hVWM than standard therapy (80%vs25%,P< 0.001). The mean rate of reduction in ulcer area was more significant after hVWM than with standard therapy (1.69% per dayvs0.73% per day,P= 0.01)[104].
CONCLUSION
Wound care, debridement, bed rest with leg elevation, and compression are basic approaches for CVLUs. Ablation of the GSVs can help to heal some ulcers. Negative pressure wound therapy is very helpful for the preparation of ulcers and promotes the growth of granulation tissue. Split-thickness skin grafting is the first choice for the management of huge CVLUs. Hair punch graft appears to have a better result than that with traditional hairless punch graft for CVLUs. Administration of adipose tissue or placenta-derived MSCs is a promising therapy for wound healing. Autologous platelet-rich plasma provides an alternative strategy for surgery for a safe and natural healing of the ulcer. There are little data to support the efficacy of silver-based dressings in the healing of CVLUs. Hydrogen peroxide is harmful to the growth of granulation tissue in CVLUs. The confirmative efficacy of current advanced ulcer therapies needs more robust evidence.
杂志排行
World Journal of Clinical Cases的其它文章
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system
- Accuracy of endoscopic ultrasound-guided needle aspiration specimens for molecular diagnosis of non-small-cell lung carcinoma