Drug-related problems among type II diabetes mellitus patients with hypertension: a cross-sectional study
2020-03-09JosephNzayisengaNicholasNjauNgomiJohnNyiligira
Joseph Nzayisenga*, Nicholas Njau Ngomi, John Nyiligira,
1Kibuye Referral Hospital, Kibuye, Rwanda. 2Mount Kenya University, Kigali campus, Rwanda.
Keywords: Drug-related problems, Type II diabetes mellitus, Hypertension, Kibuye Referral Hospital
Introduction
Diabetes and hypertension (HTN) are the most silent killer non-communicable diseases in both developing and developed countries all over the world [10, 20]. Diabetes is a disease that occurs when blood glucose (blood sugar) is too high [18], which leads to other organs damage mainly the heart, eyes, blood vessels, nerves and kidneys [28]. The commonly prevalent diabetes type in an adult is type 2 diabetes which occurs when the body does not make or use insulin well (the body becomes resistant to insulin or body doesn't make enough insulin) [1, 28]. According to the World Health Organization (2016), comprehensively 422 million people have diabetes; 1.6 million deaths were straight credited to diabetes consistently. The number of people with HTN in 2025 is evaluated to increase by 60% with sums over 1.5 billion [27]. The study by Shaw et al. (2010) showed that there would be an expansion in the number of individuals with diabetes from 171 million out of 2000 to 366 million by 2030. This number will ascend at 69% of people with diabetes in developing countries and in developed countries at 20% [24]. A poor control and inadequate or inappropriate treatment of both type II diabetes mellitus (T2DM) and HTN can lead to cardiovascular diseases (CVD), peripheral vascular disease (PVD), coronary heart disease (CHD), acute myocardial infarction (AMI), renal impairment, dyslipidemia, stroke, liver impairment, asthma, benign hyperplasia, gouty arthritis and osteoarthritis [4, 9, 16]. Diabetes mellitus type 1 and type 2 are both found in Rwanda but mostly T2DM is more prevalent accounting for 90% of all diabetes mellitus [3, 26]. According to the Rwanda diabetes association, the diabetes atlas shows that the prevalence of diabetes in Rwanda is 3.16% and 1,918 deaths are diabetes-related deaths per year [22].
HTN is the most frequent co-morbid condition in diabetic patients as it affects more than 60% of diabetic patients [12]. Drug-related problems (DRPs) can direct to low control of blood pressure [17] which are the main contributor prolonging hospitalization, rising mortality or morbidity and rise up expenditure of health care [13]. Patients with T2DM and HTN have multiple factors that are influencing the presence of a high prevalence of DRPs [30]. Poly-pharmacy is a significant factor of DRPs as the patients with T2DM and high blood pressure (HBP) complex the pharmacological management [17, 30]. The advanced age is another factor as it linked to the increasing complexity of drug monitoring pharmacokinetically and pharmacodynamically during patient health care [17]. Renal impairment, Liver impairment and multiple medications have been shown significant association to drug-related problems [13].The health quality of patients is mostly related to drug therapy use [7, 23], however improper use of drugs may lead to harmful side effects and adverse events [8, 15]. The patients who take more drugs (poly-pharmacy) bring challenges of drug selection for appropriate management of their condition [5, 11]. The Optimization of drug therapy and preventing problem-related to drug therapy saves the health care expenditure, particularly save lives, and enhance patient's quality of life [6]. Therefore, as there are no local study of DRPs among patients with T2DM and HTN, this creates a gap for knowing the status of DRPs particularly among patients with those conditions.
Methods
Research design
This study was a cross-sectional study. It was conducted to investigate DRPs among T2DM patients with HTN admitted at Kibuye Referral Hospital (KRH). The data were analyzed quantitatively. The prevalence and causes of DRPs were determined and factors influencing DRPs were established among T2DM patients with HTN admitted at KRH. Both exposure and outcome were assessed at the same time as it was a cross-sectional study.
Study population
The target population was 450 files of T2DM patients with HTN, aged 18 years old. Who was admitted and hospitalized at KRH for their condition managements, from January 2013 to December 2017. The sample size determined using Fischer formula [14]. Where n = Z2Pq/d2, n: sample size, P: proportion of patients with DRPs, q: the proportion of patients without DRPs (q = 1 - P), d: precision level and t: Z-score at a confidence level of 95%. The literature review of DRPs among T2DMs patients with HTN co-morbidities did not show local study; particularly in Rwanda. Hence the prevalence of 50% was adopted. A sample size of 385 patients' files was determined.
Inclusion criteria
i. Adult patients aged 18 years old and above with T2DM and HTN admitted at KRH from January 2013 to December 2017.ii. Patients who were admitted in a ward at KRH from January 2013 to December 2017 and used at least one anti-diabetic drug and at least one antihypertensive agent.iii. A patient who was diagnosed with both T2DM and HTN at KRH from January 2013 to December 2017.
Exclusion criteria
Patient's file with missing data of a patient admitted at KRH between January 2013 and December 2017.
Sampling technique
The simple random sampling was used for sampling patients' files among T2DM patients with HTN. A list of all patients' files who met inclusion and exclusion criteria was generated; each patient's file was marked with a specific number. A table of random numbers was generated based on a random number list generator [21] and that table was used to select a sample size of 385 patient's files from 450 total patients' files. A checklist contained demographic characteristics, clinical characteristics, DRPs and related causes were used. The classification scheme version 8.02 of pharmaceutical care network Europe (PCNE) was adopted to classify DRPs and causes of DRPs. This classification tool was utilized freely in pharmaceutical care study and practice, as long as the PCNE affiliation authorized its utilization.
Procedures of data collection
The data collected from KRH patients' files met the inclusion and exclusion criteria. A pharmacist was included in the data collection team. Independent variables were socio-demographic characteristics such as gender, age, marital status, lifestyle status and level of education. Also, the clinical characteristics such as blood glucose level, type and number of medication used, glycated hemoglobin (A1C) status, co-morbidities, hypertension complications, duration of hospital stay, and level of blood pressure were collected and recorded. The dependent variable (outcome) was DRPs. All data above was collected and entered into STATA software version 13.
The validity of the checklist
The validity of the checklist is to quantify what is proposed to measure and guarantee the legitimacy. The PCNE tool was adopted. It was the order conspires for drug-related problems adaptation 8.02 [19]. This tool was utilized freely in pharmaceutical consideration research and practice, as long as the PCNE affiliation authorized regarding its utilization and aftereffects of approvals [19]. This tool had been utilized in different DRPs studies [13, 29].
The reliability of checklist
Reliability was used to estimate the stability of the measures in order to ensure the reliability of the questionnaire or checklist. The pilot study conducted at Mugonero district hospital. A sample of 10 patients' files from Mugonero district hospital was used for the pre-test. The statistical analysis through STATA version 13, the internal consistency was good (0.8 ≤ α < 0.9), with scale reliability coefficient (α: Cronbach's alpha) equal 0.8303, for that reason the checklist was reliable.
Data Analysis
After data collection, data was entered in Excel and encoded, verified for omission and errors. Then after data was imported into STATA version 13 and verified again for omissions and errors then analyzed. Descriptive statistics (frequencies, percentages) method was generated. The categorical data was stated in percentages (%). At first round, univariate analysis was performed to describe independent variables then bivariate and multivariate analysis were performed to find the association between independent variables and DRPs. Fisher exact test performed in bivariate analysis to test the association between categorical variables. Only those with a P-value less than 0.05 were considered significant and then multivariate analysis was followed. Logistic regression was performed in multivariate analysis for adjusting the possible confounders. Only the independent variable which was found to be statistically and significantly associated with dependent variables under this study was adjusted for possible confounders using multivariate analysis. The results were presented in tables and pie charts.

Table 1 Patient's socio-demographic characteristics among T2DM patients with HTN
Ethical Consideration
Before starting data collection to conduct this study, approval (ethical clearance) to conduct the study was sought from the Mount Kenya University Rwanda (MKUR) School of postgraduate study (in Supplementary materials). The permission to access the medical records was obtained at KRH administration. Due to the nature of the study, no informed consent form was needed. Confidentiality was sustained through data collection and through the research process.
Results
Patient's demographic and clinical characteristics Patient's demographic characteristics. Socio-demographic characteristics deal with descriptive information of gender, age, education level, marital status, and patients' lifestyle among T2DM with HTN. The most prevalent T2DM patients with HTN were females with a proportion of 238 in 385 (61.56%) and a majority of patients were under 45 years old with a frequency of 282 in 385 (73.25%), which demonstrated that there was a problem shift to young people (Table 1). Concerning patients with T2DM and HTN education level and marital status most of them had education below A level and were married respectively (307; 79.75%) and (208; 54.03%). Regarding the lifestyle of patients with T2DM and HTN, most of them had not practice physical exercise (341; 88.57%), had a high body mass index (BMI) with respectively overweight (150; 38.96%), and obesity class (88; 22.86%).
Patient's clinical characteristics among T2DM patients with HTN. The patients' clinical characteristics such as blood pressure status, duration of hospital stay, duration with T2DM and HTN, glycated hemoglobin status, diabetes complication, number of co-morbidities and number of medication were identified medical record (Table 2). The majority of HTN cases (237; 61.56%) were classified as stage I HTN. Most of the patients had stayed in hospital more than or equal to 15 days (231; 60%). The half of patients their duration with T2DM and HTN co-morbidities were unknown (211; 54.8%) and other cases of patients had stayed with T2DM and HTN co-morbidities not more than 10 years (163; 42.3%). Most patients had diabetes foot ulcer (112; 29.09%) as diabetes complications. The majority of patients had less or equal 2 co-morbidities, most of those co-morbidities were osteoarthritis (120; 31.1%). Majority of patients had used five or more kinds of medicines (270; 70.13%).
Presentation of findings
Findings were based on the Pharmaceutical Care network Europe classification scheme of drug-related problems (PCNE-DRPs). The essential order presently had 3 essential sections for medication-related issues. Those spaces are treatment effectiveness problems, treatment safety problems and other problems. Each area had sub-domain. In treatment effectiveness problems the issues are no effect of drug treatment as the effect of drug treatment were not optimal with untreated manifestations or sign. In treatment safety domain the problem is adverse drug event and in domain of other problems are a problem with the cost-effectiveness of the treatment, unnecessary drug-treatment and indistinct issue/objection (further explanation vital).
The prevalence of DRPs among T2DM patients with HTN. DRPs identification and classification were based on medical judgment supported by efficient evidence-based condition management guidelines and literature. The identification of DRPs among T2DM patients with HTN was classified based on the PCNE classification system for DRPs V 8.02. During the prevalence calculation patient identified with one or more DRPs was marked one (1) and the patient without DRPs was marked zero (0). The prevalence of DRPs was referred to as the total number of DRPs among patients with T2DM and HTN admitted at KRH from January 2013 to December 2017. There was high prevalence 81.29% (313/385), most of patients 69.05% (810/1173) each had average of 2.1 DRPs (Table 3). Majority of DRPs were from treatment effectiveness problem and treatment safety problem domain respectively (270, 23.02%) and (273, 23.27%). The prevalence of DRPs (81%) among patients with T2DM and HTN was high (Figure 1).
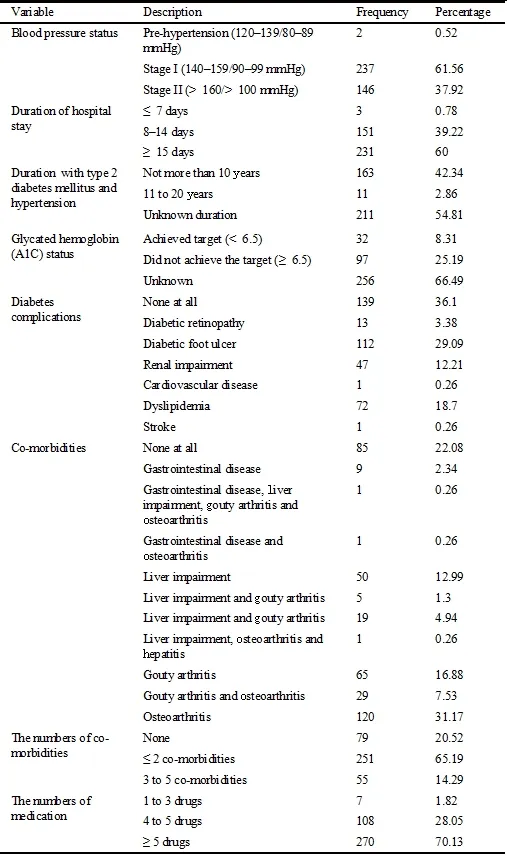
Table 2 Patient's clinical characteristics
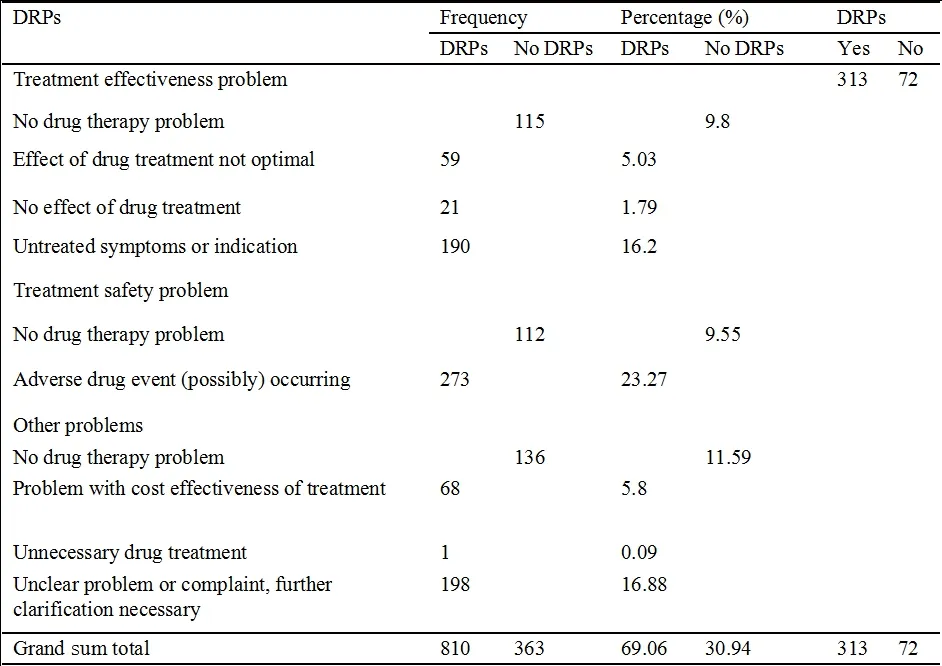
Table 3 DRPs prevalence among diabetes T2DM patients with HTN
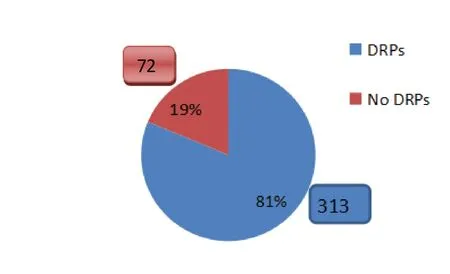
Figure 1 Prevalence of DRPs among T2DM patients with HTN
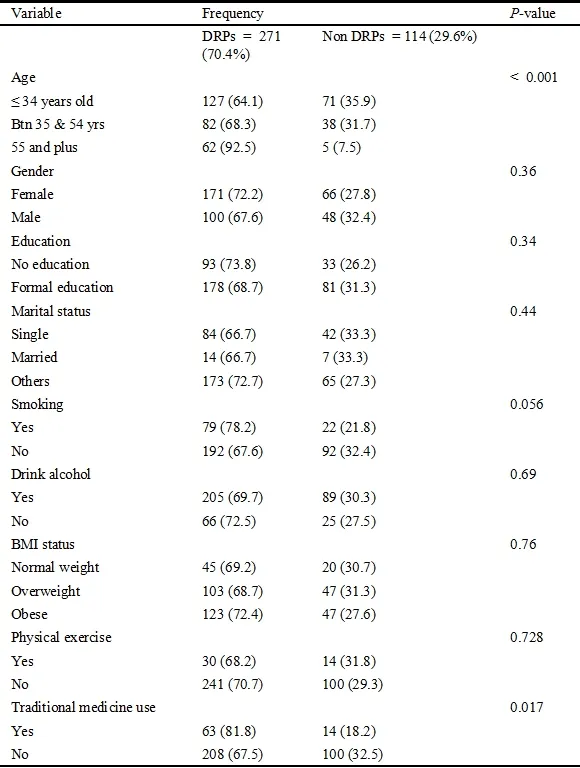
Table 4 Patient's demography bivariate analysis of the factors influencing DRPs among T2DM with HTN
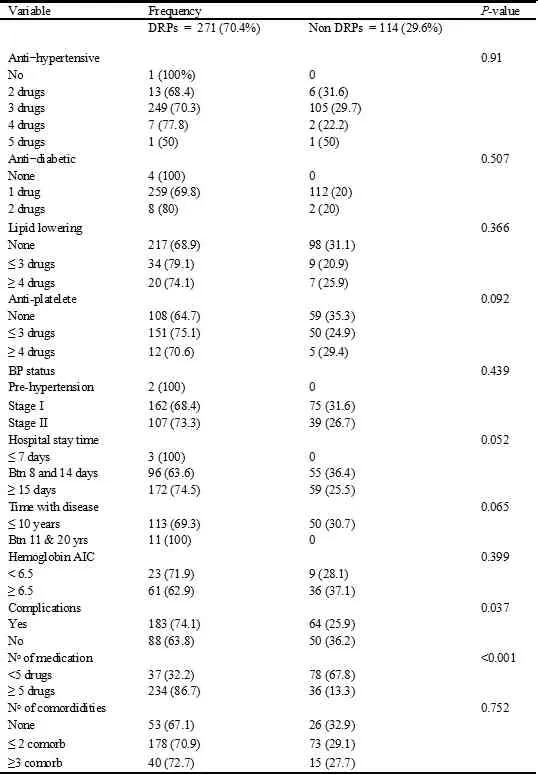
Table 5 Patient's clinical history bivariate analysis of the factors influencing DRPs among T2DM patients with HTN
The factors influencing DRPs among T2DM patients with HTN
The factors influencing DRPs among T2DM patients with HTN were established from patient demographics characteristics and clinical characteristics. The factors influencing DRPs among both conditions (T2DM and HTN) were established at the same time. The PCNE classification system for DRPs V 8.02 was used to identify DRPs. The DRPs (drug effectiveness problems, drug safety problems and other problems) were dependent variables and patient demographics characteristics and clinical characteristics were independent variables. The bivariate and multivariate analyses were performed to establish the factors influencing DRPs. The P-value less than 5 were considered as significant. The chi-square was used in bivariate analysis and logistic regression in multivariate analysis for the testing association. During multivariate analysis, unadjusted and adjusted models were used for eliminating confounding.
Study findings show that there is a statistically significant association between DRPs with age (P < 0.001) and the use of traditional medicine (P = 0.017) (Table 4), and there is a statically significant association between DRPs with patients had complications (P = 0.037), number of medication used (P < 0.001) (Table 5).
In the bivariate analysis, 4 independent variables showed an association with DRPs occurrence after running the Fisher exact test. However, in multivariate analysis advanced age, traditional medicines use, complications (having complication which was managed) and poly-pharmacy were found statistically significant associated with the occurrence of DRPs. For those aged above 55 years old were more likely to DRPs than those aged below 35 years (AOR = 1.2; P < 0.001; 95% CI: 2.6–18). Nevertheless, there was no significant association between DRPs and middle age (between 35 and 54 age of old). The patient who consumed more than or equal to 5 drugs were 2.4 more likely to develop DRPs than those who took types of drugs less than 5 (AOR = 2.4; P < 0.001; 95% CI: 1.9–3). Also traditional medicines use (AOR = 1.9; P = 0.016; 95% CI: 1.1–3.5) and having drug-related complication (AOR = 2.4; P < 0.001; 95% CI: 1.9–3) had shown significant associations (Table 6).
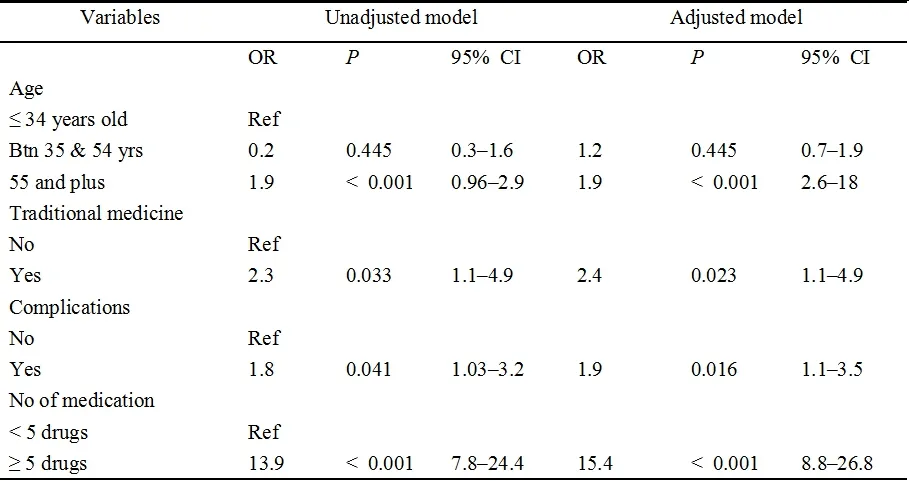
Table 6 Multivariate analysis of the associated factors of DRPs among T2DM patients with HTN

Table 7 Classifications of DRPs causes found among T2DM patients with HTN
The causes of DRPs among T2DM patient with HTN admitted at KRH
The DRPs were events or circumstances involved in drug therapy that actually or potentially interferes with desired health outcomes. Fundamentally, the issue characterized as the normal or unexpected event or condition that may not be right, in treatment with drugs. Every potential issue had a reason. The reason was the activity or absence of activity that hinted at the event of a potential or genuine issue. There may be increased potential foundations for an issue. The reason was generally the conduct that had caused the issue, and frequently that was a medical mistake. The DRPs and their potential causes were recognized from the patients' medicinal records, with an orientation to the standard rules and built up literary works. The PCNE characterization frameworks for DRPs V 8.02 were set area for deciding the reasons for DRPs. This order framework was embraced for deciding reasons for DRPs among patients with both T2DM and HTN co-morbidities. The reasons for DRPs were dictated by utilizing those instruments which were utilized in different investigations.
The DRPs causes has three main categories, the first category concerned DRPs from prescribing (drug selection 16.67%, dose selection 20.30%, and drug form selection 0.86%), the second category address DRPs arose from drug dispensing 17.6% and the third category concerned DRPs from drug use (drug use process 14.02%, patient-related 13.65% and other 17.34%). They were 1626 causes of DRPs, the most causes of DRPs were from drug use (45.01%) and prescribing (37.83%), the less contributed was dispensing (17.16%) (Table 7). The drug/dose selections (36.97%) were the main source of DRPs among T2DM patients with HTN.
Discussion
The particular specific objectives of this study were to determine the prevalence, causes of DRPs and factors influencing DRPs among diabetes mellitus type II patients with HTN at KRH. This segment offers information on the findings from the analysis of data gathered from 385 patients' files admitted between January 2013 and December 2017.
This study was in line as the PCNE classification system version 8.02 was the update version, primary ongoing investigation was utilized PCNE classification system version 5 [29, 30]. A diverse change had been produced from version 5 to version 8.02 [19]. Based on sampled size (n = 385) of this study, the sample size was higher than study done in Indonesia hospital by Zulfan et al. (n = 90), in Malaysia by Hasniza and Hoo among T2DM patient with HTN (n = 200), and by Redzuan et al. on DRPs among hypertensive patients with various co-morbidities (n = 80) . These various varieties of sample sizes may be clarified by the difference in the study setting and patient characteristics who were admitted and managed in those health facilities. A prospective study was done in Indonesia by Zulfan et al., discovered that a larger part of the patients was female (n = 52, 57.8%), which was not exactly like the findings of this study (n = 238, 61.56%). Our study was not in accordance with the study done in Malaysia by Redzuan et al. (2017) on DRPs among hypertensive patients with different co-morbidities where the primary patient was male (51.3%). This variety of sex recurrence may be expected by various settings were tended by differences in the study population. The study demonstrated the prevalence among patients with T2DM and HTN was higher in the age group under 45 years old (n = 282, 73.25%) while in the study done in Malaysia by Hasniza and Hoo, 64% were in this gathering group. The higher mean age announced might be due by that the entire population was not represented. Findings revealed that the prevalence of DRPs was 81.29% (313/385). The greater part of them every patient had an average of two DRPs (69.05%). The majority of study were not intrigued on prevalence of DRPs. They had indicated the frequency of DRPs like the study done in Malaysia by Redzuan et al. (2017), which demonstrated an expanded average of 2.15 ± 1.5 DRPs per patient. 88.8% of the patients each had one DRP. Another study done in Malaysia by Zazuli, et al. revealed averaging of 2.88 (standard deviation = 0.23) DRPs per patient. Hasniza and Hoo demonstrated that 90.5% of patient each had at least one DRP, averaging 1.9 ± 1.2 DRP. Such difference might be contributed by different tools of DRPs classification which were used, and knowledge level of health professionals about patients' care for t addressing the patient's conditions. Also, our study revealed that traditional medicines use (AOR = 1.9; P = 0.016; 95% CI: 1.1–3.5) and having drug-related complication (AOR = 2.4; P < 0.001; 95% CI: 1.9–3) had shown significant associations. Other studies did not reveal this association.
This study revealed that the patient who used more than or equal to 5 medicines were 2.4 bound to create DRPs than the individuals who took medicines less than 5 (AOR = 2.4; P < 0.001; 95% CI: 1.9-3). The prospective study was done in Malaysia by Zulfan, et al, (2017) mentioned that polypharmacy was 4.26 bound to create DRPs (r = 4.264, P = 0.039). Additionally, a retrospective study done in Malaysia by Hasniza and Hoo, (2013) was discovered that poly-pharmacy had a significant association with DRPs. These findings fail to establish other factors contributing to DRPs as equivalent to the study done in Malaysia by Zulfan, et al, which revealed respectively those different factors lipid (r = 9.840, P = 0.002), renal disability (r = 5.596, P = 0.009). This was in agreement with another study done in Malaysia by Hasniza and Hoo, 2013. This variety of variables of influencing DRPs might be contributed by patients' care level among patients with T2DM and HTN co-morbidities of this study and Malaysia. These findings had demonstrated that those patients aged over 55 years old were bound to create DRPs than those with age beneath 35 years (AOR = 1.2; P = 0.02; 95% CI: 0.2-2.3). The study done by Hasniza and Hoo was agreed with these findings where they revealed that youthful patients were protective than the old patients, the older patients had a positive factual relationship with DRPs especially on drug choice problems (P < 0.001). Accordingly, the patients who are progressed in age ought to be taken in thought as they were more defenseless than youths. This distinction of expanding of DRPs among patients with cutting edge age might be explained by sensible organ (like kidney or liver) had decreased the capacity of eliminating toxic products from digestive or circulatory or urinary systems [29, 30]. Findings indicated that they were 1626 causes of DRPs among T2DM patients with HTN. The average of 4.22 causes of DRPs per patient was high than the average of 2.37 ± 1.40 causes of DRPs revealed by the study done in Malaysia [29]. This variation in the average cause of DRPs per patient might be explained by the difference in the version of classification system tools used to determine the cause of DRP and the level of taking care of patient care. The most reasons for DRPs were from medication use (45.01%) and prescribing (37.83%), the less contributed was drug dispensing (17.16%). The different studies didn't interest classify in those main categories from DRPs causes (Adusumilli & Adepu, 2014; Hasniza & Hoo, 2013; Sonu et al., 2015; Zulfan et al., 2017). The drug/dose selection (36.97%) was the main source of DRPs among T2DM patients with HTN. This was less than drug/dose selection cause 64.67% revealed by Zulfan et al.. Another study done by Redzuan et al. revealed that drug choice (14.5%) and dosing (13.4%) were main the cause of DRPs. This variation might be due by a difference level of a health professional on pharmaceutical management for addressing patients' health conditions.
Conclusion
Since the prevalence of DRPs among patients with diabetes mellitus type II and HTN were relatively high, early detection was needed to ensure the safety and effectiveness of drug therapy as the factors influencing DRPs were identified. The cause of DRPs should be minimizing for improving patient health care.
杂志排行
Life Research的其它文章
- A meta-analysis of the treatment of cancer-related insomnia with acupuncture
- Combined music and play therapy resolves chronic toddler sleep issues: a case report
- Contrasting cognitive behavioral therapy for insomnia to analyze sleep theory in Laolao Hengyan
- A review of the treatment for insomnia in patients with cancers
- A review on the effects of sleep duration on hypertension
