Magnetic resonance imaging findings of carcinoma arising from anal fistula: A retrospective study in a single institution
2020-04-07XinZhuTianShuZhuDanDanYeShaoWeiLiu
Xin Zhu, Tian-Shu Zhu, Dan-Dan Ye, Shao-Wei Liu
Xin Zhu, Department of Radiology, The Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing 210029, Jiangsu Province, China
Tian-Shu Zhu, The First Clinical Medical College, Xuzhou Medical University, Xuzhou 221004,Jiangsu Province, China
Dan-Dan Ye, Department of Radiology, Quanzhou Orthopedic-Traumatological Hospital,Quanzhou 362000, Fujian Province, China
Shao-Wei Liu, Department of Radiology, Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing 210029, Jiangsu Province, China
Abstract BACKGROUND Magnetic resonance imaging (MRI) is currently the standard investigation for suspected perianal diseases. Carcinoma arising from anal fistula is very rare, and early diagnosis is often difficult.AIM To describe and summarize the MRI findings of carcinoma arising from anal fistula.METHODS In this retrospective study, records of ten patients diagnosed with carcinoma arising from anal fistula and confirmed by surgery (n = 7) or biopsy (n = 3)between June 2006 and August 2018 were analyzed. All patients underwent preoperative pelvic MRI. Morphologic features, signal characteristics, fistula between the mass and the anus, contrast enhancement of mass, signal and enhancement of peritumoral areas, and regional lymphadenopathy were assessed.RESULTS All ten tumors were solitary (8 mucinous adenocarcinomas and 2 adenocarcinomas). The maximum diameter of the tumors ranged from 3.4 cm to 12.4 cm (median: 4.15 cm; mean: 5.68 cm). Eight patients had a fistula between the mass and the anus. Contrast enhancement of the peritumoral areas was noted in three (3/5) patients. Perirectal or inguinal lymphadenopathy was noted in seven patients. Most lesions of mucinous adenocarcinoma were multiloculated and cauliflower-like, with a thin capsule and focally unclear boundary. They were markedly hyperintense on fat-suppressed T2WI, slightly hyperintense with focal hyperintensity on diffusion-weighted imaging (DWI), and hyperintense with focal hypointensity on apparent diffusion coefficient (ADC) map, with progressive mesh-like contrast enhancement. Adenocarcinomas had an infiltrative margin without a capsule and appeared heterogeneously hyperintense or slightly hyperintense on fat-suppressed T2WI, hyperintense on DWI, and hypointense on ADC map, with persistent heterogeneous enhancement.CONCLUSION Our study highlighted several characteristic and potentially helpful MRI findings to diagnose carcinomas arising from anal fistula.
Key Words: Anal fistula; Carcinoma; Magnetic resonance imaging; Morphologic features;Signal characteristics; Differential diagnosis
INTRODUCTION
Anal carcinomas are rare malignant tumors, accounting for approximately 2%-3% of large-bowel malignancies[1]. A carcinoma arising from an anal fistula is even rarer, and early diagnosis is often difficult[2,3]. The early symptoms of these tumors are similar to common perianal diseases; therefore, they are often wrongly diagnosed as benign lesions. Owing to the delay in diagnosis, patients typically have advanced-stage disease at the time of surgery[4]. Diagnostic confirmation of cancer arising from an anal fistula is through histopathological examination.
Magnetic resonance imaging (MRI) is considered the most accurate preoperative technique for classification of anal fistula and is useful for evaluation of the primary track, abscesses, and extensions to adjacent tissues[5-7]. More importantly, it is useful to guide clinicians in determining the extent of surgical resection. Diffusion-weighted imaging (DWI) is already being incorporated into anal cancer MRI protocol as a result of its many clinical advantages[7,8]. Although carcinomas arising from anal fistula have been reported from the perspectives of their clinical features, only few studies have focused on their MRI findings[9-11]. The purpose of this study was to describe the MRI findings in patients with carcinomas arising from anal fistula, and explore more characteristic signs to facilitate the auxiliary diagnosis of this disease.
MATERIALS AND METHODS
Patients
This retrospective study was approved by the institutional review board of the Affiliated Hospital of Nanjing University of Chinese Medicine, which waived the requirement for informed consent. Between June 2006 and August 2018, ten patients diagnosed with carcinoma arising from anal fistula underwent preoperative pelvic MRI.Age,sex,pathological subtypes,clinical symptoms,duration of anal fistula,and history of surgery were recorded (Table 1). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and national research committees and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Magnetic resonance imaging technique
MRI was performed either on a 1.5-T system (Aera, Siemens AG, Munich, Germany) (n= 9) or 3.0-T system (Verio, Siemens AG, Munich, Germany) (n= 1). Unenhanced MRI of the pelvis was performed in all the ten patients. In five patients, this was followed by dynamic contrast enhanced (DCE) scans. In the remaining five, this was followed by diffusion-weighted imaging (DWI). All patients were examined using a pelvic phased-array coil. The imaging technique used for pelvic MRI at our institution is provided in Table 2.
Diagnostic criteria and pathologic examination
Carcinoma arising from anal fistula was diagnosed according to Rosser’s criteria: (1)The fistula should usually antedate the carcinoma by at least 10 years; (2) The only tumor present in the rectum or anal canal should be secondary to direct extension from the carcinoma in the fistula; and (3) The internal opening of the fistula should be into the anal canal and not into the tumor itself[12].
Pathological specimens were observed by light microscopy and immunohistochemical analysis. All tumors were confirmed to be carcinomas arising from anal fistula by surgery (n= 7) or biopsy (n= 3). Cases of rectal cancer, malignant signs in the anal mucosa, and the internal opening of fistula into the tumor were excluded before definite diagnosis.
Image analysis
Pelvis MRI images were reviewed and interpreted in consensus by two radiologists with 5 and 20 years of experience, respectively, who were blinded to the histopathologic results. Morphologic features (location, shape, maximum diameter,capsule, and margin); signal characteristics [fat-suppressed T2-weighted MRI (FST2WI), DWI, and apparent diffusion coefficient (ADC)]; fistula between the mass and anus; contrast enhancement of mass; signal on FS-T2WI and enhancement of peritumoral areas; and regional lymphadenopathy were assessed on MRI. These features were selected based on the previous literature and our personal experience[9-11].
The capsule was observed as a hypointense area on both T1-weighted magnetic resonance imaging (T1WI) and T2WI. Signal intensity on FS-T2WI was classified as markedly hyperintense, hyperintense, and slightly hyperintense. Marked hyperintensity was defined as signal intensity similar to that of fluid in the bladder.Hyperintensity was defined as signal intensity higher than that of muscle but lower than that of fluid. Slight hyperintensity was defined as signal intensity slightly higher than that of muscle. Fistula between the mass and the anus was defined as a tubular or linear hyperintense communication between the mass and the anus assessed on FST2WI.
The enhancement pattern of tumor was assessed on T1-DCE images. We observed the enhancement characteristics of the tumor including the inner edge of the lesion(smooth or rough), enhancement of septum, and unenhanced necrotic area within the lesion. Contrast enhancement of peritumoral areas was also assessed on T1-DCE images. If there was enhancement around the tumor, the signal intensity of this area was observed on FS-T2WI.
Regional lymphadenopathy was defined as perirectal and inguinal lymph nodes > 5 mm in the short axis, morphological change (irregular or round), signal intensity on FS-T2WI, heterogeneous enhancement, or hyperintensity on DWI[13].
RESULTS
The mean age at diagnosis of the ten patients (eight mean and two women) was 59 ±12 years (age range: 31-75 years; median, 60 years). Most patients (90%) were older than 50 years. Eight patients were diagnosed with mucinous adenocarcinoma and two with adenocarcinoma. Clinical symptoms included persistent fistula in ten patients,pain in five, anal discharge in five, gradually enlarging mass in one, and hematochezia in one. One patient was diagnosed with Crohn’s perianal fistula-associated mucinous adenocarcinoma. Nine patients had long-lasting anal fistulas with durations ranging from 2 to 40 years; six of these patients had anal fistulas lasting more than 10 years.Nine patients had a history of prior surgery (Table 1). Table 3 summarizes the MRI findings of carcinoma arising from anal fistula.
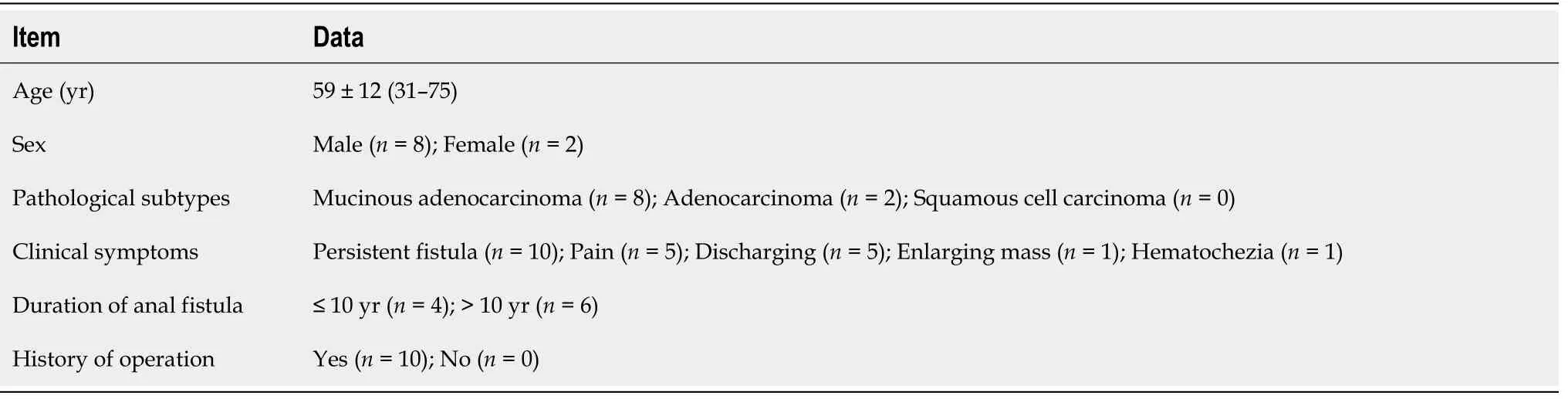
Table 1 Patient demographics and symptoms
Location of tumor:Six lesions were on the left, two on the right, and two grew across the midline (Figure 1).
Shape and maximum diameter of lesions:The lesions were multiloculated and cauliflower-like (n= 6), round or oval (n= 3), and band-like (n= 1) in shape. The maximum diameter of the tumors ranged from 3.4 to 12.4 cm (median: 4.15 cm; mean:5.68 cm) on FS-T2WI.
Margin and capsule:Seven lesions with mucinous adenocarcinoma had a thin capsule, unlike the thick fibrous capsule of a fistula, and the focal boundary of tumors was unclear (Figures 1 and 3). The remaining three lesions (one mucinous adenocarcinoma and two adenocarcinomas) had an infiltrative margin without capsule (Figure 2).
Signal on FS-T2WI, diffusion-weighted imaging, and apparent diffusion coefficient map:Among the eight patients with mucinous adenocarcinoma, six showed markedly hyperintense, one showed hyperintense, and one showed slightly hyperintense signal on FS-T2WI images (Figures 1 and 3). In two patients with adenocarcinoma, tumors appeared as heterogeneously hyperintense or slightly hyperintense signals (Figure 2).Only five patients’ MRI sequences had included DWI, including four with mucinous adenocarcinoma and one with adenocarcinoma. Of the four patients with mucinous adenocarcinoma, two patients’ lesions presented as slightly hyperintense with focal hyperintense signal on DWI and hyperintense with focal hypointense signal on ADC map (Figures 1 and 3); the remaining two patients’ lesions showed slightly hyperintense signal on DWI and hyperintense signal on ADC map. One patient with adenocarcinoma showed lesions that presented as hyperintense on DWI and hypointense signal on ADC map (Figure 2).
Fistula between mass and anus:A fistula between the mass and anus was detected in six patients with mucinous adenocarcinoma and two with adenocarcinoma (Figure 2).In two patients with mucinous adenocarcinoma, the masses surrounded the anal canal and appeared to be connected to it.
Contrast enhancement of tumor:Only five patients received contrast material for MRI studies. The lesions of three patients with mucinous adenocarcinoma appeared as progressive mesh-like contrast enhancement or septal enhancement, and the inner margin of the lesion was rough (Figure 1). The lesions of two patients with adenocarcinoma presented with persistent heterogeneous enhancement (Figure 2), and the necrotic areas were unenhanced.
Contrast enhancement of peritumoral areas:Contrast enhancement of the peritumoral areas was noted in three of five patients who received contrast material.The boundary of the enhanced region was not clear and presented as slightly higher signal on FS-T2W I (Figure 4).
Regional lymphadenopathy:Perirectal and inguinal lymphadenopathy was noted in two of ten patients, and only inguinal lymphadenopathy was noted in five of tenpatients. In the remaining three patients, small lymph nodes were seen around the rectum or inguinal region (Figure 5, Figure 6,Figure 7).
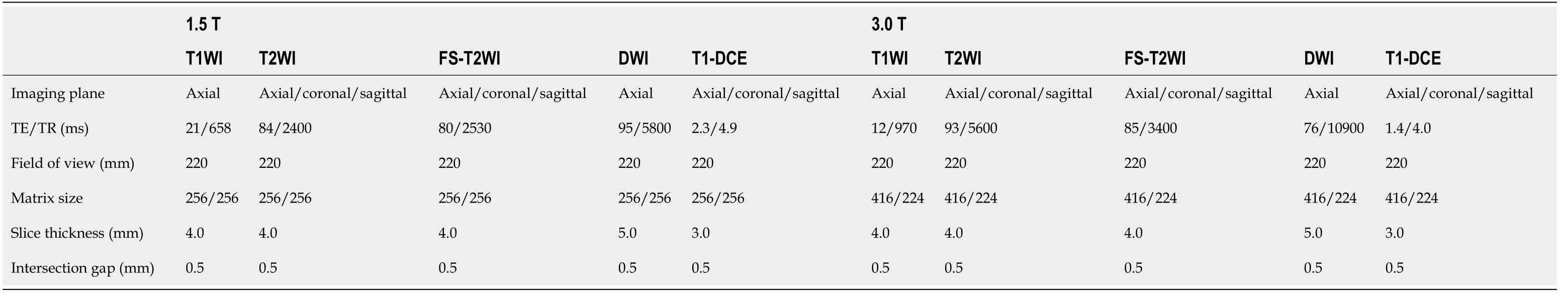
Table 2 Sequence parameters for magnetic resonance imaging in carcinoma arising from anal fistula
DISCUSSION
Carcinoma arising from an anal fistula is extremely rare. It was first reported by Rosser in 1934[12], and there have been few reported case series in the literature since then. The early diagnosis of carcinoma arising from anal fistula is very difficult either because the clinical manifestations are nonspecific and/or similar to the typical symptoms of perianal disease or because the tumor is very slow growing[14]. The risk of malignant transformation of chronic recurrent anal fistula should be seriously considered. When doctors are highly suspicious of malignant lesions, regular surveillance is recommended in chronic recurrent anorectal fistulas, and aggressive methods to rule out cancer are necessary.
The pathogenesis of carcinoma arising from anal fistula is not yet definite, but is believed to involve the following aspects: (1) Long-term recurrent chronic inflammatory stimulation and alienation of scar tissue; (2) Infection with HPV in patients with squamous cell carcinoma; and (3) Long-standing immunosuppression in patients with Crohn perianal disease[15].
Clinical and pathological features
A previous report suggested that this condition is slightly more common in men, with the average age at diagnosis being 55 years[11]. Our results were consistent with thisreport, given that most of our patients were male (8/10), and most of the patients were middle-aged or elderly (9/10; age range: 50-75 years).
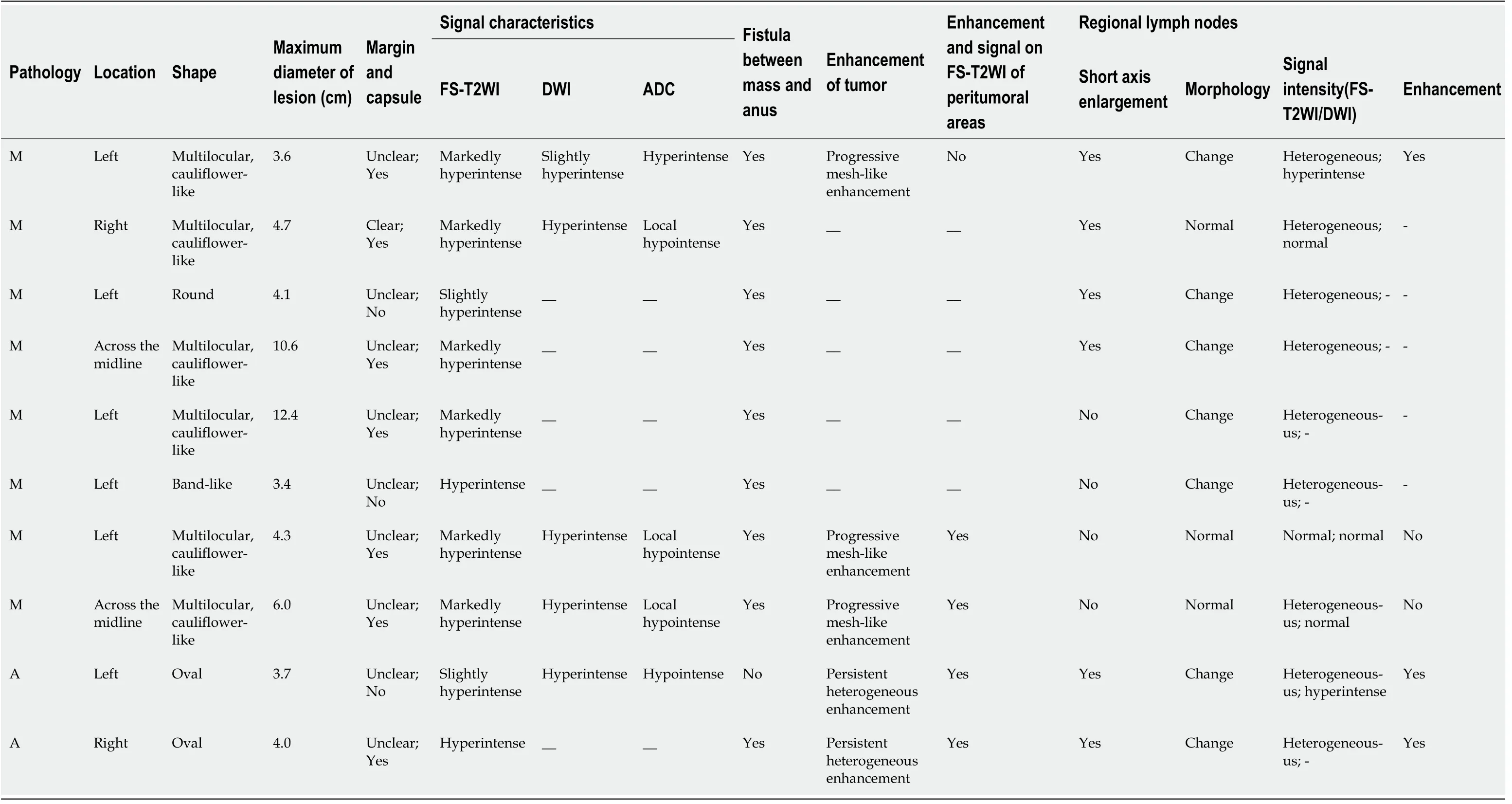
Table 3 Summary of magnetic resonance imaging findings in carcinoma arising from anal fistula
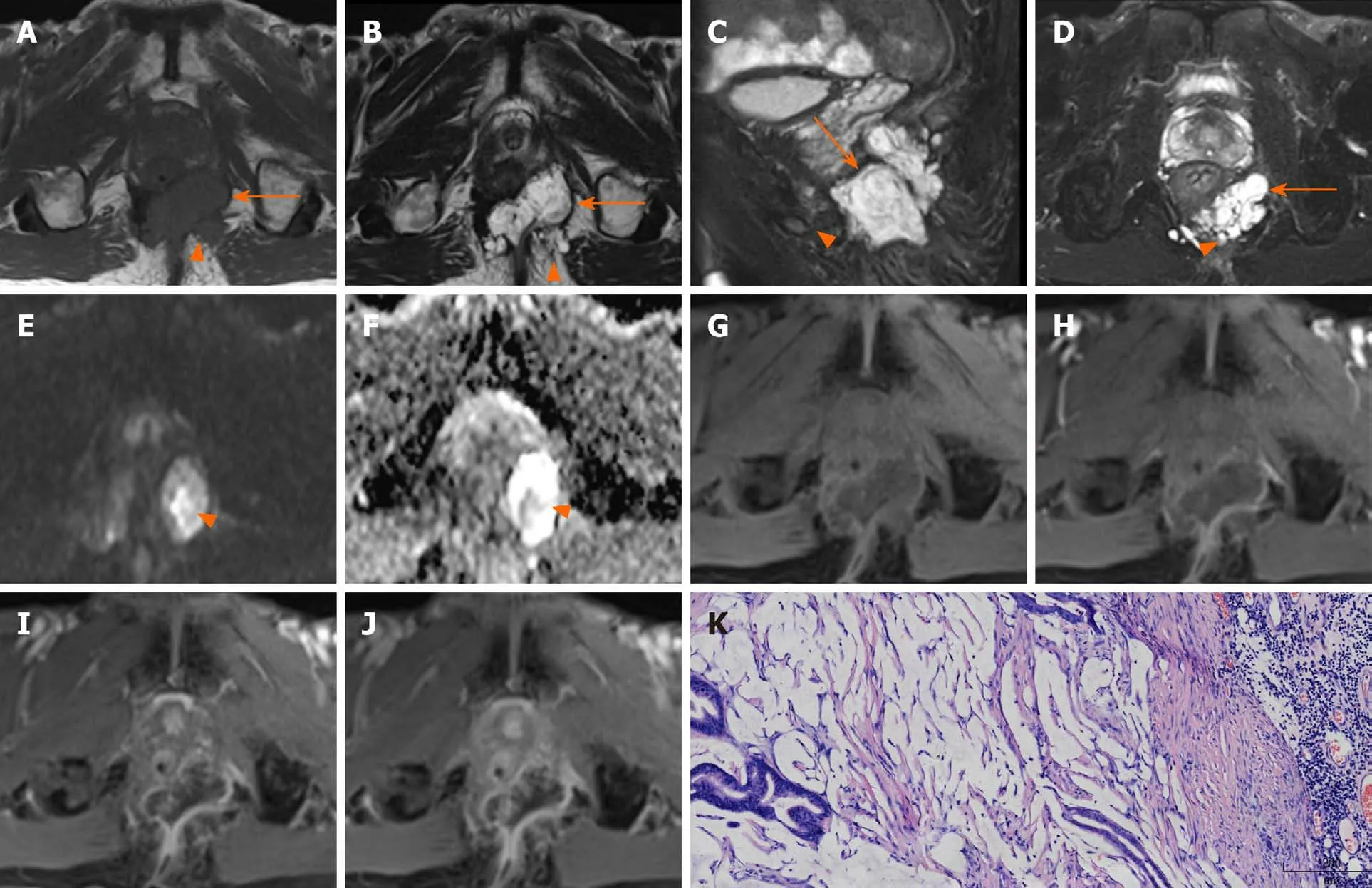
Figure 1 Magnetic resonance images of a 71-year-old man with mucinous adenocarcinoma. A: Axial T1WI; B: Axial T2WI; C: Sagittal FS-T2WI; D:Axial FS-T2WI. A-D images show that the tumor grew across the midline. This lesion was multiloculated, cauliflower-like, markedly hyperintense on FS-T2WI, with a thin capsule (orange arrows) and focally unclear boundary (orange triangles). E: Axial DWI shows a slightly hyperintense signal with focal hyperintense lesion (orange triangle); F: Axial ADC map shows hyperintense signal with focal hypointense lesion (orange triangle); G-I: Axial dynamic contrast-enhanced images show progressive mesh-like enhancement; K: The tumor was rich in mucus (hematoxylin and eosin staining; original magnification, × 100). T1WI: T1-weighted magnetic resonance imaging; FS-T2WI: Fat-suppressed T2-weighted magnetic resonance imaging.
There are three main pathological subtypes of carcinoma arising from an anal fistula—mucinous adenocarcinoma, adenocarcinoma, and squamous cell carcinoma[16-19]. Thomaset al[15]stated that the histology of adenocarcinoma was the most common (~59%); however, mucinous adenocarcinoma was the most common pathological type in our study (8/10). The possible reason is that previous studies considered only two major types, namely, adenocarcinoma and squamous cell carcinoma, and mucinous adenocarcinoma was classified as adenocarcinoma.
Head bowed in prayer, she sat in the pew near the back of the church. She paid no attention to the pastor, who was hanging the tablecloth across the unsightly hole. When the woman looked up and saw the cloth she rushed to the altar.
Early symptoms of carcinoma arising from anal fistula are similar to those of anal fistula or perianal abscess, usually without diarrhea or obstruction, which may help to distinguish from rectal cancer. Digital examination may reveal only an area of induration on the side where the fistula is situated. Six patients completely fulfilled the above criteria in our study, while in the remaining four patients, the anal fistula has been present < 10 years. To ascertain whether the standard “the fistula should usually antedate the carcinoma by at least 10 years” is still decisive, it is necessary to analyze a larger group of patients.
Abdominoperineal resection (APR) is the most common surgical treatment for this rare malignancy, and the effect of radiotherapy and chemotherapy is still controversial[15,17]. Prognosis of carcinoma arising from anal fistula is usually poor[20].
Magnetic resonance imaging findings
The masses could be unilateral or grow across the midline and typically surrounded the anal canal. The size of the tumor lesion could be relatively large. The mean of the maximum lesion diameter was 5.68 cm in our patients, and even exceeded 10 cm in two casas. In our study, the typical features of mucinous adenocarcinoma with respect to shape were multiloculated or cauliflower-like with internal septa. Hamaet al[10]hypothesized that the mucin pools produced by a mucinous adenocarcinoma without thick fibrous capsule may reflect that cancer cells have invaded the surrounding tissues before the fibrotic reaction. However, the perianal fistulas or abscess whose mucin was secreted by the anal gland had a thick fibrous capsule. We speculated that the thin capsule could still be seen in a mucinous adenocarcinoma, and the focal boundary of tumors was unclear, which could reflect the invasive nature.Adenocarcinoma lesions appeared ill-defined and had no capsule. Because of the small number of adenocarcinoma cases, the relevant characteristics could not be effectively summarized.
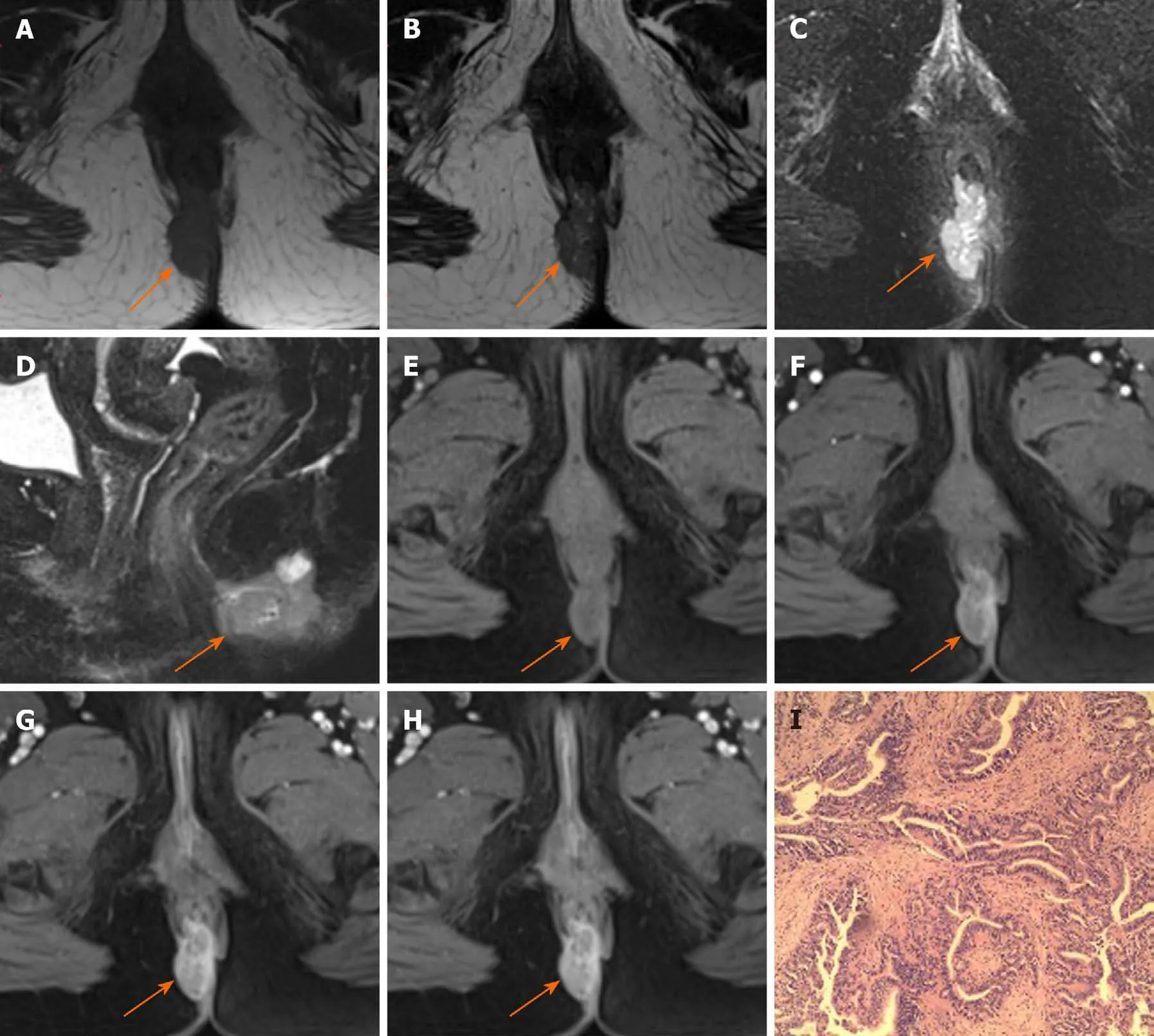
Figure 2 Magnetic resonance images of a 52-year-old woman with adenocarcinoma. A: Axial T1-weighted magnetic resonance imaging; B: Axial T2WI; C: Axial fat-suppressed T2-weighted magnetic resonance imaging (FS-T2WI); D: Sagittal FS-T2WI images show the tumor to the right (orange arrows). The tumor is oval and hyperintense on FS-T2WI without capsule. E-H: Axial dynamic contrast-enhanced images show persistent heterogeneous enhancement (orange arrows); I: Hematoxylin and eosin stained image (original magnification, × 200).
Mucinous adenocarcinoma mostly presented with markedly hyperintense signals on T2-weighted MR images, slightly hyperintense signals on DWI, and hyperintense signals on ADC map, which represented the signal of mucin pool. Some lesions of mucinous adenocarcinoma contained solid components, showing focal slightly hyperintense signal on FS-T2WI, hyperintense signals on DWI, and hypointense signals on ADC map. Adenocarcinoma showed heterogeneous high or slightly high signal on FS-T2WI, high signal on DWI, and low signal on ADC map.
Hamaet al[10]reported that a fistula between the mass and the anus is a characteristic finding of mucinous adenocarcinoma arising from an anal fistula. Our results are consistent with this conclusion because eight patients had a fistula between the mass and the anus, and two patients showed the masses surrounding the anal canal and appearing to be connected to the canal. Because of the history of anal fistula in all patients, whether the fistulas between the mass and the anus were caused by the tumor or the previous anal fistula remains to be further explored. At present, we are inclined to the latter possibility.
The lesions of mucinous adenocarcinoma showed progressively mesh-like contrast enhancement, septal enhancement, and rough inner margin. Although the number of patients with post-contrast MRI scan was small, the results were basically consistent with those reported in the literature[10]. Meanwhile, we considered that the progressively enhanced pattern was similar to that of the fiber, which was indicative of the existence of an internal septum and thin capsule. Adenocarcinomas presented with persistent heterogeneous enhancement.
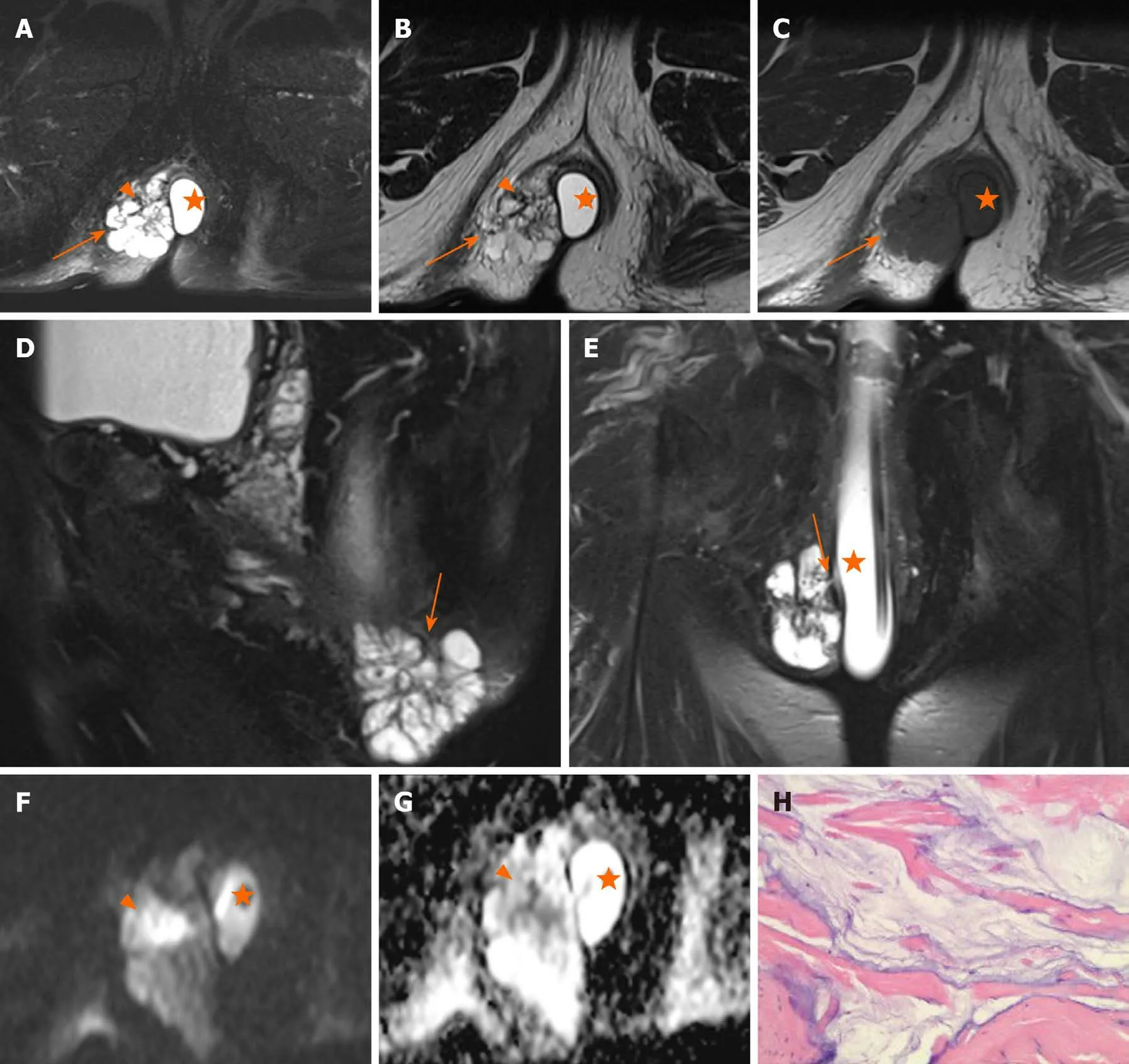
Figure 3 Magnetic resonance images of a 66-year-old man with mucinous adenocarcinoma. A: Axial fat-suppressed T2-weighted magnetic resonance imaging (FS-T2WI); B: Axial T2WI; C: Axial T1-weighted magnetic resonance imaging; D: Sagittal FS-T2WI. A-D images show the tumor to the right. This lesion was multiloculated, cauliflower-like, and markedly hyperintense with focal slightly hypointense signal (orange triangle) on FS-T2WI, with a thin capsule (orange arrows) and focally unclear boundary; E: Coronal FS-T2WI shows a fistula between the mass and the anus; F: Axial diffusion-weighted image shows a slightly hyperintense with focal hyperintense lesion (orange triangle); G: Axial ADC map shows hyperintense with focal hypointense lesion (orange triangle). Artificial water sac can be seen in the rectum (orange star); H: hematoxylin and eosin staining (original magnification, ×200).
Contrast enhancement of the peritumoral areas was noted in three of our cases.Hamaet al[10]believed that this could be a reliable finding reflecting the invasion of cancer cells. We found it challenging to distinguish contrast enhancement from enhancement of active inflammation. Considering the unclear boundary and the slightly hyperintense signal on FS-T2WI of the enhanced region, we suspected that the tumor invasion and inflammation were coexisting conditions. We recommend MRI reexamination after remission of inflammation.
Perirectal or inguinal lymphadenopathy was noted in seven of ten patients in our study. Unfortunately, pathologic confirmation could not be obtained. Iesalniekset al[21]found that approximately 50% appeared inguinal lymph node involvement and about 10% presented with distant organ metastasis. Therefore, we believe that the signs of lymph nodes are helpful in the diagnosis of carcinoma arising from anal fistula.
Differential diagnosis
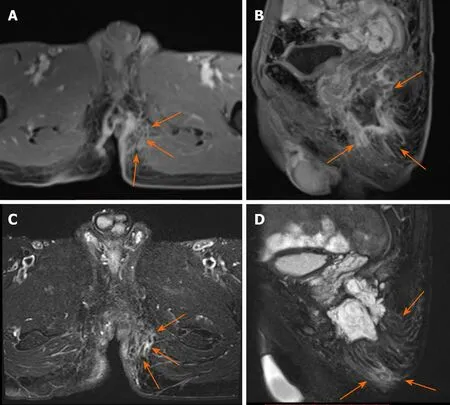
Figure 4 Magnetic resonance images of a 71-year-old man with mucinous adenocarcinoma. A: Axial dynamic contrast-enhanced image; B: Sagittal dynamic contrast-enhanced image; A and B images show the contrast enhancement of the peritumoral areas. The boundary of the enhanced region was not clear(orange arrows); C: Axial FS-T2WI; D: Sagittal FS-T2WI. C and D images show that the enhanced region was slightly hyperintense (orange arrows).
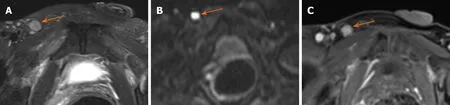
Figure 5 Magnetic resonance images of a 57-year-old man with adenocarcinoma. A: Axial fat-suppressed T2-weighted magnetic resonance imaging;B: Diffusion-weighted image shows that the lymph node was hyperintense; C: Dynamic contrast-enhanced image show right inguinal lymph node > 5 mm in the short axis, with irregular morphology and heterogeneous enhancement.
The fistula between the mass and the anus and the history of long-standing chronic anal fistula could be helpful to distinguish between mucinous adenocarcinoma arising from anal fistula and malignant transformation of cystic lesions in the pelvic cavity,such as a tailgut cyst, teratoma, or dermoid cyst[10].
Our study has some limitations. First, this was a retrospective study of patients from a single institution. Second, carcinoma arising from anal fistula is a rare diagnosis, and the sample size is therefore relatively small. It remains to be further analyzed whether imaging features of lesions could be completely summarized. Third, the included patients had a relatively long time span (between June 2006 and August 2018), and the corresponding MRI techniques were therefore not consistent.
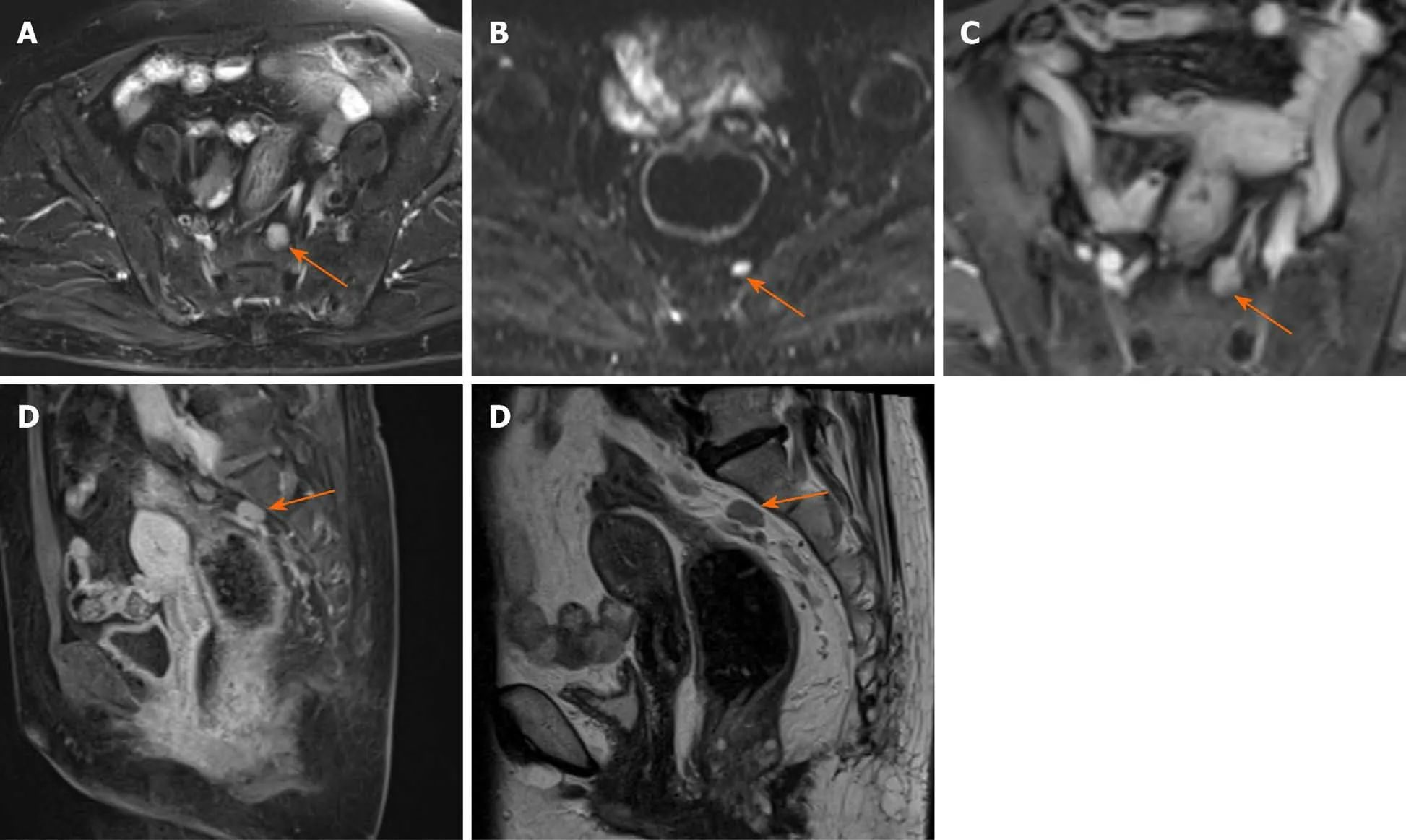
Figure 6 Magnetic resonance images of a 64-year-old woman with mucinous adenocarcinoma show perirectal lymph node with irregular morphology measuring > 5 mm in the short axis. A: Fat-suppressed T2-weighted magnetic resonance imaging; B: Hyperintense on diffusion-weighted imaging; C and D: Heterogeneous enhancement on axial and sagittal dynamic contrast enhanced magnetic resonance imaging; E: Sagittal T2-weighted magnetic resonance imaging.
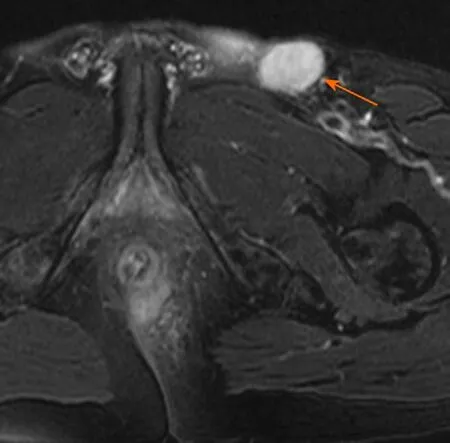
Figure 7 Magnetic resonance image of a 61-year-old man with mucinous adenocarcinoma. The left inguinal lymph node was round and > 5 mm in the short axis on axial fat-suppressed T2-weighted magnetic resonance imaging.
CONCLUSION
In conclusion, despite the first negative biopsies, clinicians should be highly suspicious of cancer in patients with chronic perineal fistulas whose symptoms change, and a repeat biopsy should be recommended. The definitive diagnosis of cancer arising from an anal fistula is always challenging. Therefore, multiple, repeated, and deep biopsies are essential for accurate and timely diagnosis. Although the number of cases was inadequate owing to the rarity of the disease, we believe that several characteristic MRI findings could contribute to accurate and timely diagnosis of carcinoma arising from anal fistula.
ARTICLE HIGHLIGHTS
Research background
Magnetic resonance imaging (MRI) is the standard investigation for suspected perianal diseases. This is important to early diagnose carcinoma arising from anal fistula, even if the incidence is low.
Research motivation
To describe and summarize the MRI findings of carcinoma arising from anal fistula.
Research objectives
To summarize the MRI manifestations of carcinoma arising from anal fistula to help improve the ability to diagnose this entity.
Research methods
A retrospective study was performed on ten patients diagnosed with carcinoma arising from anal fistula and confirmed by pathological diagnosis between June 2006 and August 2018. All patients underwent preoperative pelvic MRI. Five patients underwent enhanced MRI scans. Rosser’s criteria were used for diagnosing carcinoma arising from anal fistula. Morphologic features, signal characteristics, fistula between the mass and the anus, contrast enhancement of mass, signal and enhancement of peritumoral areas, and regional lymphadenopathy were assessed.
Research results
Most patients (90%) were older than 50 years. There were eight mucinous adenocarcinomas and two adenocarcinomas. The maximum diameter of the tumors ranged from 3.4 cm to 12.4 cm (median: 4.15 cm; mean: 5.68 cm). Eight patients had a fistula between the mass and the anus. Perirectal or inguinal lymphadenopathy was frequent (7/10).
Most lesions of mucinous adenocarcinoma were multiloculated and cauliflowerlike, with a thin capsule and focally unclear boundary. They were markedly hyperintense on fat-suppressed T2WI, slightly hyperintense with focal hyperintense on diffusion-weighted imaging (DWI), and hyperintense with focal hypointensity on apparent diffusion coefficient (ADC) map, with progressive mesh-like contrast enhancement.
Adenocarcinomas had an infiltrative margin without a capsule and appeared heterogeneously hyperintense or slightly hyperintense on fat-suppressed T2WI,hyperintense on DWI, and hypointense on ADC map, with persistent heterogeneous enhancement.
Research conclusions
A negative biopsy does not rule out the diagnosis of cancer, clinicians should be highly suspicious of cancer in patients with chronic perineal fistulas whose symptoms change, and a repeat biopsy should be recommended. The definitive diagnosis of cancer arising from an anal fistula is always challenging. Although the number of cases was inadequate owing to the rarity of the disease, we believe that several characteristic MRI findings could contribute to accurate and timely diagnosis of carcinoma arising from anal fistula in selection of puncture route and screening of high-risk groups.
Research perspectives
Earlier and better identification and monitoring of high-risk groups of carcinoma arising from anal fistula are required.
杂志排行
World Journal of Clinical Cases的其它文章
- Strategies and challenges in the treatment of chronic venous leg ulcers
- Peripheral nerve tumors of the hand: Clinical features, diagnosis,and treatment
- Treatment strategies for gastric cancer during the COVID-19 pandemic
- Oncological impact of different distal ureter managements during radical nephroureterectomy for primary upper urinary tract urothelial carcinoma
- Clinical characteristics and survival of patients with normal-sized ovarian carcinoma syndrome: Retrospective analysis of a single institution 10-year experiment
- Assessment of load-sharing thoracolumbar injury: A modified scoring system