Combined music and play therapy resolves chronic toddler sleep issues: a case report
2020-03-09DebHerdman
Deb Herdman*
1Nigh' Nigh Baby Sleep School, Victoria, Australia.
Keywords: Toddler sleep, Filial therapy, Music therapy, Play therapy
Introduction
As many as 80% of parents describe unresolved and prolonged infant and toddler sleep and settling difficulties with their children in the early formative years to age 3 or more. Despite a plethora of interventions available to parents, chronic family sleep deprivation affecting mental, social, physical and emotional health persists. This report focuses on a system allowing families to develop improved sleep through nurturing when their child is emotionally stable to cope with sleeping unassisted, rather than enforced sleep training.
Ann and Tom (names changed for client confidentiality), presented to their general practitioner for a paediatric referral to investigate their 2-year-old daughter's poor sleep, frequent overnight waking, delayed settling and early rising, which was severely affecting parenting and family dynamics. Then, referred to me for consultation, the parents have initiated a methodology devised from my work using a play therapy and music therapy approach that provides consistent and lasting sleep improvement.
Focusing on 3 repetitive interventions of Routine, Re-connection and Relaxation, toddlers are able to feel more confident and relaxed which helps them settle to sleep faster, sleep throughout the night and wake up at an appropriate time of the morning. The play activity is specific and forms part of the presleep time routine. The music therapy intervention through lullaby and instrumental addresses the need for interaction between parent and child to satisfy emotional wellbeing. Relaxation, resulting in faster and deeper sleep is accomplished from the instrumental component. Adequate sleep is essential and integral to a good mind and body healthy in the formative years and directly correlates to positive family dynamics, brain and physical health, cognitive growth and general well being.
In the first half of 2007, I gave birth to my third child after 5 years of secondary infertility. This joyous moment ended a pregnancy of severe nausea and hyperemesis, chronic constipation from pharmacological intervention to ease nausea and many episodes of 'bowel prep' medication resulting in diarrhoea to counteract constipation. A sudden and unplanned caesarean delivery without labour at 38 weeks, saw the beginning of parenting after a gap of 21 years my between babies.
My baby boy did not settle easily and slept in short bursts, often 20-30 minutes long and seemed to cry a lot. Despite natural colic medication, and supplementary feeding due to breastfeeding low supply his 'cat-napping' persisted. As most parents find in this situation, the baby cries unless being in the parents' arms and only then sleeps peacefully. This situation is not limited to daytime and can affect night-time sleep over many months and years. For me, I could afford the luxury of being a stay at home mother, and cherished the essential attachment my baby desired, but, there came a time when I longed for him to sleep and settle without having to be in my arms. Sleeping improved naturally, around 10-11 months of age. Up to this time, various and commonly recommended infant sleep methodologies were tried, including a very limited attempt at 'controlled crying/comforting'. I found this stressful as I'm sure it was to my son, and completely in opposition to my attentive, responsive and nurturing approach to parenting. A short stint of good sleep followed, then his sleep pattern changed during toddlerhood. At this point in my nursing career, I was working two part-time jobs as a scrub/scout in theatre and in a neonatal special care baby unit, working permanent nightshift. His settling to sleep was taking up to 3 hours and a general lack of sleep was affecting my emotional health and parenting. I was keen to use music but found traditional lullabies had distasteful lyrics, were too long and hard to remember and usually required many vocal repeats which were vocally challenging and exhausting when my toddler asked constantly for 'more'! No music accompaniment was available and when it was, constantly changing tracks made for inconsistency. Turning to instrumental music, other problems like changing music dynamics meant irregular volume, changed tempo and inconsistency for soothing my sensitive baby. The absence of lyrics deprived me of the pleasure of lullabying my son, and important neurological benefits to enhance bonding. When my baby turned two, I became a student of piano, having no former music education. As a tired and stressed working mother, I found a great console in playing and experiencing the joy of learning to read, play and make music. In 2010, I composed a lullaby of lyric and instrumental that met with what I felt, was necessary to help my two-year-old toddler, sleep better. I soon realised this was a very easy, effective and systemised way to promote not only his sleep independence but also deeper sleep which directly improved sleep for the whole family.
In conjunction with the music therapy system called '3 R's to sleep success', I included play therapy, which is used as a positive sleep association activity. The purpose of play therapy before sleep time is to allay initial stress hormone release, which can lead to long, protracted settling, increased hyperactivity, irritability and shortened sleep hours. Parents are also affected by fewer sleep hours, broken sleep and stress when children have poor sleep and settling habits. The methodology has shown consistent results similar to the case presented since 2011. Parents have reported similar histories for problematic sleep, failed interventions and subsequent success, or at the least marked improvement using combined play and music therapy or just the music therapy component.
Case presentation
First-time parents Ann and Tom presented to me for help and intervention to assist with their toddler daughters continued and excessive waking. At the consultation, their toddler was two years and two months of age and of white Australian ethnicity. From previous medical assessment, 'Emma' shows no dysmorphic features and no medical-based reason have been identified for her chronically poor sleep history. Her developmental history as told by her mother describes a pregnancy of 'horrendous' morning sickness with threatened preterm labour before 35 weeks. Carrying the pregnancy to term, long traumatic labour culminated in an emergency C-section. Birth weight was within normal parameters with Apgar scores of 9 at 1 minute of age and 9 at 5 minutes old. Feeding was via breast until weaning at 14 months. 'Emma' is fully immunised and her parents report common childhood ailments often associated with being in childcare, which began around 10 months of age. Initial parent separation anxiety had settled at the time of consultation.
Her parent's report 'Emma' has never slept well from birth and catnaps and wakes frequently overnight. Her usual sleep pattern consists of prolonged settling time and usually not falling asleep until 9:30 pm or later, followed by 2, 3 or more overnight waking's until morning, which starts at around 7 am. She does not sleep consistently outside of the home, including in the car, but they feel naps well at the childcare centre, which she attends 4 times per week. Ann and Tom have been chronically sleep-deprived for some time and have tried a number of usual interventions to improve baby Emma's poor sleep pattern. Ann has opted to use a dummy (pacifier) to help with settling and sleep. During infancy, baby wrapping did not seem to help with settling. She mentioned they had tried to enforce a strict bedtime routine with dinner, bath-time, reading books, a favourite bedtime song, and music but found Emma was still taking hours to get to sleep. Often it would be after 9:30 pm before she settled to sleep. They had then tried to 'wear' her out with time outside on the trampoline, walks, playtime and so on. A common feature of over-tiredness seen in young children is hyperactivity. Parents often call this 'hypo' and some may refer to their children as 'bouncing off the walls'. They also tried co-sleeping in their bed and sharing Emma's bed to be close at hand to comfort her back to sleep. Realising their daughter seemed to be an anxious and nervous baby, they were not keen to try interventions that increased anxiety, but eventually due to desperation for sleep, 'controlled crying' was initiated for a period of 1 to 2 weeks. 'Emma' continued to wake overnight. Ann stated this made her more anxious and certainly added to parent stress. Ann had also spoken via telephone to a sleep school some distance away that promotes routine and controlled comforting. She felt this service did not offer her gentle support options. She did not attend any residential sleep school options and stated she did not want to revisit controlled comforting/crying as an intervention. Other interventions included non-prescription herbal sleep mixtures and 2 months of melatonin 1mg up to 5 nights per week. She was still taking 2-3 hours to settle to sleep, despite drug intervention. As professional working parents, Ann and Tom found they needed to parent Emma overnight in shifts in order to get some sleep continuity. Ann would attend to 'Emma' from settling to 2 am and Tom 'on duty' from 2 am to 7 am. Both parents felt exhausted and barely able to function after years of broken and irregular sleep hours. Scoring Ann for her coping ability, she rated herself as minus 5 on a scale of 0-10 with 0 equal to feeling desperate for help and 10 coping well. Added to the stress of sleep deprivation, there was limited extended family support.
The intervention: 3 R's to sleep success
The intervention uses a systematic approach that focuses on three precise components of routine, re-connection, and relaxation (Figure 1). Routine is where play therapy is used and makes the process of preparing for sleep a positive interaction. Using 'Sleepy Head TED©' a 450mm tummy sleeping polar bear, parents are instructed on a short series of actions that are repeated at each bedtime.
Firstly, TED is presented to the toddler naked. Conversations with the child around bedtime for 'TED' are encouraged, with the child (depending on age) assisting with dressing the bear into his 2 piece pyjamas. This can be carried out simultaneously with the child getting into sleepwear. 'TED' has magnetised paws and a game of peek-a-boo is an appropriate but not too energetic, fun way to disengage the child from sleep associated anxiety. The bear, with long front arms, is offered to give cuddles to the child, assisted by the magnetised paws for grip and is only presented at bedtime for a positive sleep association. The bedtime routine is kept to a consistent settling time and the same sleep space. This is important to enforce discipline around sleep time and gives the child a sense of knowing what's to come and therefore a deeper sense of security. Re-connection is commenced and is important for emotional support. Many children ask in a verbal or non-verbal way for a parent/caregiver to stay with them at sleep time. This could be as simple as the child crying, calling out when left alone, or as often is the case with older children, asking for many things to delay parents leaving them alone. In this methodology, 'Nigh' Nigh' Sleepy Head' TM music therapy is actioned. Beginning with lullaby lyrics that talk about going to sleep, i.e.… 'Nigh' Nigh' Baby Time to go to bed'; it is strongly encouraged for the parent to sing, or at least hum the words to enforce that sleep is the expectation. The tempo is set to a resting heart rate of 80 bpm, with the music arrangement consistent with acoustic instrumentation of piano, strings, harp, etc. The lyrics are repeatable, simple and designed for the child and caregiver to easily remember and sing as lullabying is uniquely satisfying to produce hormonal responses that change the mood and enhance bonding.
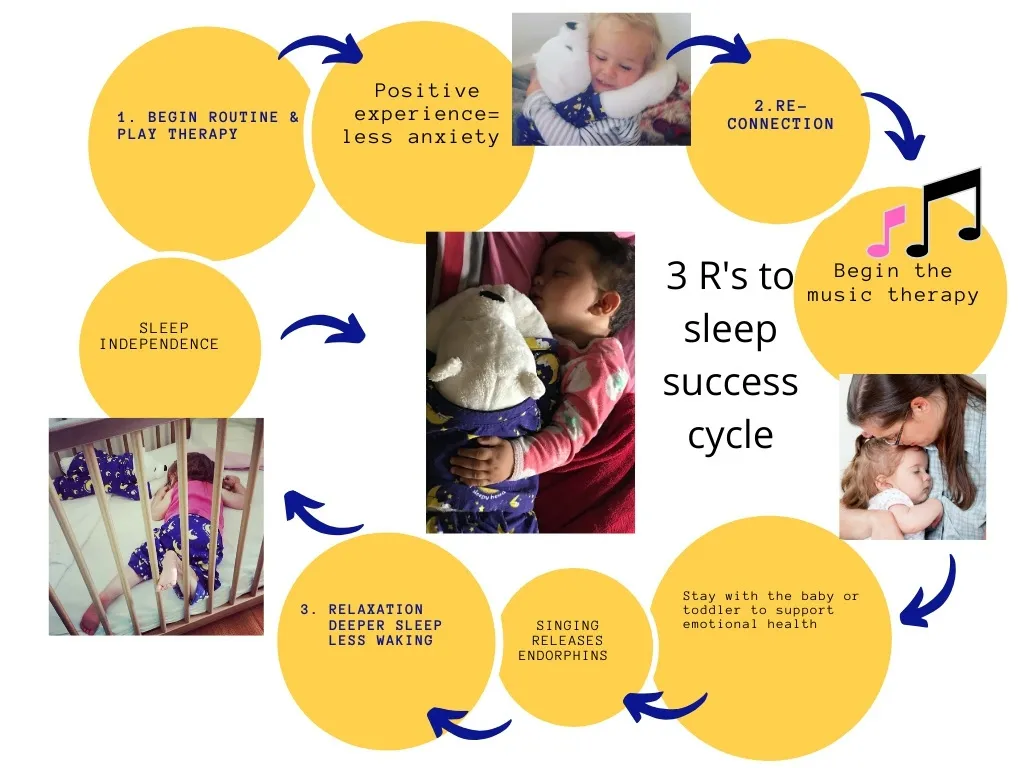
Figure 1 The intervention: 3 R's to sleep success
This is an important phase where sleep confidence is attained as children feel secure enough to move toward the ability to self settle without stress and anxiety. Relaxation is essential for a longer and deeper sleep. This part of the music therapy is without a lyric, purely instrumental but of the same former melody with counter melodies for added interest. The acoustic instrument sounds are replaced with synthesised sounds that become less complex over the course of the 47 minutes (approximate child sleep cycle) with the ending fading to silence.
Follow-up and outcomes
Ann and Tom left the initial consultation with a new sense of hope and happiness that this methodology was a gentle and nurturing approach to help baby Emma. Parents were sent, via email, a plan of action as discussed in the consultation. A follow-up phone call was made 10 days post consultation with Emma's mother. She stated that toddler Emma had responded very positively to the playing resource even sleeping well in the car on the way home after the first initial consult. There were also some positive results with less night waking. Email follow up occurred at 29 days post consultation with Ann indicating a marked improvement with Emma's sleep… "We have mostly good nights with little or no waking, and now the horrendous nights are the exception, rather than the norm". Settling had shortened with sleep accomplished by 8:30 pm instead of the former 9:30 pm or later. Ann remained anxious for earlier settling to be accomplished. She has described that when she reverts back to 'old methods' her partner has actively encouraged and reminded her to stay true to the 3 R's to sleep success methodology. At 9 weeks post-consultation, parents report Emma has many consecutive nights without waking. Ann's anxiety around a faster sleep time has been allayed with the mother realising her daughter is still needing emotional contact. She says "Now I am using this time to relax while giving her a cuddle". Commonly parents are after instant results, which sometimes do happen, but when there is prolonged anxiety and the sleep issue has become chronic, the child needs to be nurtured in order to become confident and relaxed about sleep. Then, sleep settling and sleep independence without constant parent input, can occur.
This case highlights a positive improvement in family sleep using music and play therapy even after years of failed interventions in chronically sleep-deprived subjects.
The strengths of this are based on a plethora of research that supports the benefits of lullaby, music, and play. Addressing parent and child emotional health with positive and stress-free intervention 'use at home resources' appears to be of significant value. Ann and her partner have been able to support each other as consistency amongst caregivers mean the child is getting the same message and avoids confusion. Routine is an essential component but as seen in this case, and common amongst other families, not effective enough in many situations. Sleep times require regulation and consistency as irregular bedtimes alter the amount of sleep and can contribute to a persistently 'jet-lagged', exhausted and irritable state. Lack of sleep also causes common sleep-associated problems of difficulty falling to sleep, waking, restless sleep and waking too early. Some studies show reduced or disrupted sleep in children at certain developmental stages have long term cognitive impact resulting in lower reading, maths, and spatial awareness scores. Hyperactivity, conduct problems, and emotional difficulties can become prevalent and worsen with age [1]. Although routine gives children a sense of predictability, stress and anxiety increase cortisol which can undermine and prolong settling as it takes time for circulating stress hormones to return to normal. This can contribute to sleep irregularity and fewer sleep hours. Routine is necessary for helping children develop a sense of organisation and expectation. In my capacity as a music therapy sleep consultant, a routine is often well implemented and yet sleep remains problematic and often chronic. I believe stress and anxiety combined with over tiredness contribute to the problem. These issues need to be addressed to achieve faster settling and improved sleep. Incorporating play therapy into the sleep time routine is psychotherapeutic and can help regulate negative behaviours that have a high emotional impact. Anxiety, both from the parent and child can elevate cortisol and adrenaline. This increased stress adds to emotional fragility and fatigue and can adversely affect the parent/child dyad. The act of using the Sleepy Head Ted© bear as a visual and tactile resource provides the parent with a set task. Play therapy of this nature, where the parent is taught the play intervention is described as 'Filial Therapy'. Formulated by Bernard Gurney in 1964, it is hypothesised that benefits occur from 'parental skill acquisition, a sense of parental self-efficacy, decreases in negative parent-child interactions, and an increase in positive parent-child interactions' [2]. The play intervention at the routine stage formerly engages the child's attention with corresponding positive interaction to enhance bonding. Care is taken not to overstimulate the child as the focus is around preparing for sleep. Even when the child is not keen for sleep, with imagination, the focus is on getting 'TED' ready for sleep. It is a powerful and gentle way for filling a young child's emotional cup, which I believe is particularly pertinent and important in today's busy and often distracting culture where parent/child interaction is frequently interrupted. The lullaby and music component is part of the re-connection stage for the child with the parent/caregiver and is where important sleep patterns begin to change. The play therapy has set a more relaxed precedent for going to sleep but for many children, there is an unwillingness to detach from the parent and simply go to sleep. Sometimes this is accomplished by enforcing a series of 'rules' like controlled comforting/crying/graduated extinction which all generally follow the same principles of leaving the child alone for specific amounts of time with crying and increased anxiety a common feature. I believe if a child is stressed and looking to the parent for support, it is a fundamental and nurturing response to engage with them.
With global figures raising in mental health disease it's seems important to be considerate of the child's emotional needs especially in the formative years, to enhance the development of neurological social networks that have long-lasting and positive effects. When singing is introduced in the re-connection stage many positive benefits follow. Singing is an active form of communication and more effective for baby's brain than passive listening. This is particularly important in those easy stages of changing sleep behaviour when parent support is needed in order to progress to sleep independence. Although parents will assume they cannot sing, their baby will not care, as they are comforted by the sound of a familiar voice. Parents that are self-conscious of their own singing voice can begin with humming and with increasing confidence progress to lyrics.
Discussion
Lullabies are made up of rhythm, repetition, and rhyme. They act to soothe the senses and in doing so can alter the mood. Trehub and colleagues showed that babies listening to music remained calm twice as long as babies listening to speech [3]. The very act of singing causes more air to enter the lungs, returns cortisol to normal levels, and releases hormones endorphin and dopamine that make us feel happier [4]. This can affect parent mood, resulting in a more relaxed disposition. A more relaxed parent produces a calming effect for the child. In addition to singing, music has been found to affect physiological states. Greater Ormond Street Hospital studied the effects of music and lullaby on paediatric respiratory/cardiac patients. Dr. Nick Pickett, who oversaw the study at the hospital and has worked with cardio-respiratory patients at GOSH for the past 20 years, said: "Parents have been singing to their children for thousands of years and they have always instinctively known that it helps their children to relax, but it's exciting to have scientific evidence that lullabies offer genuine health benefits for the child". Measurable outcomes included lowered heart rate and reduced pain, and improved wellbeing to the patient, family, and staff [5]. This could mean earlier patient discharge with significant well-being and economical advantage. In her book, 'The Lullaby Effect', Dr. Anita Collins shares many insights into the advantages of singing in the early formative years from many leading researchers. She says "all this research shows that we use music and singing…to create a bond, to induce trust, as a signal of familiarity and safety, to reduce stress and moderate the emotional state of parent and baby" [5]. It is an easy and effective way to get desired emotional outcomes that can aid sleep and settling. Children that suffer sleep issues cannot be viewed in isolation but rather in the context of the family unit. Irrespective of whether the cause is parent-driven through behaviours and beliefs about sleep, external stressors adding to family tension or derived from the child's own genetic makeup, sleep deprivation is a serious health issue.
Fatigue can contribute to maternal and paternal depression with sleep problems in Australian children causing psychological distress among mothers and poor general health among both mothers and fathers [6]. Family dynamics also become stressed between partners, other siblings and, can carry over into parent employment. Mental and physical health ultimately suffers which can impede work and earnings and lead to the breakdown of the family unit. Researchers have found that at certain developmental stages the effects of inadequate sleep can have both short and long-term adversity as memory and learning capacity declines and general health is affected by lower immunity. Studies in the paediatric population have found a distinct correlation between the lengths of the telomere on DNA strands. Shortening of the telomere is seen in ageing and lack of sleep. If lack of sleep causes physiological changes and impaired health, longitudinal follow up studies are yet to determine long term adversity [7]. Furthermore, a correlation may exist from tiredness related behavioural issues giving false diagnoses of Attention Deficit Hyperactivity Disorder [8]. Sleep or lack of it, appears to be a global problem but is it a new problem for parents? As a sleep consultant, I've heard many parents describe their nowadult children as being 'dreadful sleepers'. Previous parenting trends advised parents to let babies cry in order to 'learn' to sleep. Are we seeing an increase in sleep problems because parents are not inclined to follow harsh sleep regimes or are children overstimulated or affected by overstimulated and stressed parents? Irrespective of the cause, I believe the longer parents struggle with sleep deprivation the longer it takes for children to develop good sleep habits. Without any intervention, a percentage of children will become adults with poor sleep habits that can severely undermine health. Despite parents trying to help their children sleep, I believe the problem can be resolved using a combination of emotional support, lullaby, music and play therapy intervention. Although this case report is representative of one family, the methodology has shown outstanding anecdotal results across various scenarios from prenatal (foetal relaxation), travelling with distressed infants, paramedics as a calming tool for paediatric patients, and as a self-regulatory tool by toddlers when they feel anxious. Further studies with larger populations are warranted and study populations could include traumatic pregnancy—calming mother and baby for good postnatal outcomes; early intervention to prevent poor sleep issues, improving mother and father bonding with their infants, interventions to lessen sleep-deprived PND, influencing family dynamics in NICU, resolving chronic toddler sleep deprivation, ADHD and poor sleep in the paediatric population, and pain management for the teething infant. Addressing child and parent anxiety using both music therapy and play therapy intervention promotes relaxation, alleviates symptoms of sleep debt and allows sleep independence to occur naturally for the child without subjection to increased anxiety. This means families have improved physical, mental and emotional health promoting a stronger family unit which benefits the extended community and economy through better sleep health.
杂志排行
Life Research的其它文章
- Drug-related problems among type II diabetes mellitus patients with hypertension: a cross-sectional study
- A meta-analysis of the treatment of cancer-related insomnia with acupuncture
- Contrasting cognitive behavioral therapy for insomnia to analyze sleep theory in Laolao Hengyan
- A review of the treatment for insomnia in patients with cancers
- A review on the effects of sleep duration on hypertension
