胃间质瘤临床病理特征及预后分析
2019-10-09方仕旭林彬王峰刘童蕾张同罗华友
方仕旭 林彬 王峰 刘童蕾 张同 罗华友

[摘要] 目的 探討胃间质瘤患者的临床病理特征及预后影响因素。 方法 回顾性分析2009年2月~2012年11月昆明医科大学第一附属医院胃肠外科收治的108例胃间质瘤患者的临床资料、病理特征及生存状态。生存分析采用Kplan-Meier法计算1、3、5年生存率,单因素分析采用log-rank检验,预后多因素分析采用COX比例风险模型。 结果 108例患者纳入研究,其中男57例,女51例,平均年龄(57.54±12.03)岁,手术时间(155.53±82.86)min,术中出血量(165.46±329.74)mL,术后进食时间(7.71±2.62)d,术后住院时间(11.80±7.54)d。全组患者1、3、5年总体生存率为100.0%、91.6%、76.3%。单因素分析结果显示:肿瘤大小、核分裂数、改良国际肿瘤协会(NIH)危险度级别与胃间质瘤预后有关(P < 0.05)。多因素分析显示:术后改良NIH危险度级别(HR = 6.177,95%CI:1.348~28.299,P = 0.019)是胃间质瘤患者预后的独立危险因素。 结论 胃间质瘤为消化道最常见的间质性肿瘤,总体预后较好,手术切除为主要治疗手段,术后改良NIH危险度级别为影响预后的主要危险因素,危险度越高提示预后越差。
[关键词] 胃间质瘤;临床特征;病理特征;预后
[中图分类号] R735.2 [文献标识码] A [文章编号] 1673-7210(2019)07(b)-0125-04
Clinicopathological features and prognosis of patients with gastric stromal tumors
FANG Shixu1 LIN Bin1 WANG Feng1 LIU Tonglei2 ZHANG Tong2 LUO Huayou2
1.The First Clinical College of Kunming Medical University, Yunnan Province, Kunming 650032, China; 2.Department of Gastroenterology and Hernia Surgery, the First Affiliated Hospital of Kunming Medical University, Yunnan Province, Kunming 650032, China
[Abstract] Objective To explore the clinicopathological features and prognostic factors of gastric stromal tumors further. Methods Clinical data, pathological characteristics and survival status of 108 patients with gastric stromal tumors admitted to the First Affiliated Hospital of Kunming Medical University from February 2009 to November 2012 were analyzed retrospectively. Survival analysis was used Kplan-Meier method to calculate 1, 3, 5-year survival rates. Log-rank test was used for univariate analysis and COX proportional hazards model was used for prognostic multivariate analysis. Results One hundred and eight patients were enrolled in the study. The male was 57 cases, the female was 51 cases, the age was (57.54±12.03) years, the operation time was (155.53±82.86) min, the intraoperative bleeding volume was (165.46±329.74) mL, the postoperative feeding time was (7.71±2.62) days, and the hospitalization days after operation were (11.80±7.54) days. The overall survival rates for 1, 3, 5 years were 100.0%, 91.6% and 76.3%. Univariate prognostic analysis showed that tumor size, mitotic numbe, modified NIH classification were closely related to prognosis of gastric stromal tumors (P < 0.05). Multivariate prognostic analysis showed that modified NIH risk classification (HR = 6.177, 95%CI: 1.348-28.299, P = 0.019) was an independent prognostic risk factor for patients with gastric stromal tumors. Conclusion Gastric stromal tumors are the most common digestive tract stromal tumors. The overall prognosis is good. Surgical resection is the main treatment. The modified NIH risk classification is the main risk factor affecting prognosis. The higher the risk, the worse the prognosis.
[Key words] Gastric stromal tumors; Clinical features; Pathological features; Prognosis
胃肠道间质瘤为消化道常见的间质性肿瘤,来自消化道肌层的Cajal细胞。表达特异性跨膜酪氨酸激酶受体蛋白c-kit(CD117),酪氨酸激酶信号激活导致细胞持续性增殖[1]。发病率为(10~15)/100万每年,发病年龄10~100岁,最多见于胃(约60%),其次是小肠(30%)[2-4]。胃间质瘤缺乏特异性临床表现,确诊靠术后病理的免疫组化分析,CD117和DOG1高活性及KIT突变、血小板源性生长因子受体的α多肽基因突变为主要标志[5-6]。胃间质瘤是一类具有潜在恶性的肿瘤[7],2002年国际肿瘤协会(NIH)制订了复发风险评估共识,后经修正完善后即改良版NIH危险度分级[8],用以评估间质瘤的危险度。本文主要回顾性分析胃间质瘤患者的临床表现、病理特征及预后影响因素,以提高对该疾病的认识,为临床有效治疗提供理论依据。
1 资料与方法
1.1 一般资料
回顾性分析昆明医科大学第一附属医院2009年2月~2012年11月胃肠外科收治的108例术后病理证实为胃间质瘤的患者,其中男57例(52.8%),女51例(47.2%),平均年龄(57.54±12.03)岁,平均术前体重指数(BMI)为(22.33±3.34)kg/m2。
1.2 研究方法
所有患者的术后标本均行病理切片检查。术后分级均按改良NIH分级标准执行。搜集患者的临床病理特征:首发症状、术前BMI、手术方式、手术时间、术中出血量、肿瘤大小、肿瘤部位、核分裂数、改良NIH危险度级别等。
1.3 统计学方法
采用SPSS 21.0统计软件进行数据处理,计量资料用均数±标准差(x±s)表示,采用独立样本t检验,计数资料采用χ2检验,生存分析采用Kplan-Meier法,单因素分析采用Log-rank检验,多因素分析采用COX比例风险模型,以P < 0.05为差异有统计学意义。
2 结果
2.1 临床及病理特征
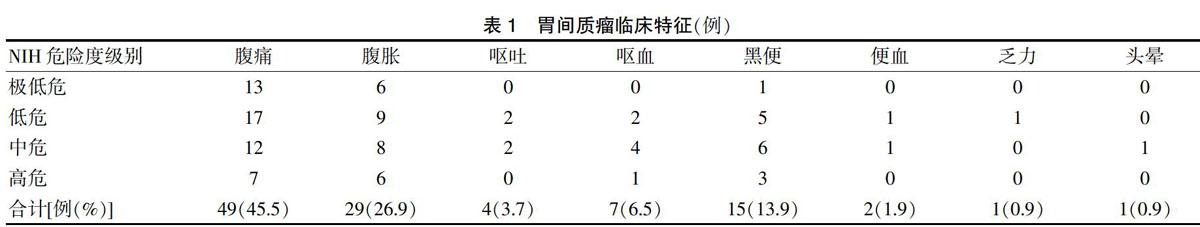
胃间质瘤患者首发症状中,以腹痛和腹胀最多见,其次为消化道出血的相关症状(呕血、黑便)。见表1。胃间质瘤患者肿瘤发生部位中,胃体最多,依次为胃底、胃窦和贲门,直径2~5 cm最常见,核分裂数以 <5/50 HPF最多。见表2。
2.2 手术治疗
108例患者中56例(51.9%)行腹腔镜手术,52例(48.1%)行开放手术。11例患者未能完整腔镜切除,中转为开放手术。手术方式以局部切除最常见。手术时间为(155.53±82.86)min,术中出血量为(165.46±329.74)mL,术后进食时间为(7.71±2.62)d,术后住院时间(11.80±7.54)d。术后高危患者建议服用伊马替尼辅助治疗3年。51例中高危患者23例接受药物辅助治疗,28例未进行辅助治疗,其中接受辅助治疗者未出现死亡,未接受辅助治疗者中13例死亡。接受辅助治疗者与未接受辅助治疗者生存率比较差异有统计学意义(χ2 = 14.332,P = 0.000),提示辅助治疗患者预后较好。
2.3 随访及预后
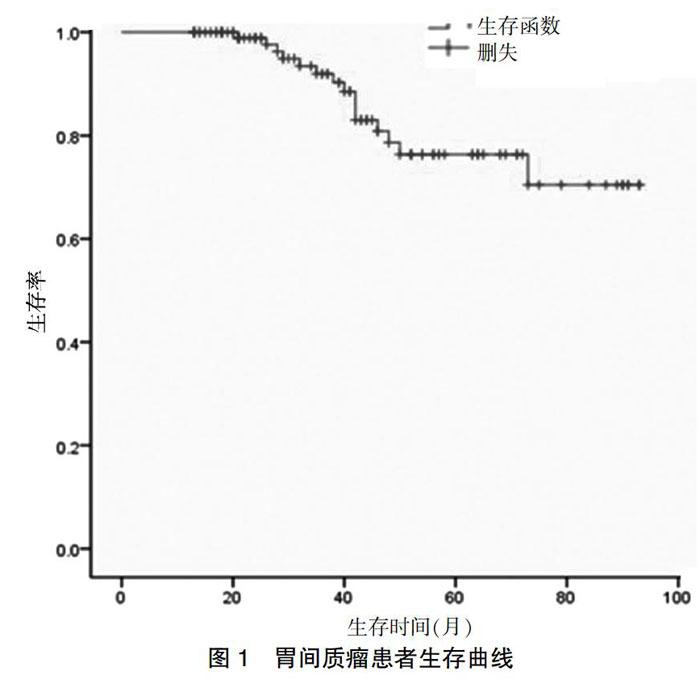
所有患者均获得随访,随访频率为3~6个月/次。采用电话、门诊复查等方式,起始时间为术后出院时间,截止日期为2017年12月30日,中位随访时间为38.5个月,随访期间死亡15例,其中13例因肿瘤复发转移死亡,2例因其他疾病死亡。预后分析:全组患者1、3、5年总体生存率分别为100.0%、91.6%、76.3%,生存曲线见图1。胃间质瘤患者肿瘤大小及核分裂数与NIH危险度级别有关(P < 0.05)。见表3。单因素分析显示:肿瘤大小、核分裂数、改良NIH危险度级别与胃间质瘤预后有关(P < 0.05)。见表4。多因素分析显示:改良NIH危险度级别是胃间质瘤预后的独立危险因素(P < 0.05)。见表5。
3 讨论
食管至直肠的任何部位均可发生胃肠道间质瘤,超过50%的为胃间质瘤[9],腹膜、肠系膜、腹膜后、肝脏、胆囊、前列腺等部位也有报道[6,10]。胃间质瘤预后较好,5年生存率达76.3%,与Huang等[11]的研究接近。临床表现无特异性,可为腹部包块、腹痛、腹胀、消化道出血等[12]。本研究中,患者中腹部不适(腹痛、腹胀)的患者最多见,余为消化道出血相关的临床表现(呕血、便血、黑便等),可能与肿瘤血供丰富、生长过快、局部坏死致血管破裂出血有关。指南推荐:手术为胃间质瘤的首选治疗[13],早期完整切除肿瘤可明显改善预后,才能治愈该疾病[14-15]。淋巴结转移率低(1%~4%)[16],无需行淋巴结清扫,据肿瘤部位及大小可采用局部切除、楔形切除、近端胃、远端胃、全胃等术式[17]。随着微创技术的发展,腹腔镜临床应用越来越广泛,具有创伤小、出血少、恢复快等优点,在胃间质瘤的治疗中扮演越来越重要的角色[18]。本研究患者主要采用腹腔手术方式,以局部切除为主。危险度因素分析显示:肿瘤的大小及核分裂数与NIH危险度级别有关(P < 0.05),与既往文献报道一致[19],肿瘤越大、核分裂數越高,其危险度级别可能就越高。本组108例患者中直径<5 cm、核分裂数≤5/50 HPF的患者,危险度级别较低,直径≥5 cm及核分裂数高的,危险度级别明显增高。单因素分析结果显示:肿瘤大小、核分裂数及改良NIH危险度级别与预后有关(P < 0.05);多因素分析结果显示:NIH危险度级别越高,患者预后越差。指南对于术后高危患者,推荐服用伊马替尼口服治疗3年,可明显降低复发率及提高总体生存率[20]。本研究中,高危患者服用药物辅助治疗的患者预后较好。
綜上所述,胃间质瘤临床表现无特异性,手术是主要治疗方法。NIH危险度级别与患者预后有关,对于危险度分级别较高的患者建议密切随访并辅助靶向治疗。
[参考文献]
[1] Connolly EM,Gaffney E,Reynolds JV. Gastrointestinal stromal tumours [J]. Br J Surg,2003,90(10):1178-1186.
[2] Pisters PW,Blanke CD,von Mehren M,et al. A USA registry of gastrointestinal stromal tumor patients:changes in practice over time and differences between community and academic practices [J]. Ann Oncol,2011,22(11):2523-2529.
[3] Soreide K,Sandvik OM,Soreide JA,et al. Global epidemiology of gastrointestinal stromal tumours (GIST):a systematic review of population-based cohort studies [J]. Cancer Epidemiol,2016,40:39-46.
[4] Wang M,Xu J,Zhang Y,et al. Gastrointestinal stromal tumor:15-years′ experience in a single center [J]. BMC Surg,2014,14:93.
[5] Blay JY,Shen L,Kang YK,et al. Nilotinib versus imatinib as first-line therapy for patients with unresectable or metastatic gastrointestinal stromal tumours (ENESTg1):a randomised phase 3 trial [J]. Lancet Oncol,2015,16(5):550-560.
[6] Miettinen M,Lasota J. Gastrointestinal stromal tumors [J]. Gastroenterol Clin North Am,2013,42(2):399-415.
[7] Yamamoto H,Oda Y. Gastrointestinal stromal tumor:recent advances in pathology and genetics [J]. Pathol Int,2015, 65(1):9-18.
[8] Joensuu H. Risk stratification of patients diagnosed with gastrointestinal stromal tumor [J]. Hum Pathol,2008,39(10):1411-1419.
[9] Mikami T,Nemoto Y,Numata Y,et al. Small gastrointestinal stromal tumor in the stomach:identification of precursor for clinical gastrointestinal stromal tumor using c-kit and alpha-smooth muscle actin expression [J]. Hum Pathol,2013,44(12):2628-2635.
[10] Almagharbi SA,Fayoumi YA,Abdel-Meguid TA,et al. Extragastrointestinal stromal tumor of prostate [J]. Urol Ann,2018,10(4):416-419.
[11] Huang H,Liu YX,Zhan ZL,et al. Different sites and prognoses of gastrointestinal stromal tumors of the stomach:report of 187 cases [J]. World J Surg,2010,34(7):1523-1533.
[12] Rammohan A,Sathyanesan J,Rajendran K,et al. A gist of gastrointestinal stromal tumors:a review [J]. World J Gastrointest Oncol,2013,5(6):102-112.
[13] Joensuu H,Hohenberger P,Corless CL. Gastrointestinal stromal tumour [J]. Lancet,2013,382(9896):973-983.
[14] Akahoshi K,Oya M,Koga T,et al. Clinical usefulness of endoscopic ultrasound-guided fine needle aspiration for gastric subepithelial lesions smaller than 2 cm [J]. J Gastrointestin Liver Dis,2014,23(4):405-412.
[15] Usta TA,Karacan T,Naki MM,et al. Comparison of 3-dimensional versus 2-dimensional laparoscopic vision system in total laparoscopic hysterectomy:a retrospective study [J]. Arch Gynecol Obstet,2014,290(4):705-709.
[16] Agaimy A,Wunsch PH. Lymph node metastasis in gastrointestinal stromal tumours (GIST) occurs preferentially in young patients ≤ 40 years:an overview based on our case material and the literature [J]. Langenbecks Arch Surg,2009,394(2):375-381.
[17] Koga T,Hirayama Y,Yoshiya S,et al. Necessity for resection of gastric gastrointestinal stromal tumors ≤ 20 mm [J]. Anticancer Res,2015,35(4):2341-2344.
[18] Chen K,Zhou YC,Mou YP,et al. Systematic review and meta-analysis of safety and efficacy of laparoscopic resection for gastrointestinal stromal tumors of the stomach [J]. Surg Endosc,2015,29(2):355-367.
[19] Ucar AD,Oymaci E,Carti EB,et al. Characteristics of emergency gastrointestinal stromal tumor (GIST) [J]. Hepatogastroenterology,2015,62(139):635-640.
[20] Joensuu H,Eriksson M,Sundby Hall K,et al. One vs three years of adjuvant imatinib for operable gastrointestinal stromal tumor:a randomized trial [J]. JAMA,2012,307(12):1265-1272.
