Long-term outcomes of hepatocellular carcinoma that underwent chemoembolization for bridging or downstaging
2019-10-19BrenoBoueriAffonsoFranciscoLeonardoGalastriJoaquimMauriciodaMottaLealFilhoFelipeNasserPriscilaMinaFalsarellaRafaelNoronhaCavalcanteMarcioDiasdeAlmeidaGuilhermeEduardoGonalvesFelgaLeonardoGuedesMoreiraValleNelsonWolosker
Breno Boueri Affonso, Francisco Leonardo Galastri, Joaquim Mauricio da Motta Leal Filho, Felipe Nasser,Priscila Mina Falsarella, Rafael Noronha Cavalcante, Marcio Dias de Almeida,Guilherme Eduardo Gonçalves Felga, Leonardo Guedes Moreira Valle, Nelson Wolosker
Abstract BACKGROUND Prospective study of 200 patients with hepatocellular carcinoma (HCC) that underwent liver transplant (LT) after drug-eluting beads transarterial chemoembolization (DEB-TACE) for downstaging versus bridging. Overall survival and tumor recurrence rates were calculated, eligibility for LT, time on the waiting list and radiological response were compared. After TACE, only patients within Milan Criteria (MC) were transplanted. More patients underwent LT in bridging group. Five-year post-transplant overall survival, recurrence-free survival has no difference between the groups. Complete response was observed more frequently in bridging group. Patients in DS group can achieve posttransplant survival and HCC recurrence-free probability, at five years, just like patients within MC in patients undergoing DEB-TACE.AIM To determine long-term outcomes of patients with HCC that underwent LT after DEB-TACE for downstaging vs bridging.METHODS Prospective cohort study of 200 patients included from April 2011 through June 2014. Bridging group included patients within MC. Downstaging group (out of MC) was divided in 5 subgroups (G1 to G5). Total tumor diameter was ≤ 8 cm for G1, 2, 3, 4 (n = 42) and was > 8 cm for G5 (n = 22). Downstaging (n = 64) and bridging (n = 136) populations were not significantly different. Overall survival and tumor recurrence rates were calculated by the Kaplan-Meier method.Additionally, eligibility for LT, time on the waiting list until LT and radiological response were compared.RESULTS After TACE, only patients within MC were transplanted. More patients underwent LT in bridging group 65.9% (P = 0.001). Downstaging population presented: higher number of nodules 2.81 (P = 0.001); larger total tumor diameter 8.09 (P = 0.001); multifocal HCC 78% (P = 0.001); more post-transplantation recurrence 25% (P = 0.02). Patients with maximal tumor diameter up to 7.05 cm were more likely to receive LT (P = 0.005). Median time on the waiting list was significantly longer in downstaging group 10.6 mo (P = 0.028). Five-year posttransplant overall survival was 73.5% in downstaging and 72.3% bridging groups(P = 0.31), and recurrence-free survival was 62.1% in downstaging and 74.8%bridging groups (P = 0.93). Radiological response: complete response was observed more frequently in bridging group (P = 0.004).CONCLUSION Tumors initially exceeding the MC down-staged after DEB-TACE, can achieve post-transplant survival and HCC recurrence-free probability, at five years, just like patients within MC in patients undergoing DEB-TACE.
Key words: Hepatocellular carcinoma; Down-staging; Liver transplantation; Local regional therapy; Bridging
INTRODUCTION
Hepatocellular carcinoma (HCC) is the sixth leading cause of cancer and the third leading cause of cancer death worldwide. It is the number one oncologic cause of death in cirrhotic patients, with approximately one million deaths/year[1,2]. According to the Barcelona Clinic Liver Cancer (BCLC) staging classification, liver resection (LR),radiofrequency ablation (RFA), and liver transplantation (LT) are potentially curative treatments for HCC[3,4].
LT is a well-established modality for curative treatment of HCC because it removes the tumor, while excluding the cirrhotic environment, which could lead to the emergence of new malignant lesions[5]. Success rates of LT as a curative treatment are attributed to improved candidate selection using restrictive criteria based on number and tumor size, among which the most frequently used is the Milan criteria (MC)[6]. In centers that frequently perform LT, the 5-year post-transplant patient survival can achieve 75%-80%[7].
According to the BCLC, transarterial chemoembolization (TACE) is indicated as palliative treatment in patients with intermediate HCC (BCLC B). However, over the last several years, TACE has being indicated as downstaging (reduction in the size of tumor using locoregional therapies (LRT) in selected patients to meet acceptable criteria for LT)[7,8]and bridging (neo-adjuvant therapy attempt to avoid HCC growth while the patient is waiting for transplantation)[9]. Nevertheless, there is a lack of consistent data on radiological response, overall and recurrence-free survival after transplantation in this heterogeneous group of patients.
Drug-eluting beads (DEB-TACE) is a technology that has been developed to enhance tumor drug delivery and reduce systemic availability and toxicity. DEBTACE loaded with doxorubicin is a safe and effective palliative treatment for HCC and offers clinical benefit to patients with more advanced disease[10]. Another benefit of this technology is that it allows for standardization of the chemoembolization technique, since it is possible to estimate the amount of drug delivered to each tumor.The purpose of this study was to compare the long-term outcomes of patients that underwent LT after DEB-TACE for downstaging versus bridging. Also, we aimed to investigate radiological tumor response after the first DEB-TACE session in both groups.
MATERIALS AND METHODS
This study was a single-institution, prospective, cohort study, conducted at the Department of Interventional Radiology and approved by the research ethics committee (SGPP155711/CEP11/1704-CAAE0199.0.028.000-11). All patients signed an informed consent form and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki.
Patients
The present study included 200 consecutive patients with HCC, from April 1, 2011 to June 30, 2014, who underwent DEB-TACE at our institution using the outpatient treatment protocol previously described[11]. These patients were part of the liver transplant program and were divided into two groups: Bridging and downstaging(Figure 1). At that time, precise criteria for HCC downstaging related to the sum of the maximal tumor diameters were unclear; therefore, we included in the downstaging group all patients out of the MC[6], without vascular invasion based on cross-sectional magnetic resonance imaging (MRI) or computed tomography (CT) and without lymph node involvement by tumor or extra-hepatic tumor spread. Consistent with Yaoet al[8], we classified the downstaging patients into 5 groups, as summarized in Table 1. It was identified a subgroup never before described, Group 4 which has a low tumor volume (less than 8 cm) but with 2 or 3 lesions above 5 cm. Patients who were within MC[6]or T2 of the United Network for Organs Sharing were classified as bridging group (Table 1) and were divided into 3 groups, Group 1 = one tumor;Group 2 = two tumors; and Group 3 = three tumors.
Diagnostic imaging
All patients underwent multiphasic abdomen CT (Aquilion One 320, Toshiba, Tokyo,Japan, Aquillon 64, Toshiba, Tokyo, Japan-Aquilion Vision 640 Toshiba, Tokyo, Japan)or MRI (GE 2 HDXT-1.5T, General Electric, Boston, Massachusetts, United States and Siemens Espree-1.5T, Siemens AG, Berlin, Germany). The overwhelming majority of the imaging examinations were performed with MRI. All images were acquired using the following parameters: 120kV voltage; tube current (sure exposure 3D SD 10.00,Max 500 Min 100 mAs, reconstruction slice thickness: 1 or 3 mm - depending on the acquired sequence). Patients submitted to abdominal CT received an intravenous bolus injection of 1.7 mL of contrast/kg body weight of the non-ionic iodinated contrast agent Henetix®350mg I/mL, Guerbet-Rio de Janeiro, Brazil (350 mg I/mL Iobitridol). Patients who underwent abdominal MRI received intravenous bolus injection of 0.2 mL/kg patient weight of the paramagnetic contrast agent Magnevistam®, Bayer-Leverkusen, Germany (469 mg/mL Dimeglumine Gadopentetate), both with injection rate of 3 to 4 mL/s. HCC diagnosis for a lesion ≥ 1 cm was based on either CT or MRI demonstrating arterial phase enhancement and washout during the delayed images, according to the American Association for the Study of Liver Diseases guidelines[12,13]. Hepatic nodules < 1 cm were not counted as HCC. Percutaneous biopsy was not routinely performed.
Eligibility
Criteria for downstaging failure and exclusion from liver transplant are summarized in Table 1. There was no time limit or DEB-TACE session limit for completing downstaging. Eligibility for LT and time on the waiting list until LT were compared between the downstaging and bridging groups.
DEB-TACE protocol
DEB-TACE protocol was previously described by Nasseret al[11]and Cavalcanteet al[14]. Briefly, DEB-TACE procedures were performed under local anesthesia with lidocaine 2%, sedation and analgesia, with venous administration of midazolam and fentanyl.
Using a unilateral femoral artery approach, diagnostic angiograms of the superior mesenteric, celiac trunk, and common hepatic artery were performed with the purpose of outlining the hepatic artery anatomy, delineate the tumor, identify its feeding vessels, and evaluate portal vein patency. In each DEB-TACE session, feeding vessels were catheterized with a 2.8F microcatheter (Progreat, Terumo, Japan), and embolization of the tumors was performed with injection of iodinated contrast medium mixed with one vial of DC-BEAD 100-300μm (Biocompatibles, United Kingdom) or HepaSphere 50-100 μm (Merit Medical Systems, United States) loaded with 50 mg of Doxorubicin. If the endpoint was not achieved after the injection of loaded beads, additional bland beads (Beadblock, Biocompatibles, United Kingdom or Contour, Boston, United States) were injected until the endpoint (complete stasis) was reached. For patients with more than one tumor, DEB-TACE began by the largest nodule to reach the smallest tumor, regardless of how many sessions were required[11].Vascular lake phenomenon was defined as a localized pooling of contrast media within the tumor, which persists in the venous phase of angiography, resembling extravasation[14].
Radiological response
Tumor response was assessed through imaging studies (contrast-enhanced MRI or multiphasic abdomen CT) and performed 30-45 d after DEB-TACE, according to the modified response evaluation criteria in solid tumors (mRECIST) guidelines[15], as follows: (1) Target lesion response: response of the treated nodules was evaluated by comparing the baseline sum of diameters of target lesions before DEB-TACE with the sum of diameters of viable target lesions after DEB-TACE in each patient; (2)Complete response (CR) was defined as disappearance of any intra-tumoral enhancement in all target lesions; Partial response (PR) was defined as at least a 30%decrease in the sum of diameters of viable target lesions; Stable disease (SD) was defined as any case that does not qualify for either PR or progressive disease; Disease progression was defined as an increase of at least 20% in the sum of the diameters of viable target lesions; (3) Objective response (OR) rate was defined as the sum of CR and PR.
Survival
Five-year post-transplant overall survival and recurrence-free survival were evaluated and compared between the two groups.
Statistical analysis
Statistical analysis was performed with SPSS version 15.0 (IBM, Armonk, NY, United States). Quantitative characteristics were described by group (bridging and downstaging) before and after transplantation using summary measures (mean,standard deviation, median, minimum and maximum) and compared with Student'st-tests or Mann-Whitney tests. Qualitative characteristics were described by group(bridging and downstaging) before and after transplantation. Associations were tested with chi-square tests or exact tests (Fisher's exact test or likelihood ratio test).Overall survival and recurrence-free survival were estimated using bivariate Cox regression and multivariate Cox regression to verify the influence of significant characteristics on survival. Overall survival and recurrence-free survival were evaluated, by group, using the Kaplan-Meier method. Receiver operating characteristic (ROC) curve was generated to identify maximal tumor diameter most associated with liver transplant in the downstaging group.Pvalue of 0.05 or less was considered significant.
RESULTS
Baseline characteristics
A total of 200 patients were enrolled during the inclusion period: 64 in downstaging group and 136 in bridging group. Three patients could not perform DEB-TACE and were excluded. Two patients were excluded as a result of hepatic artery dissection during the procedure. One patient was excluded because she presented with respiratory failure after sedation and the procedure was interrupted before embolization (Figure 1).
The groups did not significantly differ in terms of age, gender, etiology of liver disease, Child score, or baseline alpha-fetoprotein levels. At presentation, the downstaging population presented a greater number of nodules, median of 2.81 nodulesvs1.47 (P= 0.001); increased total tumor diameter 8.09vs3.73 (P= 0.001);increased multifocal HCC 78%vs34.6% of samples (P= 0.001); and increased vascular lake phenomenon 34.3%vs12.5% (P= 0.001) (Table 2).
Eligibility for transplantation
Several variables that would increase the chance of the individual undergoing transplant were evaluated to identify LT predictors. Patients with coagulopathy (RNI> 1.2) and thrombocytopenia (platelet count < 150.000/mm3)[16,17]were more likely to be transplanted (Table 3). After TACE, only patients within MC were transplanted.More patients underwent LT in the bridging group than in downstaging (65.9%vs33.9%,P= 0.001) (Tables 3 and 4). Among the downstaging patients, G4 demonstrated the best eligibility for orthotopic liver transplantation (OLT) (60%) and did not have any cases of HCC recurrence (Table 4).
Median time on the waiting list for LT (interval between the first DEB-TACE to LT)in the downstaging group was significantly longer 10.6 months (range, 1.7 to 20.1 mo)than in the bridging group 6.6 mo (range, 0.6 to 30.5 mo) (P= 0.028) (Table 5). ROC curve analysis revealed that patients with maximal tumor diameter up to 7.05 cm were more likely to receive LT during DEB-TACE (P= 0.005) than patients with maximal tumor diameter more than 7.05, with sensitivity of 65.9% and specificity of 71.4% (Figure 2).
Radiological response
CR was observed more frequently in bridging than in downstaging group (P= 0.004).However, since PR occurred more often in the downstaging group, there was no statistically significant difference in OR between groups (P= 0.105) (Table 6). Six patients from the bridging group were submitted to LT after the first DEB-TACE procedure, thereby occurring before the imaging study (less than 30 d after DEBTACE).
Recurrence and survival
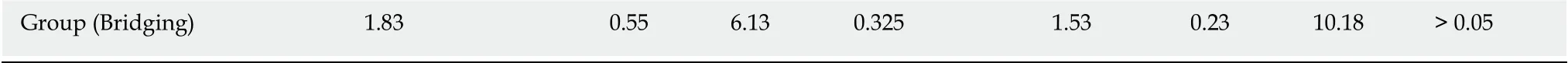
Overall survival and recurrence-free survival were estimated using bivariate Cox regression and multivariate Cox regression to verify the influence of baseline characteristics (age, gender, etiology, CHILD score, MELD, alpha-fetoprotein, number of nodules, maximal tumor diameter) on survival. There was no influence of baseline characteristics (P> 0.05), and/or between groups (bridging versus downstaging) on overall survival (P= 0.662) (Table 7) or recurrence-free survival (P= 0.874) (Table 8).
In an intragroup analysis, there was no statistical difference between overall survival (P= 0.955) and recurrence-free survival (P= 0.955) observed in subgroups 1,2, and 3 of the bridging group. However, in the downstaging group, it seems that subgroup 3 had worse overall survival (P= 0.04) and worse recurrence-free survival(P= 0.027), compared to the other subgroups (Table 4). Post-transplantation recurrence occurred more frequently in the downstaging group 25% (5/20) than in the bridging group 5.81% (5/86) (P= 0.020); however, these events did not significantly affect recurrence-free survival (P= 0.874).
Kaplan-Meier’s 1, 3, and 5-year post-transplant overall survival probability were 95%, 88.2%, 73.5% in the downstaging group, and 82.8%, 76.5%, 72.3% in the bridging group (P= 0.317), respectively (Figure 3). Median overall survival was 1150 d or 3.15 years (SD = 1.33, range from 0.52 to 5.07) in the downstaging group, and 1083 d or 2.97 years (SD = 1.66, range from 0 to 5.77) in bridging group. Kaplan-Meier’s 1, 3, and 5-year post-transplant recurrence-free survival probability were 95%, 82.8%, 62.1% in the downstaging group, and 80.2%, 76.5%, 74.8% in the bridging group (P= 0.935),respectively (Figure 4). Recurrence-free survival was 1104 d or 3.02 years (SD = 1.37,range from 0.34 to 5.07) in downstaging group, and 1070 days or 2.93 years (SD = 1.69,range from 0 to 5.77) in bridging group (Table 6).
DISCUSSION
The best approach to patients with HCC beyond MC is controversial given the scarcity of available organs for transplantation and the impreciseness of identifying patients who are most likely to benefit from LT. In 2010, downstaging of HCC has been identified as a priority for research in the field of LT[18]. Since that time, we have not found in the literature many published data evaluating this controversial subject.
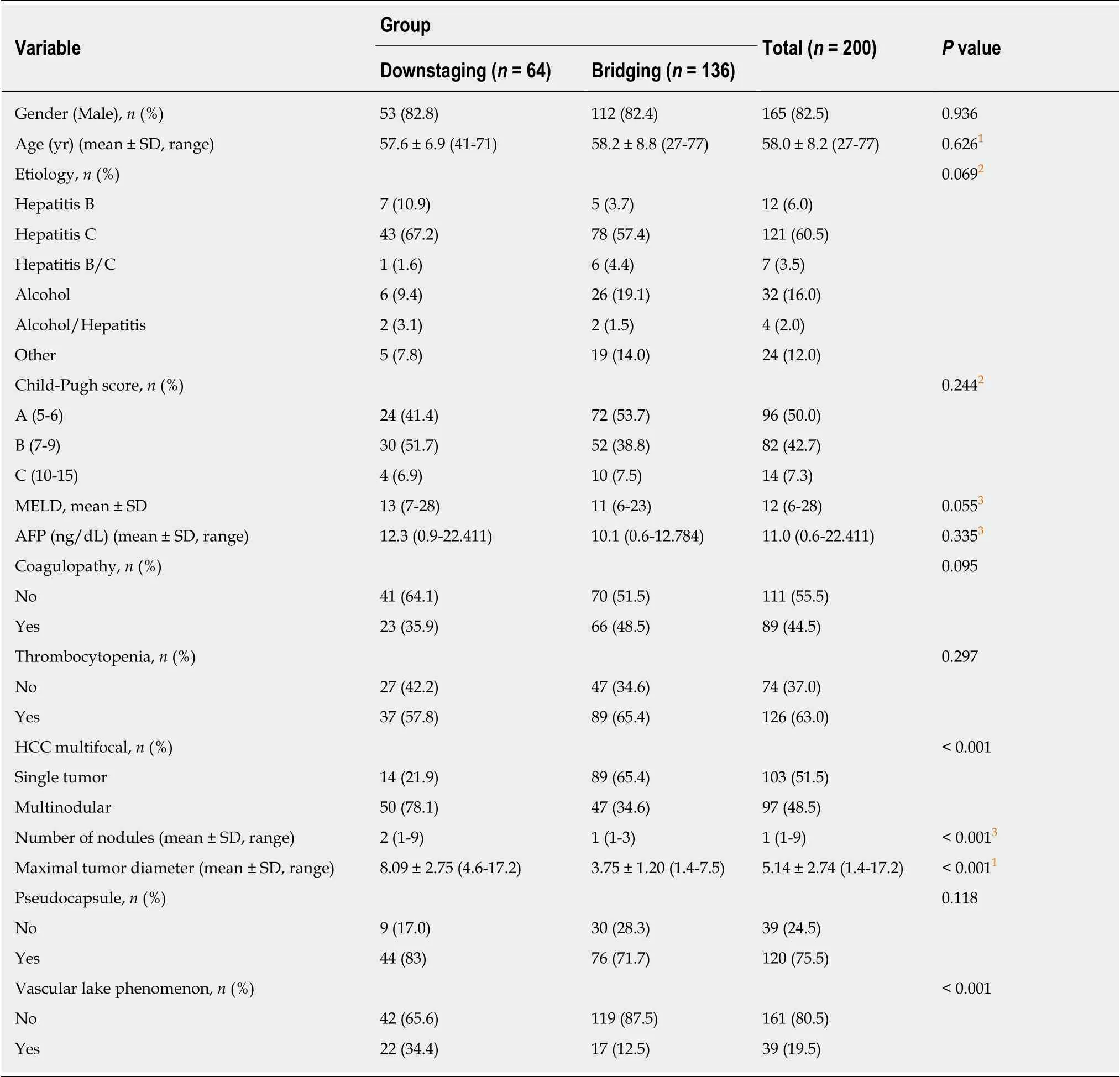
Table 2 Patients demographics
The majority of papers is limited by small sample size, short duration of follow-up,and absence of a comparison group[7-9,19-24]. Most studies have used MC as the endpoint for downstaging[9,19,22-24]. There appears to persist a doubt if patients beyond MC should undergo LT after successful downstaging. There is a lack of information in the literature regarding long-term overall and recurrence-free survival in these patients[25].
The current understanding regarding neo-adjuvant treatment for HCC is that it would be most appropriate for: Controlling HCC progression for expected long waiting times (bridging), identifying patients with different probabilities of cancer progression (selection criterion), and reducing tumors sizes to meet acceptable criteria for LT (downstaging)[26]. However, there is no strong evidence that neo-adjuvant treatments should be applied if the expected waiting time for LT is shorter than 6 mo[25-27].
The present study included patients that have used neo-adjuvant therapy, DEBTACE loaded with Doxorubicin, for HCC patients undergoing bridging and downstaging. Patients fulfilling the MC were immediately included on the waiting list for LT, whereas patients beyond MC were listed only after they met MC, regardless ofhow many DEB-TACE sessions. Few studies followed the same protocol: none exclusively using DEB-TACE and the majority using many different kinds of LRT[19,20,22]. Graziadei et al[19], used conventional TACE (cTACE) for both groups:patients fulfilling the MC were started immediately after listing for OLT and patients beyond MC were included on the waiting list after showing response to the first TACE. Ravaioli et al[20], used many kinds of LRT, such as LR, percutaneous ethanol injection (PEI), RFA, and cTACE for both groups. Additionally, patients fulfilling the MC were listed immediately for LT and patients beyond MC were listed after completing the pre-established downstaging protocol. De Luna et al., employed transcatheter arterial chemoinfusion for both groups. Patients fulfilling the MC were listed immediately for OLT and patients beyond MC were included on the waiting list after reaching MC (downstaged)[22].
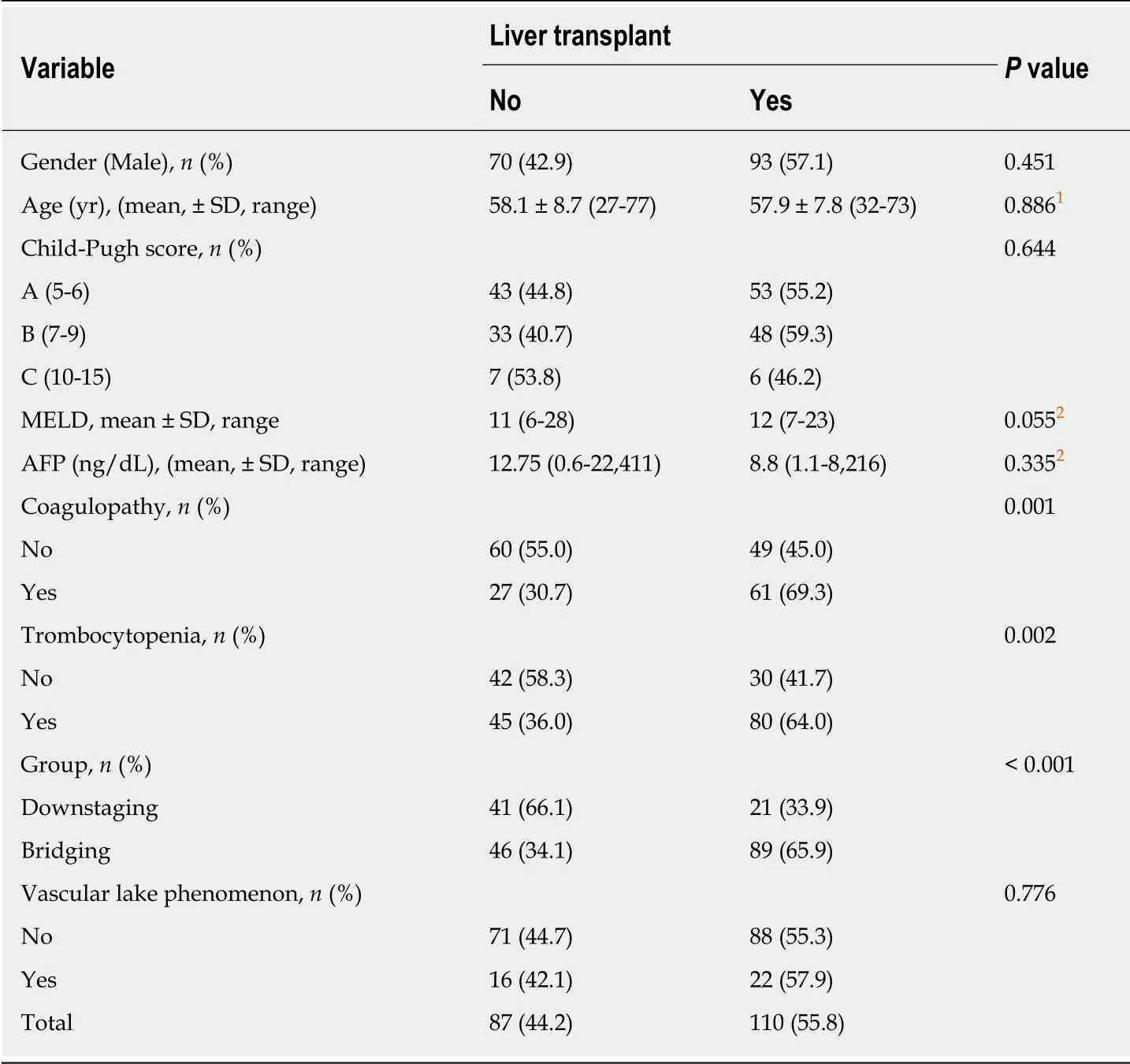
Table 3 Bivariate analysis of liver transplant predictors
Few studies have used LRT in patients beyond MC in order to achieve downstaging[7-9,21,23,24]. Some studies compared their results with other LRT, such as transarterial radioembolization[9]; some studies did not compare between groups[8,9,21,23,24]; and other studies used patients within the MC on the waiting list for LT as a comparative group[7]. Among these, the most significant study, highlighted by the sample and methodology, was published recently by Yao et al[7]. In a prospective cohort, the authors reported the outcomes of 118 patients (largest study group)exceeding the MC that underwent LRT (cTACE, RFA, and PEI) in a downstaging well-established protocol with the intent for LT and compared to 488 patients within the MC on presentation[7].
In the present study, at the presentation, the two populations did not have significantly different baseline demographic characteristics. Vascular lake phenomenon was much more frequent in downstaging population 34.3% (P = 0.001),perhaps since vascular lake phenomenon occurs more frequently in tumor of size ≥3.0 cm[14].
More patients underwent LT in the bridging group (66%) compared to the downstaging group (34%, P = 0.001). In the literature, eligibility for LT reported for the bridging group ranges from 68% to 85.4%[19,20,22]. Yao et al[7], reported 68% eligibilityfor LT in the MC group, similarly seen in our study. In a recent study, a dropout rate of 2.58% due to tumor progression was observed in patients who received bridging LRT, while the rate among patients who did not receive LTR was 8.18% (P = 0.01)[28].Among downstaging patients, neo-adjuvant success rates regarding eligibility for LT widely vary from 11% to more than 70%[29]. This large range reflects the heterogeneity of the criteria used to include patients in a downstaging protocol, differences in the LTR protocol itself, and several different criteria used worldwide on when to include a patient on a transplant list.
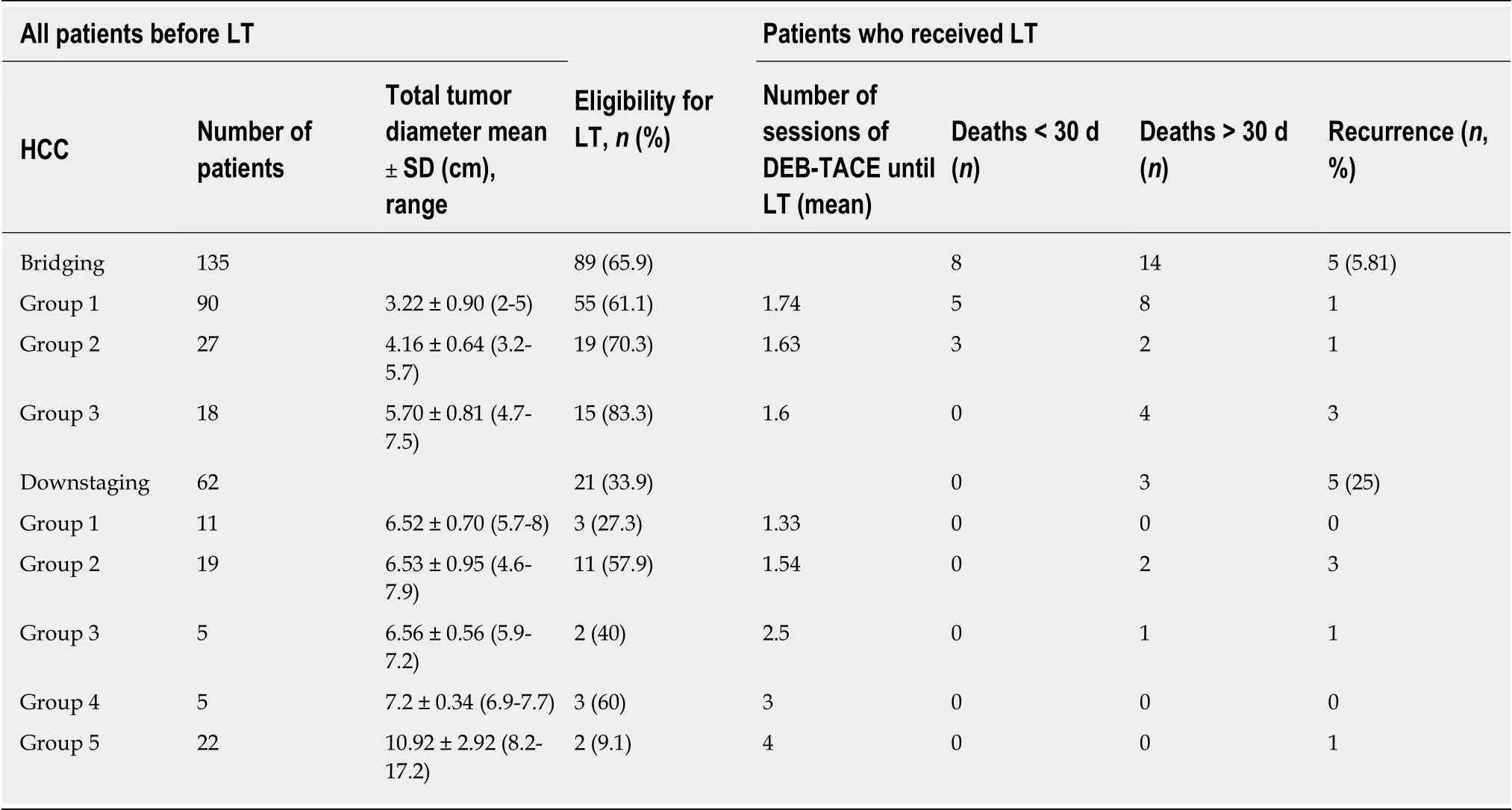
Table 4 Subgroup analysis
In the downstaging protocol, it was included patients with maximal tumor diameter ≤ 8 cm (G1, G2, G3, and G4) and > 8 cm (G5). In this way, eligibility for LT was 34%. However, if we closely look at eligibility for LT in subgroups with maximal tumor diameter up to 8 cm, eligibility for LT would be 47.5%, closer to Yao et al[7]’s reported eligibility of 54%. Maximal tumor diameter appears to influence success of HCC downstaging due to eligibility for LT, so much so that Yao et al[7], limit maximal tumor diameter to 8 cm in their downstaging protocol.
In the present study, G1, G2, and G3 used the same criteria described by Yao et al[7].Nevertheless, we found a new group of patients with maximal tumor diameter ≤ 8 cm(G4 = 2 or 3 lesions at least one > 5 cm with the sum of the maximal tumor diameters≤ 8 cm), not previously described. Among patients in the downstaging group, we sought to verify if there was a cutoff limit that related to maximal tumor diameter,and a better chance for the patient to be submitted to LT. We found that patients in the downstaging group with maximal tumor diameter up to 7.05 cm had a greater chance of LT (P = 0.005). Contrary to this finding, G4, with a mean maximal tumor diameter of 7.2 cm, had the best eligibility for LT (60%). On the other hand,corroborating Yao et al[7]’s impression, G5, where the maximal tumor diameter was 10.9 cm on average, had the worst eligibility for LT (2 patients of 22; 9.1%). Other variables that were implicated with a greater chance of LT were coagulopathy,thrombocytopenia, and belonging to the bridging group.
Studies provided a cautionary note with an anticipated higher recurrence rate post LT: the further the tumor burden is beyond the MC (the Metro ticket concept)[25,30]. In our study, post LT recurrence occurred more frequently in the downstaging group 25% (5/20) compared to the bridging group 5.81% (5/86) (P = 0.02); however, this finding did not interfere with recurrence-free survival (P = 0.874). Group 4 did not have a case of HCC recurrence. In the downstaging group, HCC recurrence rate was higher than Yao et al[7]’s rate (7.5%), but similar to Ravaioli et al[20]’s rate (18%).
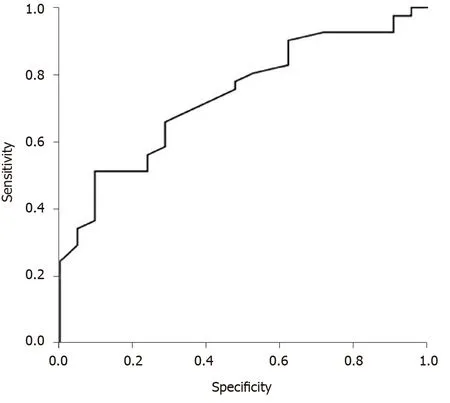
Figure 2 Receiver operating characteristic curve analysis revealed that in the downstaging group, patients with maximal tumor diameter up to 7.05 cm are more likely to receive orthotopic liver transplant during drugeluting bead trans-arterial chemoembolization (P = 0.005).
Our results suggest that patients, with tumors initially exceeding the MC downstaged after DEB-TACE, can achieve post-transplant survival and HCC recurrencefree probability, at five years, just like patients within MC. And, that most patients who have a total tumor diameter less than 7.0 cm will require up to 2 sessions of DEBTACE to reach downstaging and/or to be transplanted. Patients with total tumor diameter greater than 7.0 cm will require 2.5 or more sessions. As far as we know, this study is the only one in the literature that compares long-term results between two cohorts (downstaging and bridging) that used DEB-TACE with doxorubicin exclusively as LRT[25]. No baseline characteristic, including AFP levels, served as a predictor of poor overall or recurrence-free survival after LT.
There is no evidence that one type of LRT is clearly superior to another, but TACE,especially cTACE, is the most frequently one used[26,31]. In HCC, a temporary overproduction of vascular endothelial growth factor (VEGF) is caused by a single session of TACE. And an increase in serum VEGF is related to tumor growth via neoangiogenesis, metastatic seeding, and cancer cell migration and survival[32].Lipiodol emulsion, used in cTACE, causes unstable ischemia with reperfusion injury in the targeted tissue[32]. On the other hand, the beads used in DEB-TACE lead to irreversible permanent embolization and ischemia[33]. Schicho et al[32], compared cTACE with DEB-TACE, finding that VEGF plasma levels were significantly higher in cTACE patients as soon as 24 h after treatment (P = 0.01) and remained at high levels 28 d after cTACE (P = 0.03), compared to DEB-TACE patients. Thus, perhaps DEBTACE should be preferentially used when TACE is the LRT option that is considered.We found one paper in the literature that uses DEB-TACE with doxorubicin for downstaging, but the study did not include a comparative group[24].
Response to TACE as a selection criterion is promptly identifiable in clinical practice and may reflect biological properties, such as tumor aggressiveness[34]. There is an excellent correlation between pathologic degree of tumor necrosis post LRT found in MRI using mRECIST criteria and explant pathology[35]. In the present study,we verified that there was an association between degree of response in both groups after first DEB-TACE (P = 0.004). The bridging group presented with more CR events and less PR events than the downstaging group. However, the OR rate was not statistically significant different between the two groups (P = 0.105).
We recognize that the subgroup analysis is strongly limited by the low number of patients included in each subgroup but the absence of difference between groups in the final outcome shows the equivalence of results by the technique employed.Successful downstaging of HCC to within MC with DEB-TACE loaded with doxorubicin was associated with a lower rate of LT and four times more HCC recurrence than the bridging group. Despite this finding, both groups had comparable post-transplant survival and recurrence-free probabilities. OR did not differ between groups.
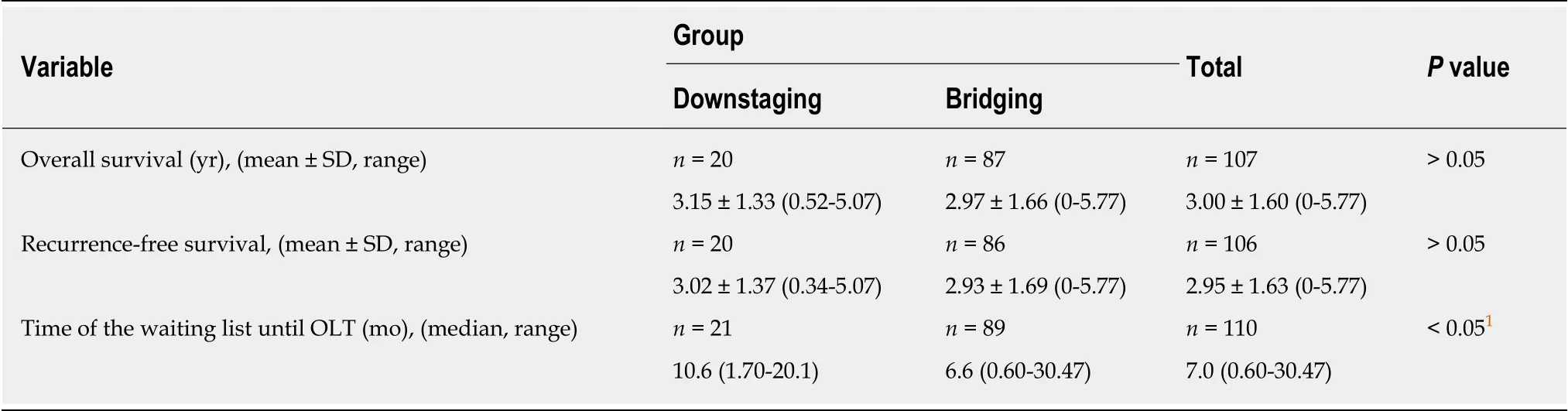
Table 5 Overall survival and recurrence-free survival
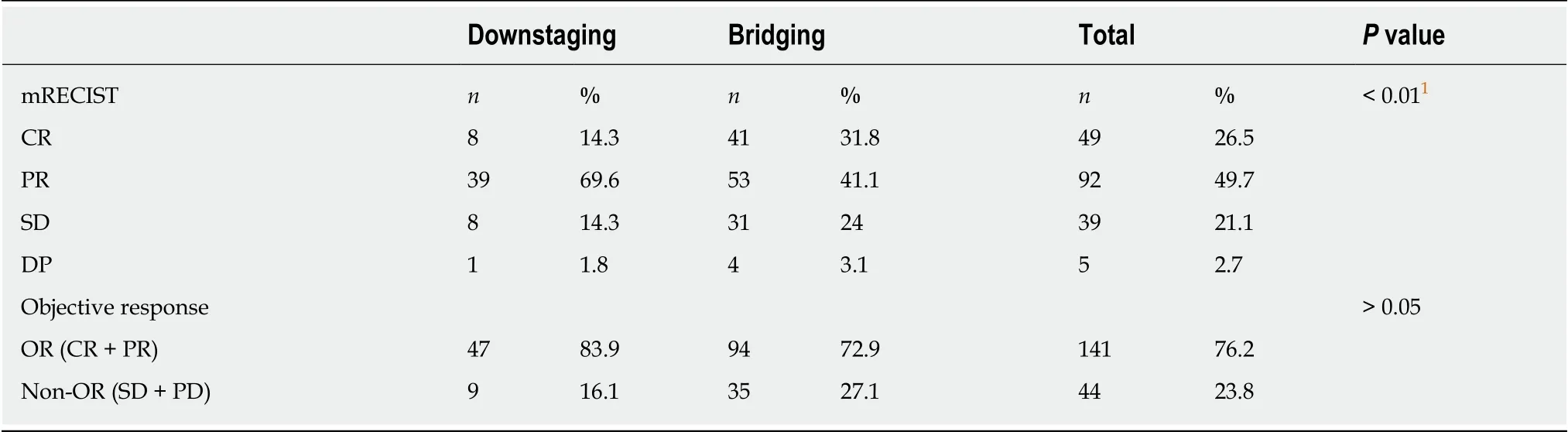
Table 6 Target lesion response
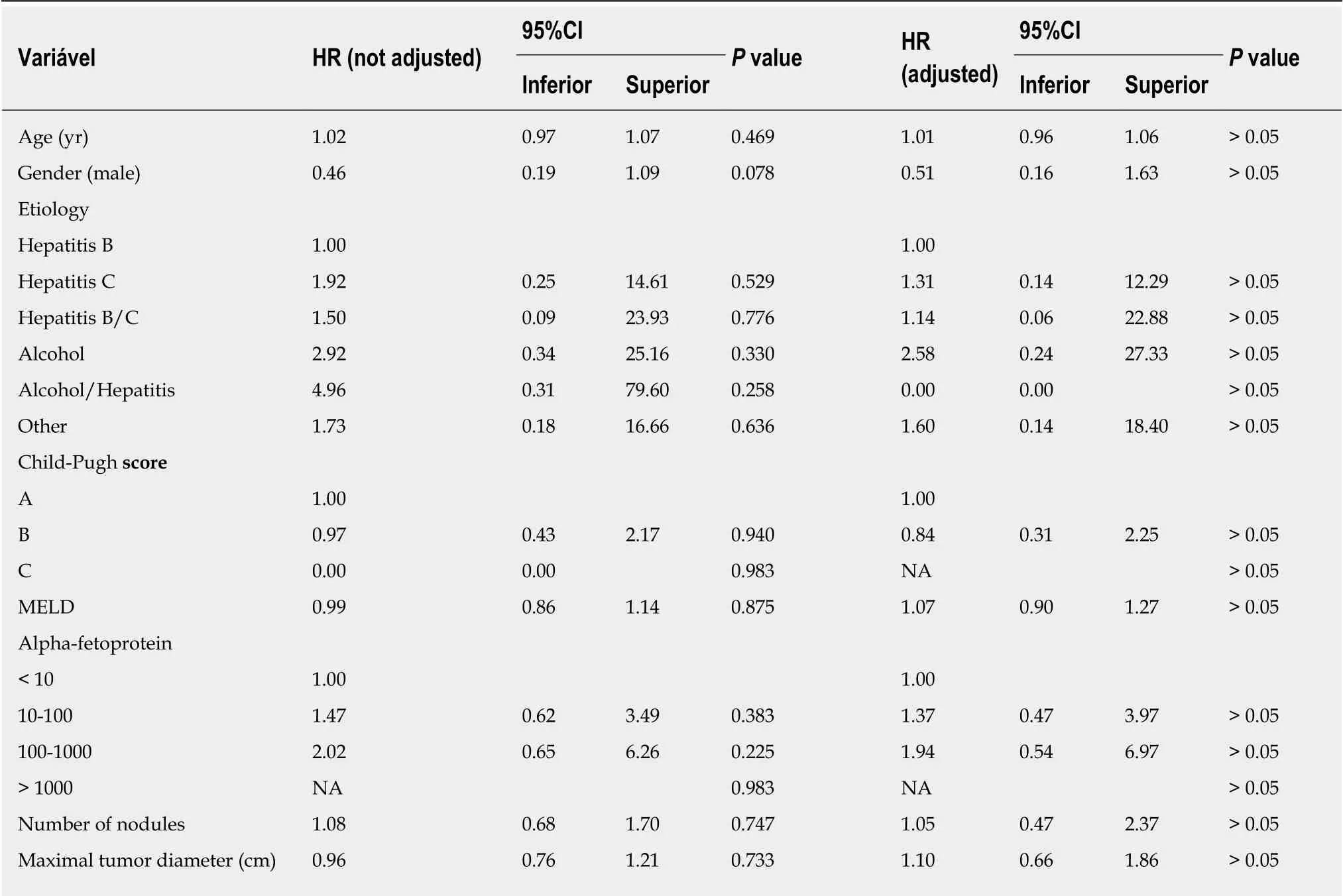
Table 7 lnfluence of baseline characteristics on overall survival after liver transplant
HR: Hazard ratio; CI: Confidence interval; NA: Not available.
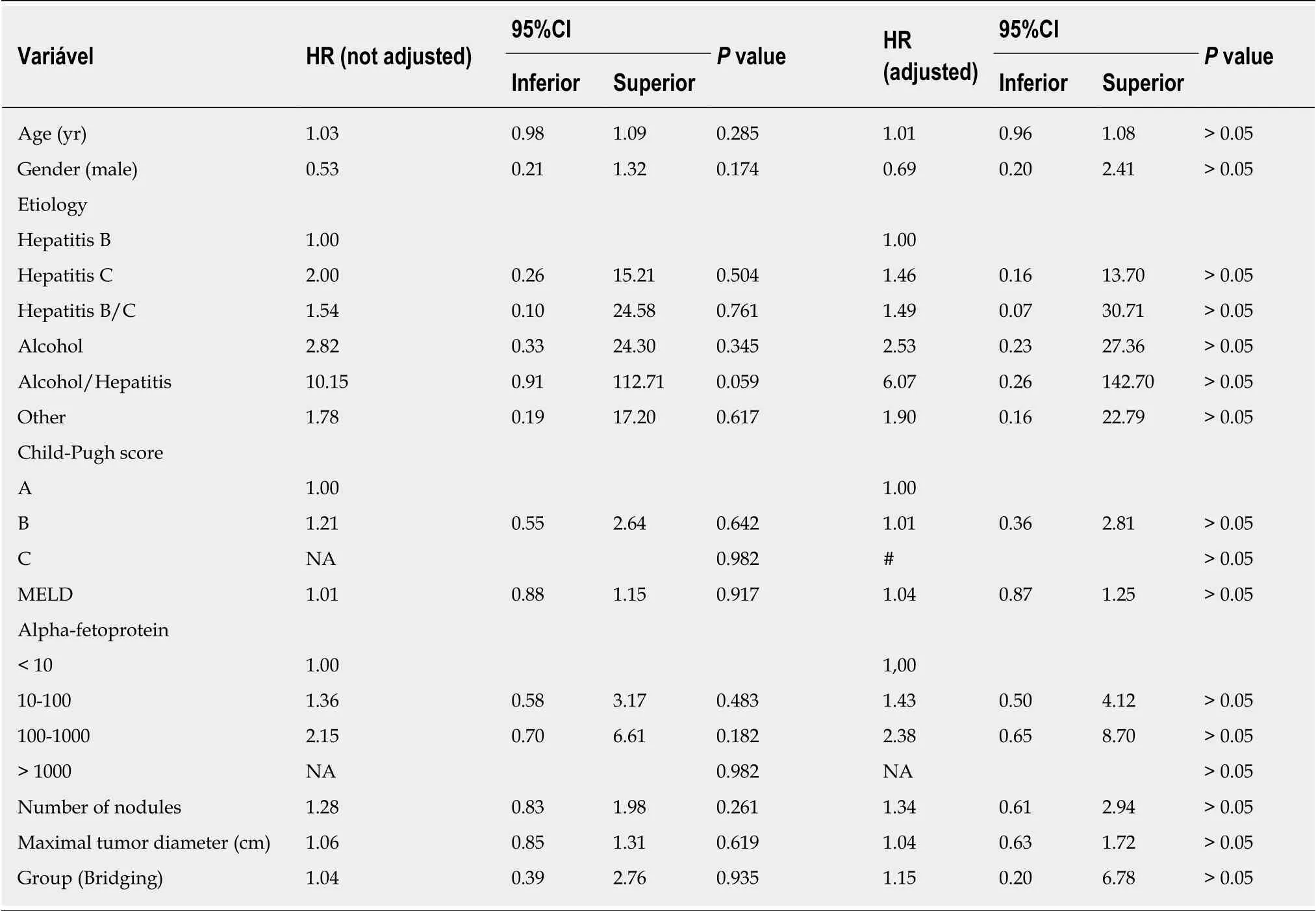
Table 8 lnfluence of baseline characteristics on recurrence-free survival after liver transplant
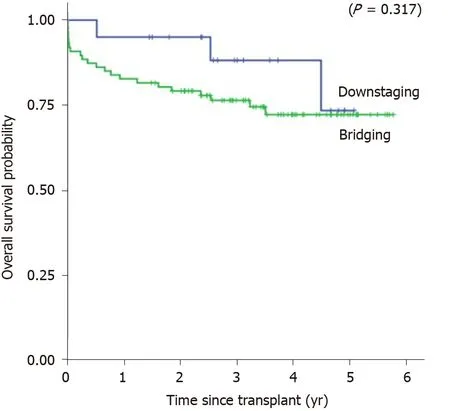
Figure 3 Kaplan-Meier’s overall survival probabilities of the downstaging group and the bridging group.
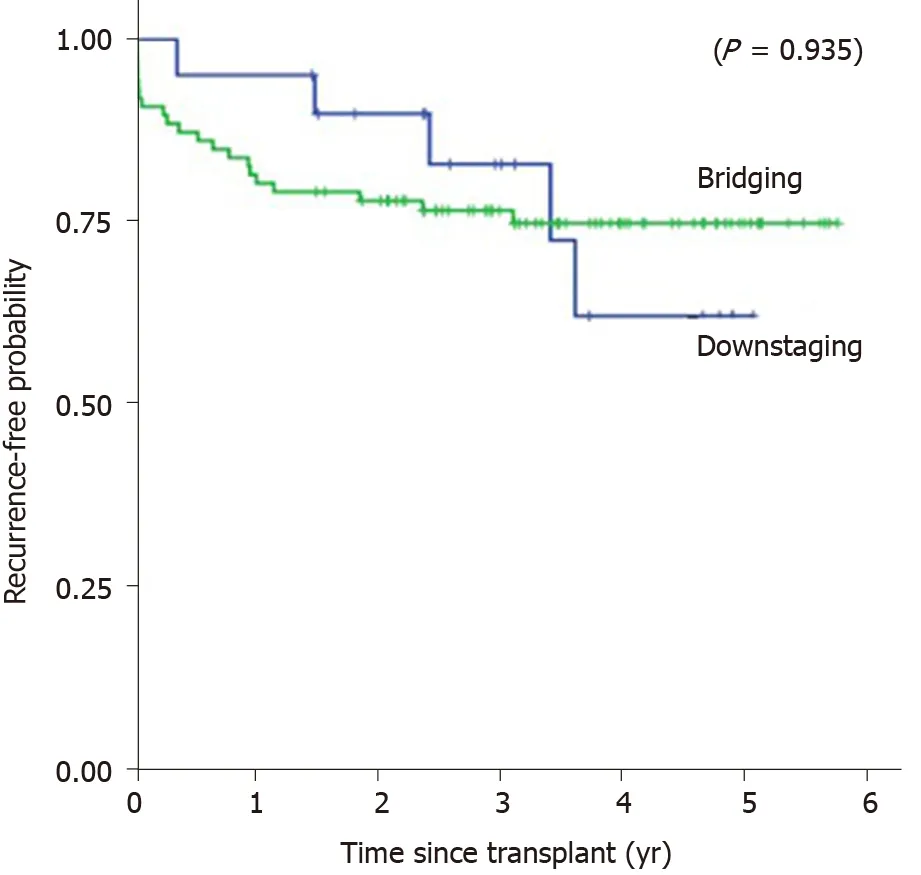
Figure 4 Kaplan-Meier’s recurrence-free survival probabilities of the downstaging group and the bridging group.
ARTICLE HIGHLIGHTS
杂志排行
World Journal of Gastroenterology的其它文章
- Pathogenesis and clinical management of Helicobacter pylori gastric infection
- Oncogenic ADAM28 induces gemcitabine resistance and predicts a poor prognosis in pancreatic cancer
- Correlation of plasma miR-21 and miR-93 with radiotherapy and chemotherapy efficacy and prognosis in patients with esophageal squamous cell carcinoma
- Accuracy of an administrative database for pancreatic cancer by international classification of disease 10th codes: A retrospective large-cohort study
- Post-transplant infection improves outcome of hepatocellular carcinoma patients after orthotopic liver transplantation
- Short-term efficacy of robotic and laparoscopic spleen-preserving splenic hilar lymphadenectomy via Huang's three-step maneuver for advanced upper gastric cancer: Results from a propensity score-matched study
