Quantitative flow ratio and intravascular ultrasound guided percutaneous coronary intervention of left anterior descending lesion concomitant with severe coronary myocardial bridge
2019-12-31XiaoQingCAIJingJINGJinWENWeiJunYINYangLIUWeiHUFeiWANGLingMAShanShanZHOUTaoZHANGFengTIANLianCHENYunDaiCHEN
Xiao-Qing CAI, Jing JING, Jin WEN, Wei-Jun YIN, Yang LIU, Wei HU, Fei WANG, Ling MA, Shan-Shan ZHOU, Tao ZHANG, Feng TIAN, Lian CHEN, Yun-Dai CHEN,#
1Department of Cardiology, the 940th Hospital of Joint Logistics Support Force of Chinese PLA, Lanzhou, China
2Department of Cardiology, the First Medical Center of Chinese PLA General Hospital, Beijing, China
3Department of Medical Service, the 940th Hospital of Joint Logistics Support Force of Chinese PLA, Lanzhou, China
4Department of Cardiology, the 305 Hospital of Chinese PLA, Beijing, China
Keywords: Coronary myocardial bridge; Intravascular ultrasound; Percutaneous coronary intervention; Quantitative flow ratio
Severe coronary stenosis concomitant with congenital coronary myocardial bridge (MB) is a tough scenario for cardiologist to perform revascularization, for which the complication rates including in-stent restenosis, stent fracture, stent thrombosis and even coronary perforation are still high.[1,2]Meanwhile, the necessity of revascularization in such patients is worth prudent evaluation. Cardiac imaging modalities are crucial and helpful in making revascularized decisions and strategies. Herein, we report a case using quantitative flow ratio (QFR) and intravascular ultrasound (IVUS) to facilitate accurate revascularization in a patient with both severe coronary stenosis and deep coronary MB.
The patient was a 66-year-old male presented with exerted chest discomfort for six months, aggravating for one month. The independent risk factors for coronary artery disease are tobacco use for more than 30 years and hyperlipidemia with low-density lipoprotein cholesterol 3.95 mmol/L. Electrocardiography showed flat and biphasic T waves in precordial V2-V4 leads, while echocardiography manifested unaffected cardiac function. Considering the typical angina during mild activity, we performed diagnostic angiography, which showed severe stenosis in proximal left anterior descending (LAD) coronary artery, followed by significant MB in mid LAD presented as milking effect, whereas mild plaques in both circumflex and right coronary artery. To evaluate the severity of the LAD stenosis, we performed quantitative coronary angiography (QCA) and calculate the lesion severity, it was found to account for 74% stenosis in lumen area with reference diameter as 3.5 mm. At the same time, in order to further evaluate the functional significance of such lesion, then we calculated the QFR value as 0.68 in distal LAD during diastolic phase, which is less than 0.80 indicating significant ischemia in LAD (Figure 1). Revascularization strategy is critical for revascularization to treat ischemia, then we performed IVUS to depict the characteristics of the LAD lesion. The pullback showed half-moon sign indicating MB in mid LAD, while focal stenosis in proximal LAD with huge plaque burden accounting for 86%, meanwhile the necrotic core in plaque indicated vulnerability of the lesion. Considering the revascularization strategy, the focal lesion in proximal LAD with clear boundary away from MB suggesting proper landing zone for stenting strategy. Meanwhile, considering the ostium of diagonal branch which set off from proximal LAD was also severely suffered, we decided to use provisional strategy to treat the bifurcation lesions. After predilating the LAD lesion using plain balloon and cutting diagonal ostium by cutting balloon, one 3.5 mm × 15 mm drug eluting stent was deployed in proximal LAD. After sufficient post dilation and another pullback of IVUS was performed, calculating the minimum lumen area (MLA) was 9.4 mm2, nearly three times of initial MLA (Figure 2). Finally, angiography revealed ideal residual stenosis accounting for less than 10% and the final QFR after the procedure was 0.94 during diastolic phase, indicating good prognosis of stent patency. To control the resting heart rate and prolong the diastolic perfusion time, the patient took both metoprolol and ivabradine. At follow-up one year after the procedure, the patient remained asymptomatic with good exercise tolerance.
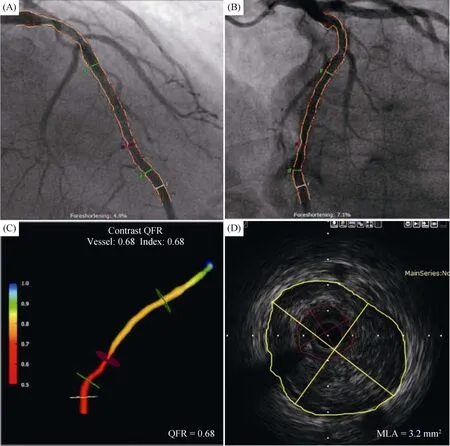
Figure 1. QFR calculation and IVUS measurement before PCI. (A & B): Two angiographic projections of LAD acquired at different angles ≥ 25° before the procedure; (C): QFR calculation based on 3-Dimensional QCA and computational fluid dynamics indicated severe ischemia; and (D): MLA measured by IVUS is 3.2 mm2, with plaque burden as 86%. IVUS: intravascular ultrasoun; LAD: left anterior descending; MLA: minimum lumen area; PCI: percutaneous coronary intervention; QCA: quantitative coronary angiography; QFR: quantitative flow ratio.
Coronary MB, which means segmental myocardium overlying epicardial coronary artery, is a congenital anomaly and traditionally recognized as a benign entity. However, clinical factors as aging, heart rate, left ventricle hypertrophy and the presence of coronary atherosclerosis may exacerbate MB and cause cardiac ischemia.[3]Meanwhile, 20 mm to 30 mm proximal to the entrance of MB were prone to suffer from atherosclerosis due to low shear stress and disturbed coronary flow.[4,5]In our case, the resting heart rate as 75 bpm and aging unmasked the ischemic symptoms. Moreover, IVUS proved that the severe atherosclerotic lesion located in proximal LAD and in close proximity to the entrance of MB is the culprit of recurrent angina.
The treatment of coronary stenosis concomitant with MB is crucial and thought-provoking. Whether medication or revascularization as the optimal treatment is difficult to decide in some scenarios. Despite advantages in assessing functional significance of coronary lesions, the use of fractional flow reserve (FFR) has been limited due to the costly pressure wire and administration of adenosine. QFR is a novel method to calculate FFR value of target vessel based on 3-Dimensional QCA and computational fluid dynamics algorithms.[6]The FAVOR Pilot and FAVORⅡChina study verified the capability of QFR to evaluate functional significance of coronary stenosis.[7,8]In our case, we calculated the QFR value prior to the procedure during diastolic phase, the value as 0.68 definitely suggested the necessity of revascularization in LAD.

Figure 2. QFR calculation and IVUS measurement after PCI. (A & B): Two angiographic projections of LAD acquired at different angles ≥ 25° before the procedure; (C): QFR calculation showed resolved ischemia in LAD during diastolic phase; and (D): MLA measured by IVUS is 9.4 mm2, with satisfied stent expansion and apposition. IVUS: intravascular ultrasoun; LAD: left anterior descending; MLA: minimum lumen area; PCI: percutaneous coronary intervention; QFR: quantitative flow ratio.
Revascularization strategy is another vital question to think over. Both coronary artery bridging graft and percutaneous coronary intervention were recommended revascularization choices in such scenario, and the latter was easier to accept by patients due to less injury. Since the in-stent restenosis rates is up to 25% at one year follow-up with drug-eluting stent extending into the MB, the ideal landing zone of stent deployment is to fully seal the culprit without entering the MB.[1]Intravascular imaging modality with high resolution is not only good at revealing the plaque characteristics, minimal lumen area, and plaque burden; but also adept at choosing stent profile and landing zone.[9]In this case, through using IVUS, we found that there was clear boundary located in proximal LAD, from which the first diagonal and septal branches sequentially taking off, between the atherosclerotic lesion and MB. Both the final IVUS pullback and QFR value showed the satisfied revascularization results and indicated good prognosis as one recent study reported.[10]The one-year follow-up verified aforementioned findings.
Acknowledgments
This study was supported by grants from National Key R&D Program of China (2016YFC1300304). The authors had no conflicts of interest to disclose.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Depression and cardiovascular diseases among Canadian older adults: a cross- sectional analysis of baseline data from the CLSA Comprehensive Cohort
- Hypoxia promotes pulmonary vascular remodeling via HIF-1α to regulate mitochondrial dynamics
- Irregular surface of carotid atherosclerotic plaque is associated with ischemic stroke: a magnetic resonance imaging study
- Pacemaker therapy in very elderly patients: survival and prognostic parameters of single center experience
- Risks of incident heart failure with preserved ejection fraction in Chinese patients hospitalized for cardiovascular diseases
- Coarctation of the aorta in twins with severe hypertension
