Therapeutic efficacy and mechanism of heat-sensitive moxibustion for vascular dementia
2020-02-28WangMinchao王敏超LinLihong林丽红
Wang Min-chao (王敏超), Lin Li-hong (林丽红)
Lishui Second People’s Hospital, Zhejiang 323000, China
Abstract
Keywords: Moxibustion Therapy; Moxa Stick Moxibustion; Heat-sensitive Moxibustion; Quality of Life; Activities of Daily Living; Mental Status and Dementia Tests; Dementia, Vascular
Vascular dementia (VD) is a syndrome caused by cerebrovascular disease, with progressive cognitive dysfunction as the main clinical manifestation, may be accompanied by relevant cerebrovascular disease and neurological dysfunction[1].After the occurrence of cerebrovascular disease, the brain presents with anoxic state, which causes blood-brain barrier dysfunction,neuronal degeneration, and eventually induces VD.Study showed that 25%-41% of stroke patients developed VD symptoms within 3 months after the onset of cerebral stroke[2].In China, VD is the main type of dementia, second to Alzheimer's disease, and 0.43%-2.64% of people over 60 years old have VD[3].VD significantly reduces the quality of life (QOL) of patients,and brings heavy burden to their families and society.At present, the treatment of VD is mainly medications that promote brain metabolism, improve microcirculation and nourish the brain and nerves[4].However, the efficacy of drugs is uncertain, and the adverse reactions are obvious.
Acupuncture-moxibustion has certain therapeutic effects on VD, without obvious adverse reactions[3],while the mechanism is not completely clear.In this study, we used heat-sensitive moxibustion to treat VD,observe the clinical efficacy and explore the possible mechanism.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria in Western medicine
This study referred to the diagnostic criteria of VD in theDiagnostic and Statistical Manual of Mental Disorders-5th edition (DSM-5)[5]: cognitive deficits such as memory deterioration, aphasia, agnosia, and apraxia;cognitive deficits inducing impairment of social and professional functions; localized neurological symptoms and signs, with cerebrovascular disease confirmed by CT and other imaging examination.
1.1.2 Criteria for syndrome differentiation of traditional Chinese medicine (TCM)
Criteria for syndrome differentiation of TCM referred to the criteria of syndrome of blood stasis blocking brain in theGuiding Principles for Clinical Study of New ChineseMedicines[6].Primary manifestations:intelligence decline, stabbing headache, bluish purple lips and nails.Secondary manifestations: apathy, low spirit and rather silent, or anxious and agitated, speech confusion, slurred speech, palpitations, insomnia, a dark purple tongue or ecchymosis and petechia on the tongue, dark purple sublingual collateral vessels, deep and slow pulse or stagnant pulse.
1.2 Inclusion criteria
Those who met the above diagnostic criteria of VD in Western medicine and syndrome of blood stasis blocking brain for syndrome differentiation of TCM;duration over 3 months; aged 65-80 years; patients and their families agreed to participate in this trial and signed informed consents.
1.3 Exclusion criteria
Patients with cognitive disorder caused by Alzheimer’s disease or head trauma; those with severe diseases of heart, brain, liver or kidney; patients with mental disorder such as schizophrenia, anxiety or depression; those who were allergic to the medication;those on nootropic drugs or medications that might influence the efficacy evaluation.
1.4 Statistical method
All data were statistically analyzed by the SPSS version 20.0 statistical software.Chi-square test was applied to the comparison of counting data.Measurement data were expressed as mean ± standard deviation (±s).Paired samplet-test was applied to the comparison of intra-group data.Independent samplet-test was applied to the comparison between groups.P<0.05 was considered to indicate statistical significance.
1.5 General data
A total of 70 patients who met the inclusion criteria of vascular dementia were enrolled from our hospital between January 2017 and January 2019.All patients were randomly divided into an observation group and a control group by the random number table, with 35 cases in each group.There were no significant differences in the general data including gender, age and duration of disease between the two groups (allP>0.05), indicating that the two groups were comparable (Table 1).
2 Methods
2.1 Observation group
2.1.1 Western medicine
Oral piracetam tablets (national drug registration number: H42020389, Huazhong Pharmaceutical Co.,Ltd., China), 1.2 g/time, three times a day, for 8 consecutive weeks.
2.1.2 Heat-sensitive moxibustion
Acupoints: Baihui (GV 20), Sishencong (EX-HN 1),bilateral Xuehai (SP 10), Xuanzhong (GB 39) and Taichong (LR 4).
Methods: Acupoint locations referred to theScience of Meridians and Acupoints[7].The heat-sensitive moxibustion operation referred to theAcupoint Heat-sensitization Moxibustion:A New Moxibustion Therapy[8].The patient took a supine position, exposing the acupoints.The physician sought heat-sensitized point first, which was to apply circling moxibustion and mild moxibustion to acupoints with an ignited moxa stick 2-3 cm away from skin.When patient felt heat penetration, heat expansion, heat transmission or heat in distant area but not in local area, that would be the heat-sensitized point.Then the physician continued to perform mild moxibustion at this heat-sensitized point,with 10 min for each point.Then the physician repeated the above steps until the selected acupuncture points were completed for moxibustion in turn.It should be emphasized that when moxibustion was applied to the head acupoints, a layer of cotton cloth should be used to cover the acupoints, and then the heat-sensitized point seeking and mild moxibustion could be performed,so to prevent burning the hair.The heat-sensitive moxibustion was performed once every other day for a total of 8 weeks.
2.2 Control group
The control group only received the same medication as the observation group.The dosage, usage and the treatment course were the same as those in the observation group.
3 Observation of Curative Efficacy
3.1 Observation items
3.1.1 Mini-mental state examination (MMSE)
MMSE was scored before and after treatment in the two groups by the same neurologist not knowing about grouping[9].The total score of the MMSE scale was 30 points.The higher the score, the better the cognitive function.
3.1.2 Activities of daily living (ADL)
ADL was scored before and after treatment in the two groups by the same nurse not knowing about grouping[10].The ADL score ranged from 20 to 80 points,20 points standing for completely normal, and over 20 points indicating a varying decline of self-care ability.
3.1.3 TCM symptom score
The TCM symptoms were scored according to theSyndrome Differentiation Scale of Vascular Dementiabefore and after treatment in the two groups by the same traditional Chinese physician not knowing about grouping[11].Syndrome of blood stasis blocking brain was scored from 0 to 30 points.With a score of 7 points or higher, the syndrome diagnosis was confirmed: 7-14 points stood for mild, 15-22 points for moderate and 23-30 points for severe.
3.1.4 Levels of acetyl choline (Ach) and homocysteine(Hcy)
The fasting venous blood was collected in early morning before and after treatment.The plasma Ach levels of the two groups were measured by enzymelinked immunosorbent assay (ELISA), and the Hcy levels were measured by the enzyme cycling assay.
3.2 Criteria of curative efficacy
The improvement rate of MMSE score was used as the criteria of efficacy evaluation[12].MMSE improvement rate = (Total score of MMSE after treatment - Total score of MMSE before treatment) ÷Total score of MMSE before treatment × 100%.
Cured: The main symptoms basically disappeared.MMSE improvement rate ≥90%.
Marked effect: The main symptoms were significantly improved.MMSE improvement rate ≥60%, but <90%.
Effective: The main symptoms were improved.MMSE improvement rate ≥30%, but <60%.
Invalid: The main symptoms were not significantly improved or even worse.MMSE improvement rate<30%.
3.3 Results
3.3.1 Comparison of clinical efficacy
The total effective rate in the observation group was 91.4%, which was significantly higher than 71.4% in the control group.The difference between the groups was statistically significant (χ2=4.63,P=0.03), (Table 2).
3.3.2 Comparison of MMSE score
There was no significant difference in the MMSE score between the two groups before treatment(P>0.05).After treatment, the MMSE scores in both groups increased significantly (bothP<0.05), and the MMSE score in the observation group was significantly higher than that in the control group (P<0.05), (Table 3).
Table 3.Comparison of MMSE score between the two groups(±s, point)
Note: Compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
Group n Before treatment After treatment Observation 35 17.54±1.95 21.80±2.191)2)Control 35 17.43±1.88 19.80±1.621)
3.3.3 Comparison of ADL score
There was no significant difference in the ADL score between the two groups before treatment (P>0.05).After treatment, the ADL scores in the two groups decreased significantly (bothP<0.05), and the ADL score in the observation group was significantly different from that in the control group (P<0.05), (Table 4).
Table 4.Comparison of ADL score between the two groups(±s, point)

Table 4.Comparison of ADL score between the two groups(±s, point)
Note: Compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
Group n Before treatment After treatment Observation 35 40.06±3.02 35.78±2.401)2)Control 35 40.66±2.79 38.63±2.261)
3.3.4 Comparison of TCM symptom score
There was no significant difference in the TCM symptom score between the two groups before treatment (P>0.05).After treatment, the TCM symptom score in the observation group decreased significantly(P<0.05), and was significantly lower than that in the control group (P<0.05), (Table 5).
3.3.5 Comparison of plasma Ach and Hcy levels
There were no significant differences in the plasma Ach and Hcy levels between the two groups before treatment (bothP>0.05).After treatment, the Ach level in the observation group increased significantly (P<0.05),and the Hcy level decreased (P<0.05).The plasma Ach and Hcy levels in the observation group were significantly different from those in the control group(bothP<0.05), (Table 6).
Table 5.Comparison of TCM symptom score between the two groups (±s, point)
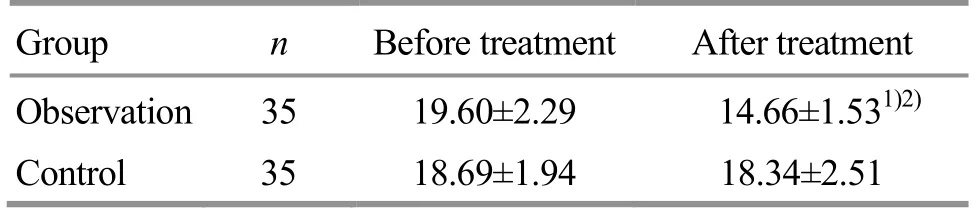
Table 5.Comparison of TCM symptom score between the two groups (±s, point)
Note: Compared with the same group before treatment, 1)P<0.05; compared with the control group after treatment, 2)P<0.05
Group n Before treatment After treatment Observation 35 19.60±2.29 14.66±1.531)2)Control 35 18.69±1.94 18.34±2.51
Table 6.Comparison of Ach and Hcy levels between the two groups (±s)

Table 6.Comparison of Ach and Hcy levels between the two groups (±s)
Note: Compared with the same group before treatment, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
Group n Ach (μg/mL)Hcy (μmol/L)Before treatment After treatment Before treatment After treatment Observation 35 66.34±10.64 79.33±8.941)2) 31.04±3.05 24.34±4.301)2)Control 35 67.24±10.05 70.64±10.30 30.75±3.38 29.70±3.99
3.3.6 Adverse reactions
During the treatment, there were no obvious abnormal changes in blood, urine, stool, liver and kidney functions, and electrocardiogram examinations of the two groups.There were 2 cases of insomnia and 1 case of anorexia in the control group.There were 2 cases of dry mouth in the observation group.The adverse reactions were minor and all self-relieved within a few days.
4 Discussion
VD is directly related to cerebrovascular diseases such as ischemic cerebral infarction, hemorrhagic cerebral infarction, and hypoxic ischemic encephalopathy.Hypertension, hyperlipidemia,abnormal blood glucose, cardiovascular disease, and heredity are all risk factors for VD[13].The pathogenesis of VD is complex and still not completely clear.It is generally considered to be related to the damage of cholinergic neural circuit system, changes of neural circuit junction-synaptic, damage of oxidative stress and free radicals, and inflammatory responses[14].With the development of molecular biology, the role of Ach and Hcy in the onset and progression of VD has been widely concerned.
Ach is one of the neurotransmitters most closely related to cognitive function and learning and memory.It has the functions of maintaining consciousness and ability of learning and memory.With cerebral ischemia and hypoxia, the process of glucose oxidative metabolism is blocked in brain, resulting in the reduction of acetyl-CoA synthesis (the raw material of Ach synthesis), leading to the decrease of Ach synthesis,which affects the ability of learning and memory, and induces the occurrence of VD[15].Study showed that cholinergic neural activity in brain tissues of VD patients decreased, and the cholinergic neural functional activity of the dorsal thalamus was significantly lower than that in the control group[16].The serum Ach level of VD patients was significantly lower than that of healthy participants, and it decreased progressively with the aggravation of the disease[17].In animal experiments,researchers found that Ach protein level in VD animal models decreased, the cholinergic receptors reduced,and the cholinergic neurons were missing[18].It is clear that there should be a close relationship between the lack of Ach synthesis and VD.
The increase of Hcy level is one of the independent risk factors of VD.The increase of Hcy level promotes the generation of oxygen free radicals and aggravates the oxidative damage of cerebral vascular endothelial cells and neurons.Hcy has neurotoxicity, and its metabolite, homocysteine, also has excitotoxic effects on hippocampal neurons, resulting in impairment of intelligence and memory function.In addition, Hcy also obstructs the metabolism of nitric oxide, and excessive nitric oxide causes neurotoxic damage[19-20].Study showed that plasma Hcy level in VD patients was significantly higher than that in the cerebral infarction group and the healthy group, and the Hcy level was positively correlated with the severity of dementia[21].Leblhuber F,et al[22]found that the serum Hcy level of VD patients was negatively correlated with MMSE score,and the Hcy level of severe dementia patients with MMSE score less than 10 points had a higher trend.
VD belongs to the category of forgetfulness,dementia or dementia disease in Chinese medicine.The location of the disease is in brain and is correlated with kidney, liver, heart and spleen.The constitutional deficiency of both qi and blood, insufficiency of kidney essence, and phlegm and static blood blocking brain orifices result in brain marrow consumption and spiritual mechanism disuse, which induces the occurrence of VD.Among them, blood stasis blocking brain is an important pathogenesis of VD.Static blood blocking brain collateral causes mind disuse and induces the occurrence of VD.VD with syndrome of blood stasis blocking brain is more common[23], and activating blood and resolving stasis, benefiting intelligence and tranquillization should be the principles of treatment.
Heat-sensitive moxibustion has the traditional moxibustion functions of warmly dredging and invigorating, which is suitable for the deficiency syndrome, cold syndrome and syndrome of qi and blood obstruction.In addition, heat-sensitive moxibustion is characterized by sensitizing acupoints with suspended moxibustion, focusing on the meridian transmission provoked by moxibustion, thereby producing more significant therapeutic efficacy than traditional moxibustion.
In this study, Baihui (GV 20), Sishencong (EX-HN 1),Xuehai (SP 10), Xuanzhong (GB 39) and Taichong (LR 4)were selected for heat-sensitive moxibustion.Baihui(GV 20) is located on the top of the head, the crossing point of the Governor Vessel and Three Yang Meridians of Hand and Foot.It has effects of resuscitating and opening the orifices, promoting yang qi to ascend, and treats mental diseases.Sishencong (EX-HN 1) has the effects of resuscitation and opening the orifices, and treating vertigo by calming endogenous wind.Xuehai(SP 10) can activate blood and resolve stasis, replenish and nourish blood, and lead blood to the channel.Xuanzhong (GB 39) is the marrow joint in the Eight Influential points.It has the effects of dispersing stagnated liver qi for relieving qi stagnation,replenishing marrow and nourishing kidney, promoting meridians and activating collaterals.It is often used in the treatment of stroke.Taichong (LR 4) is the Yuan-Primary point and Shu-Stream point of the Liver Meridian, with functions of activating qi-flow to disperse liver, dispelling stasis and relieving pain,promoting and regulating qi movement in three Jiao(triple energizers).The combination of the above five acupoints produced the effect of moving qi and activating blood, resuscitating and opening the orifices,benefiting intelligence and tranquillizing.
The results in this study showed that the effective rate of the observation group was significantly higher than that of the control group.After treatment, scores of MMSE and ADL in the observation group were significantly improved, and superior to those in the control group.The TCM symptom score in the observation group decreased significantly, while that in the control group had no significant change.The plasma Ach level in the observation group was significantly increased and the Hcy level was significantly decreased.The plasma Ach and Hcy levels in the observation group were significantly different from those in the control group.These results indicated that heat-sensitive moxibustion produced a certain efficacy in treating VD.It can significantly improve dementia symptoms, selfmanagement in daily life and TCM symptoms, which may be related to the correction of the plasma Ach and Hcy levels.
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Initiation mechanisms of acupuncture effect: a literature review of basic studies
- Manipulation parameter optimization in Liu’s back tuina therapy for kids’ cough variant asthma in remission stage
- Clinical observation of sinew-regulating bone-setting manipulations plus exercise therapy for chronic non-specific low back pain
- Observation on therapeutic efficacy of tuina plus cupping for chronic fatigue syndrome
- Clinical study on Jin’s three-needle therapy for post-stroke cognitive impairment
- Therapeutic efficacy and mechanism of heat-sensitive moxibustion for adjuvant treatment of depression in Parkinson disease