Transumbilical enterostomy for Hirschsprung's disease with a twostage laparoscopy-assisted pull-through procedure
2019-12-30PeiPeiXuXiaoPanChangXiZhangShuiQingChiGuoQingCaoShuaiLiDeHuaYangXiangYangLiShaoTaoTang
Pei-Pei Xu, Xiao-Pan Chang, Xi Zhang, Shui-Qing Chi, Guo-Qing Cao, Shuai Li, De-Hua Yang, Xiang-Yang Li,Shao-Tao Tang
Abstract BACKGROUND A one-stage laparoscopic operation has recently been considered a favorable option for the management of patients with Hirschsprung's disease (HD) due to its superior cosmetic results. One-stage transanal endorectal pull-through for the treatment of rectosigmoid HD has been widely used in newborns without complications. However, enterostomy is required in some HD cases for enterocolitis and dilated colon. Our transumbilical enterostomy (TUE) and twostage laparoscopy-assisted anorectoplasty were effective and achieved a similar cosmetic effect to one-stage laparoscopy on the abdominal wall in patients with anorectal malformation, but the effect in patients with HD is unclear.AIM To evaluate the safety, efficacy and cosmetic results of TUE in two-stage laparoscopy-assisted pull-through for HD.METHODS From June 2013 to June 2018, 53 patients (40 boys, 13 girls; mean age at enterostomy: 5.5 ± 2.2 mo) who underwent enterostomy and two-stage laparoscopy-assisted pull-through for HD with stoma closure were reviewed at our institution. Two enterostomy approaches were used: TUE in 24 patients, and conventional abdominal enterostomy (CAE) in 29 patients. Eleven patients with rectosigmoid HD had severe preoperative enterocolitis or a dilated colon. 26 patients had long-segment HD, and 16 patients had total colonic aganglionosis(TCA). The patients with left-sided HD underwent the two-stage laparoscopic Soave procedure, and the patients with right-sided HD and TCA underwent the laparoscopic Duhamel procedure. Demographics, enterostomy operative time,complications and cosmetic results were respectively evaluated.RESULTS There were no differences between the groups with respect to gender, age at enterostomy, weight and clinical type (P > 0.05). No conversion to open technique was required. Two patients experienced episodes of stomal mucosal prolapse in the TUE group and 1 patient in the CAE group (8.33% vs 3.45%, P >0.05). No parastomal hernia was observed in either of the two groups. Wound infection at the stoma was seen in 1 case in the TUE group, and 2 cases in the CAE group (4.17% vs 6.90%, P > 0.05). No obstruction was noted in any of the patients in the TUE group, whereas obstruction was found in 1 patient in the CAE group. Enterocolitis was observed in 3 and 5 patients in the TUE and CAE group, respectively (12.50% vs 17.24%, P > 0.05). There was no significant difference between the TUE group and CAE group in terms of the incidence of soiling and constipation (P > 0.05). The cosmetic result using the scar score in the TUE group was better than that in the CAE group (6.83 ± 0.96 vs 13.32 ± 1.57, P <0.05).CONCLUSION TUE is a safe and feasible method for the treatment of HD, and the staged enterostomy and two-stage laparoscopy-assisted pull-through achieved a similar cosmetic effect to the one-stage laparoscopic procedure.
Key words: Hirschsprung's disease; Transumbilical enterostomy; Conventional abdominal enterostomy; Laparoscopy; Pull through; Cosmetic result
INTRODUCTION
Hirschsprung's disease (HD), also known as aganglionosis, is characterized by the absence of ganglion cells in the myenteric and submucosal plexuses of the colon[1]. In 1948, Swenson first reported a staged repair by a transabdominal pull-through operation, followed by closure of the colostomy of HD[2]. Since 1980, one-stage pullthrough has been reported to be safe and effective in HD[3-5]. Primary laparoscopic pull-through for HD in infants and children was reported in mid 1990s[6,7]. In 1998,De la Torre-Mondragonet al[8]first described single-stage transanal endorectal pullthrough in the newborn, which has been widely used in the treatment of rectosigmoid HD without complications[9-12]. With the development of laparoscopy, laparoscopic procedures have been increasingly applied in various types of HD. Recently, many surgeons have accepted the one-stage laparoscopic procedure as a favorable option in the management of children with HD as it has a superior cosmetic result.
However, enterostomy is essential in some HD cases due to enterocolitis and dilated colon. The problem is that the cosmetic results of the laparoscopic approach have been reduced by the abdominal scar in some patients undergoing enterostomy.In the 1980s, Gordonet al[13]and Peteret al[14]reported the umbilical loop ostomy of HD. In 2005, Saueret al[15]described their experience with the use of the umbilicus as a site for colostomy, biopsies and surgery in 6 infants with complicated HD. It was thought that the transumbilical operation was safe and effective. We previously reported that transumbilical colostomy in a modified double-barreled fashion and the two-stage laparoscopy-assisted anorectoplasty were safe and effective in patients with anorectal malformation[16], which achieved a similar cosmetic effect to the one-stage laparoscopy. Here, we describe a surgical technique for transumbilical enterostomy(TUE) in a single-barreled fashion and the two-stage laparoscopy-assisted pullthrough of HD with stoma closure, and assess the safety, efficacy and cosmetic results of this procedure.
MATERIALS AND METHODS
Patients and methods
This study was approved by the Ethics Committee of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology. The clinical data of 53 patients (40 boys, 13 girls; mean age at enterostomy: 5.5 ± 2.2 mo) who underwent two-stage laparoscopy-assisted pull-through for HD with stoma closure were included in this retrospective study. From June 2013 to June 2018, two enterostomy approaches were used: TUE in 24 patients, and conventional abdominal enterostomy(CAE) in 29 patients. Eleven patients (TUE 4, 16.67%; CAE 7, 24.14%) with rectosigmoid HD and severe enterocolitis or a dilated colon, 26 patients (TUE 11,45.83%; CAE 15, 51.72%) with long-segment HD, and 16 patients (TUE 9, 37.50%; CAE 7, 24.14%) with total colonic aganglionosis (TCA) underwent enterostomy. Of these 53 cases, patients with left-sided HD underwent the two-stage laparoscopic Soave procedure, and patients with right-sided HD and TCA underwent the laparoscopic Duhamel procedure.
An intraoperative frozen-section biopsy and postoperative pathological examination in the definitive procedure were performed to determine the transition zone and confirm the diagnosis. The definitive surgical procedures were performed by the same surgical team at our institution.
Surgical technique for TUE
Under sufficient general anesthesia, a circumferential skin incision was made at the umbilicus. We vertically cored out the skin, subcutaneous tissue, and fascia. In neonates, we individually ligated the umbilical vessels and urachal remnant to the opening of the fascia. In other children, the umbilicus was directly cut longitudinally.After identification and exteriorization of a loop of the sigmoid colon through the opening in the fascia and peritoneum under laparoscopy, the transverse colon was directly identified through the umbilicus. In order to pull the intestine out without contamination, we pre-punctured the stomal site to reduce the intestine size due to the severely distended colon. An enterostomy was created in a single-barreled fashion with a chimney of the proximal end approximately 2 cm above the periumbilical skin.The distal end was closed and fixed to the proximal end in the abdominal cavity for easy finding next time (Figure 1).
Two-stage laparoscopy-assisted pull-through with stoma closure
Three to six months later, we closed the stoma through a peristomal skin incision. Our two-stage laparoscopic Soave procedure of left-sided HD was based on our previous reports[17,18]. We placed one 5 mm or 10 mm trocar as the working port through the stoma site, and two 3 mm trocars were respectively inserted in the right and left upper quadrant. Routinely, intraoperative frozen-section biopsy was performed before anastomosis[19]. We then used Lone Star retractors (Lone Star Medical Products,Stafford, TX, United States) to expose the anus, and electrocautery to make a circumferential incision in the rectal mucosa at 0.5-1.0 cm proximal to the dentate line.A long muscular rectal cuff was developed for > 5 cm up to the peritoneal reflection,which was then shortened to 1-2 cm. The rectal muscular cuff was partial dissected in a “V” shape at the posterior wall, and the necessary amount of the mobilized colon was dissected. A coloanal anastomosis was then performed.
The laparoscopic Duhamel procedure for right-sided HD and TCA was similar to that described previously[20]. By separating the stoma through a peristomal skin incision and mobilizing part of the bowel through the abdominal stoma opening, we were able to reach the splenic flexure. The positions of the trocars were the same as those for the laparoscopic Soave procedure for left-sided HD described above. The remaining intestines were mobilized by a laparoscopic ultrasound scalpel. In the patients with right-sided HD, the Delayer's maneuver was used to transpose the colon 270° anticlockwise, and the appendix was cut at the same time. The colon was pulled down directly in TCA. An Endo-Cutting (Johnson-Johnson Co., Ltd) Stapler was then used to facilitate extra-anal division of the rectum perpendicular to the anus, to obtain a short 3.5-4.5 cm rectal stump. Single-layer 4-0 Vicryl was used to complete the colorectal or ileorectal end-to-side anastomosis and the Endo-Cutting Stapler was used to complete the colorectal or ileorectal side-to-side anastomosis.

Figure 1 Appearance of transumbilical enterostomy.
By using 0.5% iodine and warm 0.9% normal saline while suturing, the incision was washed repeatedly. After surgery, a tube was maintained in the anus. By leaving a central open area to create a deep circular scar resembling a normal umbilicus, the umbilical wound was reconstructed with a subcutaneous purse string suture of 4-0 absorbable sutures (Figure 2). Postoperatively, total parenteral nutrition and nasogastric decompression for 24-48 h were performed in all patients, and the peristomal area was kept clean and dry. When the patients were clinically stable, they were discharged.
According to the results of a routine digital rectal examination at 2 wk postoperatively, the process of anal dilatation was achieved with Hegar dilators for 2-3 mo[17].
Statistical analysis
SPSS software version 22.0 was used to analyze the data. The Student'sttest was used to compare the demographic data and the mean scar score. All results are reported as mean ± standard deviation and percentage. Values ofP< 0.05 were considered statistically significant.
RESULTS
General characteristics and operative data during enterostomy
There were no statistically significant differences in demographics between the TUE and CAE groups, including gender, age at enterostomy, weight, and clinical type. No intraoperative complications were observed in either group. The mean operative time was not significantly different in the two groups (P= 0.381). There was no significant difference in mean blood loss and mean length of hospital stay between the two groups; no conversion to open technique was required. In 53 patients, a sigmoid colostomy (n= 11), a transverse colostomy (n= 23) or an ileostomy (n= 19) was performed (Table 1).
Complications
Two patients developed stomal mucosal prolapse in the TUE group and 1 patient in the CAE group (8.33%vs3.45%,P> 0.05). During repair of the proximal intestine in 3 patients with stomal mucosal prolapse, 2 patients with transverse colostomy in the TUE group underwent successful reoperation for TUE, and 1 patient with terminal ileostomy in the CAE group underwent reoperation for CAE. The causes of stomal mucosal prolapse in these 3 patients were proximal intestinal redundancy and frequent crying. There was no case of parastomal hernia in the two groups. Wound infection at the stoma occurred in 1 patient in the TUE group, and 2 patients in the CAE group (4.17%vs6.90%,P> 0.05). Dermatitis around the stoma was found in 4 patients in the TUE group and in 8 patients in the CAE group (16.67%vs27.59%,P>0.05). Meticulous nursing care and keeping the stoma clean decreased the pain and speeded up the recovery. Enterocolitis occurred in 8 patients, 3 patients in the TUE group and 5 patients in the CAE group (12.50%vs17.24%,P> 0.05), and treatment consisted of intravenous fluid, antibiotics, parenteral nutrition, and enemas. In the TUE group, umbilical ring narrowing, obstructive symptoms, and fecal impaction were not observed; thus, the outcome after diverting the fecal stream was satisfactory.In the CAE group, we noted obstruction after enterostomy in 1 case. One child developed adhesive intestinal obstruction on postoperative day 16, but responded well to conservative management (Table 2).

Figure 2 Appearance of the umbilicus after the two-stage laparoscopy-assisted pull-through with stoma closure.
Postoperative constipation was found in 3 patients in the TUE group and 2 patients in the CAE group (12.50%vs6.90%,P> 0.05), which steadily improved after a laxative or enema. Seven patients (4 patients in the TUE group and 3 patients in the CAE group) experienced episodes of soiling (16.67%vs10.34%,P> 0.05), which was effectively managed conservatively.
Characteristics and operative data during the pull-through procedure
At the time of two-stage laparoscopy-assisted pull-through procedure, age, sex,preoperative enteritis and operative data were not significantly different between the TUE group and CAE group. The operative time for the two-stage laparoscopic procedure in the TUE group was shorter than that in the CAE group (144.8 ± 28.2 minvs160.3 ± 27.6 min,P< 0.05) (Table 3).
Cosmetic assessment
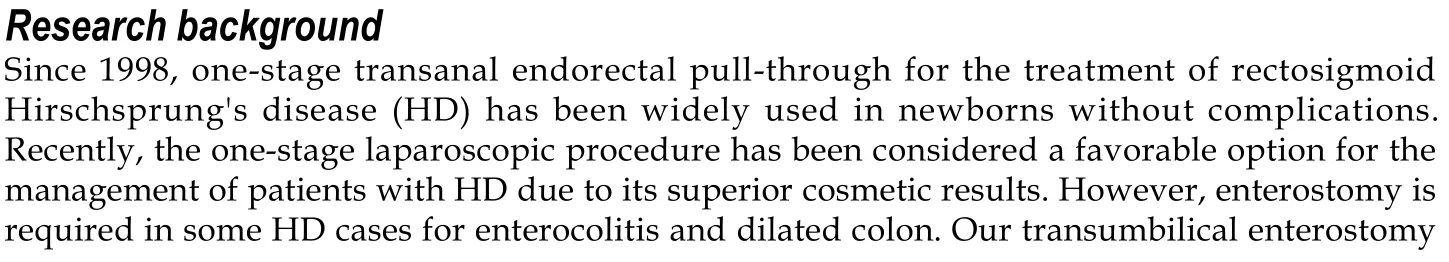
The laparoscopic-assisted two-stage pull-through procedure with simultaneous stoma closure was successfully performed in all patients, and no conversions to laparotomy were required. One year after surgery, a cosmetic assessment was conducted (Table 4). Assessment of the stoma revealed a scarless umbilicus in TUE patients (Figure 3A),and one visible abdominal scar in CAE patients (Figure 3B). The Manchester Scar Scale[18,21]was used to assess the scar score for TUE and CAE patients, and demonstrated a significant difference between the two groups (TUE: 6.83 ± 0.96vsCAE: 13.32 ± 1.57,P< 0.05).
DISCUSSION With the introduction of minimally invasive surgery, one-stage laparoscopic surgery has gradually replaced the traditional staging operation as the first choice for HD treatment[22,23]. This has the advantages of less postoperative pain and a better cosmetic result[7], but a diverting enterostomy in the normal proximal bowel is necessary in some patients with complicated HD as a life-saving procedure[24]. In recent years, the two-stage and the three-stage operation have been recommended. Although there is a debate regarding whether the two-stage operation is as safe as the three-stage operation, the two-stage operation has gained popularity in both parents and surgeons due to cost-effectiveness and no increase in postoperative complications[25].The real issue is that the scar on the abdominal wall after CAE would have reduced cosmetic results compared with the laparoscopic approach.
Inspired by pyloroplasty through a small incision at the umbilicus, some pediatric surgeons reported that TUE was safe and effective in HD[13-15]. In anorectal malformation, transumbilical colostomy and laparoscopic anorectoplasty achieved a similar cosmetic effect to one-stage laparoscopy on the abdominal wall[16]. We then began to perform TUE and two-stage laparoscopy-assisted pull-through in HD.Patients and their families were advised of the advantages and disadvantages of TUE and CAE; thus, the enterostomy procedure could be freely chosen. A retrospective study of 24 patients with TUE in our hospital, found that TUE allowed diversion of the fecal stream and enteral decompression, and did not increase postoperative complications in patients with HD compared with CAE. In addition, there was no significant difference in the length of hospital stay and the total hospital cost between the two groups. These findings indicated that TUE was a safe and effective procedure without increasing the economic burden of patients.
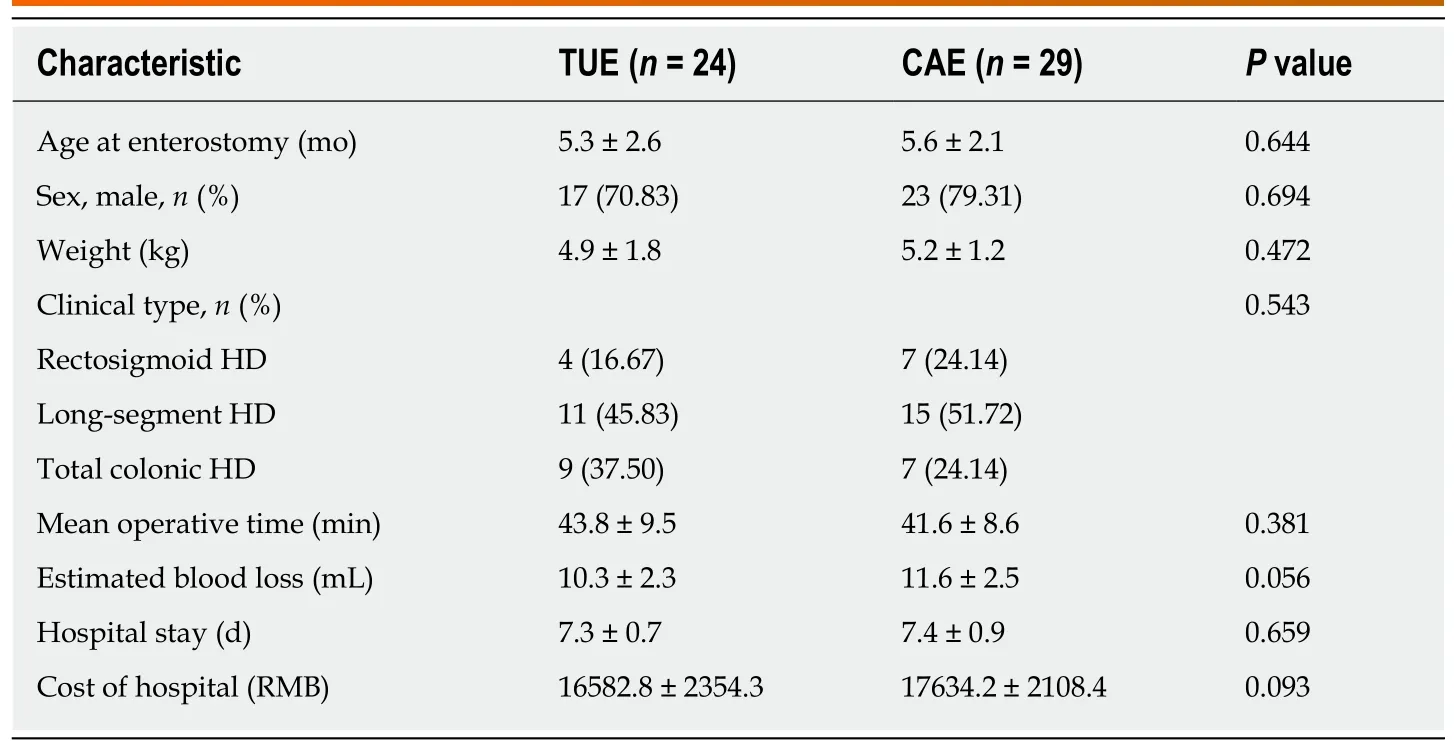
Table 1 Characteristics and operative data during enterostomy
TUE is an alternative method for patients who require enterostomy without increasing the difficulty of surgery or the incidence of postoperative complications. As reported in the literature, the ileocecum, ascending colon, transverse colon, the splenic flexure of the colon and biopsy could be easily mobilized through the umbilical incision after the umbilical stoma was separated, and converting laparoscopic total or right-sided colon resection into laparoscopic left-sided colon resection, shortened the anesthesia and operative time in TUE. However, the incision for CAE was either in the left abdomen or in the right abdomen. It is not convenient to perform these procedures in CAE. Therefore, the duration of the two-stage laparoscopic procedure for TUE was shorter than that for CAE.
This location for TUE is convenient as the stoma is on the apex of the abdominal wall, and the stoma bag is easily attached without side leakage. In the TUE group, the resulting scar after enterostomy closure closely resembled a normal umbilicus and had superior cosmetic results compared to the scar in the CAE group.
In conclusion, TUE is a safe and feasible treatment for HD. This method results in easier stoma care and better cosmetic results than CAE, and the staged laparoscopic enterostomy achieved a similar cosmetic effect to the one-stage laparoscopic procedure.
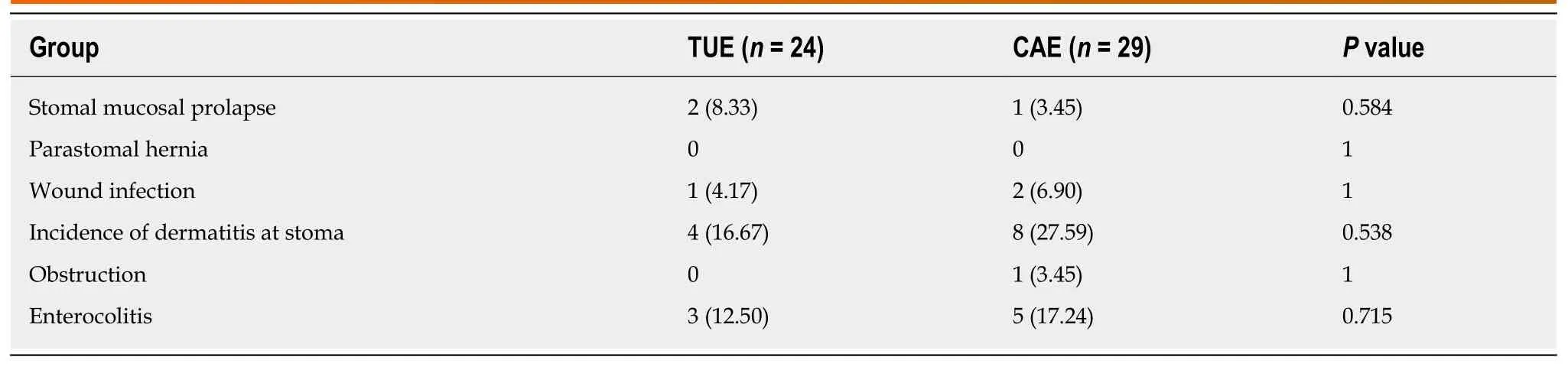
Table 2 Enterostomy-related complications, n (%)
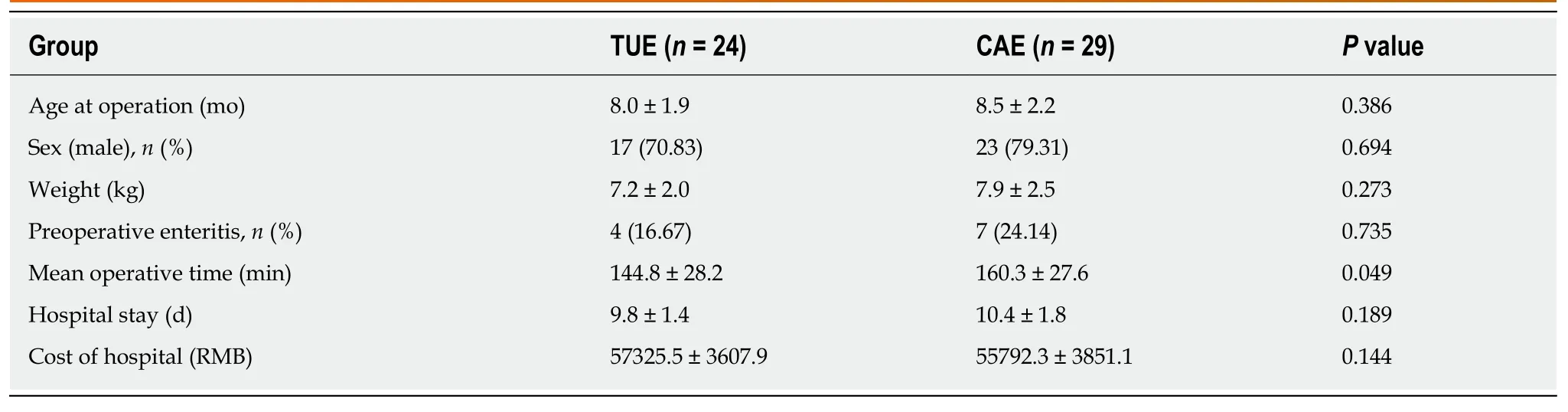
Table 3 Characteristics and operative data during pull-through procedure
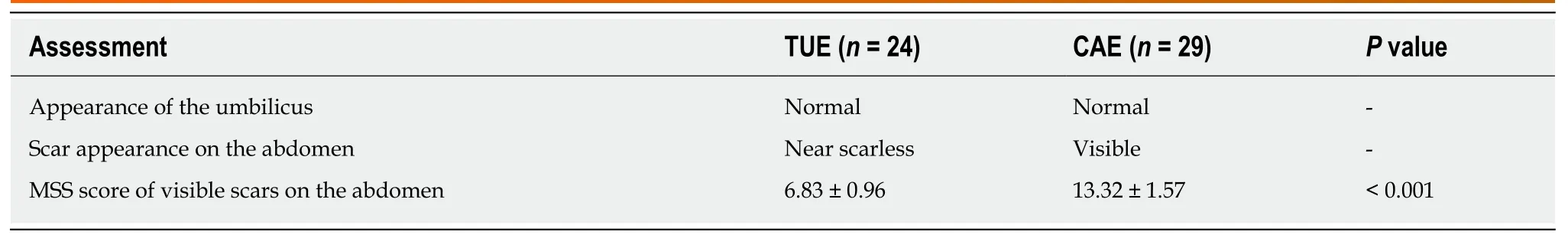
Table 4 Cosmetic assessment
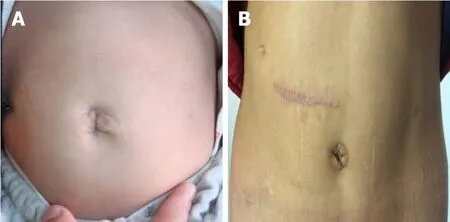
Figure 3 Appearance of the umbilicus 1 year postoperatively. A: Transumbilical enterostomy. B: Conventional abdominal enterostomy.
ARTICLE HIGHLIGHTS(TUE) and two-stage laparoscopy-assisted anorectoplasty were effective and achieved a similar cosmetic effect to the one-stage laparoscopy on the abdominal wall in patients with anorectal malformations, but the effect in patients with HD is unclear.
Research motivation
Our TUE and two-stage laparoscopy-assisted anorectoplasty were effective and achieved a similar cosmetic effect to the one-stage laparoscopy on the abdominal wall in anorectal malformations, but the effect in patients with HD is unclear.
Research objectives
This study aimed to evaluate the safety, efficacy and cosmetic results of TUE for the management of HD in a two-stage laparoscopy-assisted pull-through, and was retrospectively compared with conventional abdominal enterostomy (CAE).
Research methods
From June 2013 to June 2018, 53 patients (40 boys, 13 girls; mean age at enterostomy: 5.5 ± 2.2 mo) who underwent enterostomy and two-stage laparoscopy-assisted pull-through for HD with stoma closure were reviewed at our institution. Two enterostomy approaches were used: TUE in 24 patients and CAE in 29 patients. Eleven patients with rectosigmoid HD had severe preoperative enterocolitis or a dilated colon. 26 patients had long-segment HD, and 16 patients had total colonic aganglionosis (TCA). Patients with left-sided HD underwent the two-stage laparoscopic Soave procedure, and patients with right-sided HD and TCA underwent the laparoscopic Duhamel procedure. Demographics, operation duration, complications and cosmetic results were respectively evaluated.
Research results
There were no differences between the groups with respect to gender, age at enterostomy,weight and clinical type (P> 0.05). No conversion to open technique was required. Two patients experienced stomal mucosal prolapse in the TUE group and 1 patient in the CAE group (8.33%vs3.45%,P> 0.05). No parastomal hernia was observed in the two groups. Wound infection at the stoma was seen in 1 case in the TUE group, and 2 cases in the CAE group (4.17%vs6.90%,P> 0.05). No obstruction was found in any of the patients in the TUE group, whereas obstruction was found in 1 patient in the CAE group. Enterocolitis was observed in 3 and 5 patients in the TUE and CAE group, respectively (12.50%vs17.24%,P> 0.05). There was no significant difference between TUE group and CAE group in the incidence of soiling and constipation (P>0.05). The cosmetic result in terms of the scar score in the TUE group was better than that in the CAE group (6.83 ± 0.96vs13.32 ± 1.57,P< 0.05).
Research conclusion
TUE is a safe and feasible method for the treatment of HD, and the staged enterostomy and twostage laparoscopy-assisted pull-through procedure achieved a similar cosmetic effect to the onestage laparoscopic procedure.
Research perspectives
TUE could help patients who require enterostomy to achieve good cosmetic results in the treatment of HD using the two-stage laparoscopy-assisted pull-through with stoma closure,which is expected to be favored by patients and their families in the future.
ACKNOWLEDGEMENTS
We are grateful to Professor Ping Yin for the statistical evaluation.
杂志排行
World Journal of Gastroenterology的其它文章
- Severe liver injury due to herbal and dietary supplements and the role of liver transplantation
- Long non-coding RNA HULC as a diagnostic and prognostic marker of pancreatic cancer
- Tailored eradication vs empirical bismuth-containing quadruple therapy for first-line Helicobacter pylori eradication: A comparative,open trial
- Mesenterico-portal vein invasion should be an important factor in TNM staging for pancreatic ductal adenocarcinoma: Proposed modification of the 8th edition of the American Joint Committee on Cancer staging system
- Clinical relevance of fluorodeoxyglucose positron emission tomography/computed tomography and magnifying endoscopy with narrow band imaging in decision-making regarding the treatment strategy for esophageal squamous cell carcinoma
- Two-week bismuth-containing quadruple therapy and concomitant therapy are effective first-line treatments for Helicobacter pylori eradication: A prospective open-label randomized trial
