毗邻颗粒链菌感染一例
2020-03-04吕漫罗洁丽张友平
吕漫?罗洁丽?张友平
【摘要】毗邻颗粒链菌可引起包括心内膜、骨髓、关节等不同部位的感染,因缺少统一的药物敏感度试验结果使其治疗变得困难。该文分析1例毗邻颗粒链菌感染患者的病例资料。该例60岁男性患者入院后病情进展迅速,出现严重心力衰竭、脓毒血症休克、MODS,经抗感染、肾脏替代治疗、呼吸机辅助通气等积极治疗仍无效,于入ICU 60 h死亡,血培养回报结果为革兰阳性球菌、毗邻颗粒链菌,确诊为毗邻颗粒链菌败血症。文献分析显示,毗邻颗粒链菌普遍对万古霉素、左氧氟沙星、克林霉素,美罗培南敏感。该文提示,毗邻颗粒链菌感染病情进展极为迅速,临床医师应加深对毗邻颗粒链菌的认识,提高对相关感染所致败血症的警惕。
【关键词】毗邻颗粒链菌;感染;药物敏感试验;败血症;诊断
Granulicatella adiacens infection: a case report Lyu Man, Luo Jieli, Zhang Youping. Puren Hospital Affiliated to Wuhan University of Science and Technology, Wuhan 430080, China
Corresponding author, Zhang Youping, E-mail: fongbaiyang@ 163. com
【Abstract】Granulicatella adiacens can cause infection in multiple sites, such as endocardium, bone marrow and joints, etc. Lack of standardized antimicrobial susceptibility test results increases the difficulty of treatment. In this article, clinical data of 1 patient with Granulicatella adiacens infection were reported. The 60-year-old male patient developed rapidly after admission and suffered from severe heart failure, septic shock and MODS. After active treatment such as anti-infection, renal replacement therapy, ventilator-assisted ventilation and other organ support therapy, the patient was still not treated and died at 60 h after admission to ICU. Blood culture result was Gram-positive cocci. The patient was diagnosed with Granulicatella adiacens septicemia. Literature review revealed that Granulicatella adiacens was generally sensitive to vancomycin, levofloxacin, clindamycin and meropenem. This case prompts that the disease progression of Granulicatella adiacens infection is extremely rapid. Clinicians should deepen their understanding of Granulicatella adiacens septicemia and enhance their cautions against infection-related bacteremia.
【Key words】Granulicatella adiacens;Infection;Drug susceptibility test;Septicemia;Diagnosis
毗邻颗粒链菌是一种营养变异链球菌(NVS)。毗邻颗粒链菌感染则是一种少见的机会性感染,在国外早有相关的病例报道,而在国内仅有个别报道。临床医师对该病的认识和重视严重不足。本文拟结合近年确诊的1例毗邻颗粒链菌感染病例及国内外相关文献综合分析,为该病的治疗提供药物选择依据。
病例资料
一、病史和体格检查
患者男,60岁。因反复胸闷、气喘半年余、再发加重伴少尿1 d于2017年5月14日从武汉科技大学附属武汉市普仁医院心内科转入ICU。患者半年前无明显诱因反复胸闷、气喘,休息后可缓解,未予重视。入院前1 d症状加重,且感少尿,遂来求诊。因入院后病情加重,转入ICU治疗。起病以来,患者神志清晰,精神差,体力下降,体质量变化不明显。患者有高血压病史1年(未服药控制血压),有头孢类药物过敏史。
入院体格检查:体温36.5 ℃,脉搏98次/分,血压96/54 mm Hg(1 mm Hg = 0.133 kPa,升压药维持),呼吸36次/分。患者烦躁不安,呼吸急促,颜面冷汗,四肢冰冷,伴全身及四肢花斑样改变,面罩给氧,SaO2 1.0,双侧瞳孔等大、等圆,直径2 mm,对光反射存在,双肺呼吸音粗,右下肺可闻及明显干性啰音及少量湿性啰音。心界扩大,节律整齐,二尖瓣区可闻及收缩期Ⅳ/Ⅵ级杂音,腹软,无压痛反跳痛,肝脾肋下未扪及,墨菲征阴性,双下肢輕度凹陷性水肿。生理反射存在,病理反射未引出。
在临床表现上,毗邻颗粒链菌感染患者多有基础心脏疾病或是中性粒细胞减少性发热,口腔黏膜炎症和中性粒细胞减少患者可能更易发生毗邻颗粒链菌感染[7]。无论何种NVS菌属,均主要表现为典型的菌血症、败血症或者感染性心内膜炎的表现。2001年Christensen等道了97例乏养球菌和颗粒链菌引起的感染,55例患者为邻颗粒链菌感染,其中IE 25例、菌血症或败血症10例;43例患者乏养球菌感染,其中IE、菌血症或败血症28例。2003年Woo等报道了9例毗邻颗粒链菌和缺陷乏养球菌感染者,9例均有基础疾病,其中4例为心血管疾病,6例为颗粒链菌血培养阳性。此外有报道颗粒性链球菌可引起中枢神经系统、关节腔、骨髓、腹膜等的感染[8-11]。
美国心脏协会和英国抗菌化学治疗学会推荐颗粒链菌和乏养球菌引起的IE在治疗上可参考肠球菌性IE方案,即苄星青霉素或氨苄青霉素联合庆大霉素;青霉素过敏者可单用万古霉素6周。目前針对NVS的治疗多数先给予经验性抗菌药物方案,再结合血培养药物敏感度试验(药敏)结果及时调整。有学者使用氨苄青霉或头孢曲松钠联合庆大霉素4 ~ 6周的治疗方案[7] 。
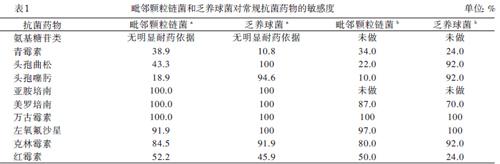
由于NVS的培养条件苛刻,目前尚无标准的药敏结果可参考。早在2000年Marion等参照2000年国际临床实验室关于青霉素在链球菌上的敏感度标准,提出颗粒链菌和乏养球菌对克林霉素、利福平、左氧氟沙星与万古霉素敏感,对庆大霉素也未见明显的耐药。现有的2项高质量的大样本研究则更为详细和深入地研究颗粒链菌和乏养球菌的药敏结果差异后也得出类似结论:颗粒链菌和乏养球菌普遍对万古霉素、左氧氟沙星、克林霉素、美罗培南敏感,其中颗粒链菌对常用抗菌药物的敏感度低于乏养球菌,见表1 [12-13]。
尽管经过积极的治疗,本文病例结局仍然不如人意,提示毗邻颗粒链菌感染危害极大,临床医师需要提高对其的认识水平。另外,该病例也值得我们进一步思考。首先,文献提示美罗培南对毗邻颗粒链菌敏感,我们给予了同样属碳青霉烯类的比阿培南联合替加环素抗菌方案。在短短的48 h抗生素治疗中,患者的炎症指标降钙素原由8.92 μg/L 降到2.74 μg/L,降幅接近60%,提示抗感染治疗有效,但患者病情仍持续进展导致死亡。究其原因,可能是患者在入院时已有严重的肝、肾、肺、脑等重要器官衰竭,已处于不可逆的终末期,虽然我们积极地给予了强力的抗感染及脏器功能支持等治疗,但患者病情仍持续进展,后期出现DIC及顽固性代谢性酸中毒、高钾血症,最终死亡。其次,尽管比阿培南对该菌的有效性是较肯定的,但现有的国内外文献中替加环素对该菌的敏感度尚无相关报道,该联合治疗方案对毗邻颗粒链菌败血症的疗效有待进一步研究明确。
总之,毗邻颗粒链菌感染病情进展迅速,危害极重,提高对该病的认识与警惕对诊断和治疗尤其重要。
参 考 文 献
[1] 游文忠. 左心房黏液瘤并发感染性心内膜炎1例. 新医学, 2010, 41(9): 622-623.
[2] 梁峰,沈珠军,方全,胡大一. 2015年欧洲心脏病学会关于感染性心内膜炎指南的解读.中华临床医师杂志(电子版),2017,11(6):975-983.
[3] Hase R, Otsuka Y, Yoshida K, Hosokawa N. Profile of infective endocarditis at a tertiary-care hospital in Japan over a 14-year period: characteristics, outcome and predictors for in-hospital mortality. Int J Infect Dis,2015,33:62-66.
[4] Téllez A, Ambrosioni J, Llopis J, Pericàs JM, Falces C, Almela M, Garcia de la Mària C, Hernandez-Meneses M, Vidal B, Sandoval E, Quintana E, Fuster D, Tolosana JM, Marco F, Moreno A, Miro JM; Hospital Clínic Infective Endocarditis Investigators. Epidemiology, clinical features, and outcome of infective endocarditis due to Abiotrophia species and Gran-ulicatella species: report of 76 cases, 2000-2015. Clin Infect Dis,2018,66(1):104-111.
[5] Akiyama T, Miyamoto H, Fukuda K, Sano N, Katagiri N, Shobuike T, Kukita A, Yamashita Y, Taniguchi H, Goto M. Development of a novel PCR method to comprehensively analyze salivary bacterial flora and its application to patients with odontogenic infections. Oral Surg Oral Med Oral Pathol Oral Radiol Endod,2010,109(5):669-676.
[6] Ratcliffe P, Fang H, Thidholm E, Bor?ng S, Westling K, ?zenci V. Comparison of MALDI-TOF MS and VITEK 2 system for laboratory diagnosis of Granulicatella and Abiotrophia species causing invasive infections. Diagn Microbiol Infect Dis,2013,77(3):216-219.
[7] Vandana KE, Mukhopadhyay C, Rau NR, Ajith V, Rajath P. Native valve endocarditis and femoral embolism due to Granulicatella adiacens: a rare case report. Braz J Infect Dis,2010,14(6):634-636.
[8] Elfessi Z, Liu E, Dukarevich Y, Caniff K, Marquez K, Shabbir Z. Sepsis induced bacterial peritonitis caused by Granulicatella adiacens. Am J Emerg Med,2019,pii: S0735-6757(19)30577-7.
[9] Patil SM, Arora N, Nilsson P, Yasar SJ, Dandachi D, Salzer WL. Native valve infective endocarditis with osteomyelitis and brain abscess caused by Granulicatella adiacens with literature review. Case Rep Infect Dis,2019,2019:4962392.
[10] Pingili C, Sterns J, Jose P. First case of prosthetic knee infection with Granulicatella adiacens in the United States. IDCases,2017,10:63-64.
[11] York J, Fisahn C, Chapman J. Vertebral osteomyelitis due to Granulicatella adiacens, a nutritionally variant streptococci. Cureus,2016,8(9):e808.
[12] Alberti MO, Hindler JA, Humphries RM. Antimicrobial susce-ptibilities of abiotrophia defectiva, Granulicatella adiacens, and granulicatella elegans. Antimicrob Agents Chemother,2015,60(3):1411-1420.
[13] Mushtaq A, Greenwood-Quaintance KE, Cole NC, Kohner PC, Ihde SM, Strand GJ, Harper LW, Virk A, Patel R. Differential antimicrobial susceptibilities of Granulicatella adiacens and abi-otrophia defectiva. Antimicrob Agents Chemother,2016,60(8):5036-5039.
(收稿日期:2019-09-18)
(本文編辑:林燕薇)
