Occupational exposure to vinyl chloride and liver diseases
2019-09-13UgoFedeliPaoloGirardiGiuseppeMastrangelo
Ugo Fedeli, Paolo Girardi, Giuseppe Mastrangelo
Abstract Portal hypertension, liver fibrosis, and angiosarcoma of the liver (ASL) have been reported among workers exposed to vinyl chloride monomer (VCM) since the 1970s. In 2007, the International Agency for Research on Cancer established the association of VCM with hepatocellular carcinoma (HCC), though only on the basis of the few cases available. Thereafter, recent reports from the United States cohort and a European sub-cohort of vinyl chloride workers provided compelling evidence of a strong association between cumulative VCM exposure and HCC risk. Further areas of research include the risk of liver cancer at lower levels of exposure and different patterns of risk of ASL and HCC with the time since exposure. The evidence of interaction between VCM exposure and other known liver carcinogens such as alcohol and chronic viral infection provides clues for the health surveillance of exposed workers. Notably, also the risk of VCM-associated chronic liver disease is modulated by alcohol consumption, viral infection, and genetic polymorphism. A counter-intuitive finding from cohort studies of exposed workers is the lower mortality from liver cirrhosis with respect to the general population; this can be attributed to the healthy worker effect and to the selection of liver cancer as the cause of death in the presence of concomitant chronic liver disease. Studies designed to overcome these intricacies confirmed an association between cumulative VCM exposure and the risk of liver cirrhosis.
Key words: Vinyl chloride; Occupational exposure; Epidemiology; Liver cancer;Angiosarcoma; Hepatocellular carcinoma; Liver cirrhosis
INTRODUCTION
Vinyl chloride monomer (VCM) is a synthetic gas mostly used in the manufacture of polyvinyl chloride (PVC), a widely used plastic material. Occupational exposure to VCM primarily occurs in the VCM/PVC production and processing industry[1]. The role of occupational exposure to VCM in the development of angiosarcoma of the liver (ASL) is well known since the mid-1970s. In 2007, the International Agency for Research on Cancer (IARC) established that exposure to VCM causes both ASL and hepatocellular carcinoma (HCC)[2]. The evidence on HCC was mainly derived from studies carried out in the early 2000s, demonstrating a relationship between HCC incidence and cumulative VCM exposure, as well as an association of VCM exposure with liver cirrhosis[3-5].
However, some controversy remained because findings on HCC were based only on a limited number of confirmed cases. Such controversy was fueled by reviews issued by VCM industry consultants, claiming that the results about HCC might have been biased due to misclassification between HCC and ASL, and underlining the fact that overall among VCM workers mortality from liver cirrhosis was lower with respect to the general population[6-8]. Notably, one of these reviews deduced that a firm conclusion about the role of VCM in the development of liver diseases other than ASL is unlikely to be reached in the future, because of the contrasting personal views given by experts[8]. The statements regarding irresolvable controversies might be used in the legal setting, yet the scientific evidence usually proceeds by slowly accumulating new original studies that shed light on gray areas of the available knowledge.
In fact, after the IARC assessment, new epidemiological studies updating previous results from cohorts of workers employed in VCM/PVC production in the United States[9], Europe[10,11], and Taiwan[12]have been published. Aim of this review is to summarize such new findings within the frame of the previous evidence.
HEPATOCELLULAR CARCINOMA
An increase in mortality from liver cancer among vinyl chloride workers has been reported by several studies carried out in the past decades, especially two large multicentric cohort studies from the United States[9,13-15]and Europe[3,16]. However, the association between VCM exposure and HCC is difficult to investigate because most studies did not collect histological or clinical information distinguishing HCC from ASL or other primary/secondary neoplasms[1]. The IARC assessment carried out in 2007 relied mostly on the results from the European cohort of workers employed in the vinyl chloride industry[3], from an Italian sub-cohort[4], and a case-control study nested in the latter sub-cohort[5]. Overall, a clear association of HCC risk with cumulative exposure was found, although based only on a few confirmed cases(ranging from 10 to 13).
Two studies have recently confirmed the IARC assessment. For the first time in 2017, data were published from the US cohort of vinyl chloride workers specifically addressing HCC risk, with the diagnosis based on information reported in death certificates. The risk of HCC steeply increased with increasing duration of employment and VCM cumulative exposure. The authors warned that in the absence of histopathological confirmation, such figures might have been influenced by misclassification of ASL and HCC in the earlier decades[9]. However, such misclassification did not probably affect the main results since findings were confirmed after exposures were lagged by 10-40 years. More recently, an update of an Italian cohort of vinyl chloride workers found a strong association with VCM cumulative exposure in a large series of HCC confirmed by histology and/or clinical records[11]. In summary, all the original studies available provide compelling evidence of the causal role of occupational VCM exposure in the development of HCC (Table 1).
It must be remarked that vinyl chloride is mutagenic, being associated to chromosomal aberrations, micronucleus formation, sister chromatid exchange, Ki-ras and p53 gene mutations[2]; furthermore, the development of liver cirrhosis per se increases the risk of HCC through multiple mechanism, including chromosomal instability[17]. Within this framework, specific aspects of the association between VCM and HCC, namely, the absence of risk below a threshold of exposure, a decrease in the rates of liver cancer in historical cohorts through the more recent decades of followup, and interactions with other known risk factors for HCC, need further clarification.
Analyses on the risk of HCC at low levels of cumulative VCM exposure are hampered by the limited number of available cases. In the United States cohort, based on 32 cases of HCC as identified from death certificates, mortality rates did not increase except for the highest quintile of cumulative exposure (≥ 2271 ppm-years).However, after exposures were lagged by 30 years, HCC mortality significantly increased already in the 865-2271 ppm-years class (or in the 1021-3301 ppm-years class using high cut-points based on quintiles for all liver cancers, see also Table 1).The authors suggested a possible threshold at about 1000 ppm-years cumulative exposure[9]. In the European cohort of vinyl chloride workers, an increase in liver cancer risk (all types) with increasing exposure was confirmed in analyses restricted to subjects with cumulative exposure < 1500 ppm-years[3]. In an Italian cohort, an approach based on a non-parametric regression was adopted to model in continuous form the relationship between exposure and mortality considering 31 confirmed HCC cases; HCC mortality rates were found to increase with cumulative VCM exposure already in the range below 2000 ppm-years[11]. In view of the above data, the risk of HCC seems not to be confined only to a few subjects in the highest exposure categories, but probably involves most workers from the United States and Europe,who had relevant exposures to VCM before the major improvements in working conditions achieved in the mid-1970s.
The second issue is represented by the possible decline in liver cancer risk among previously exposed workers decades after the large decrease in the VCM exposure levels that were achieved in the chemical industry. According to the last update of the cohort of vinyl chloride workers in Taiwan[12], liver cancer mortality reached a peak during 1991-1996, and thereafter showed a decline. Although information on histological type was missing for most patients who died of liver cancer, the limited number of cases with available medical records were all confirmed HCC, with no case of ASL identified[18]. In the United States cohort, the peak of standardized mortality ratios (SMR) for liver cancer (all types) was observed during the 1970s; however, in subsequent decades a more than two-fold excess risk for liver cancer was still observed[15]. Among the confirmed cases, the median latency for HCC (48 years) was found to be considerably longer than that for ASL (36 years)[9]. In an Italian cohort of vinyl chloride workers, SMRs for liver cancer remained increased through the most recent period of follow-up[11]; analyses by latency showed that the highest SMR was reached after more than 40 years from the first exposure[10,11]. Once again among the confirmed cases, latency was observed to be longer for HCC as compared to ASL,being mean latency 39 and 32 years, respectively[11]. The overall picture from the historical cohorts is consistent with a first major peak of liver cancer deaths, mostly represented by ASL; in the more recent decades, mortality for liver cancer remained significantly increased, mainly sustained by the occurrence of HCC.
A common criticism of cohort studies is the lack of adjustment for known risk factors such as alcohol consumption and hepatitis B virus (HBV) or hepatitis C virus(HCV) infection. Two nested case-control studies, already included in the IARC review, investigated such an issue. A multiplicative effect between employment in jobs with high VCM exposure and HBsAg carrier status was reported for liver cancer(mostly HCC) in the Taiwanese cohort[19]. Furthermore, a study from Italy reported that cumulative VCM exposure was an independent risk factor for HCC, interacting synergistically with alcohol consumption and additively with viral infection[5]. Such studies provide useful clues for the health surveillance and disease prevention in previously exposed workers, as the interaction between multiple exposures further increases the risk for HCC. Therefore, cessation of alcohol consumption and treatment of chronic viral infection should be prioritized among vinyl chloride workers,especially in the view of the recent availability of directly acting antivirals for HCV treatment.
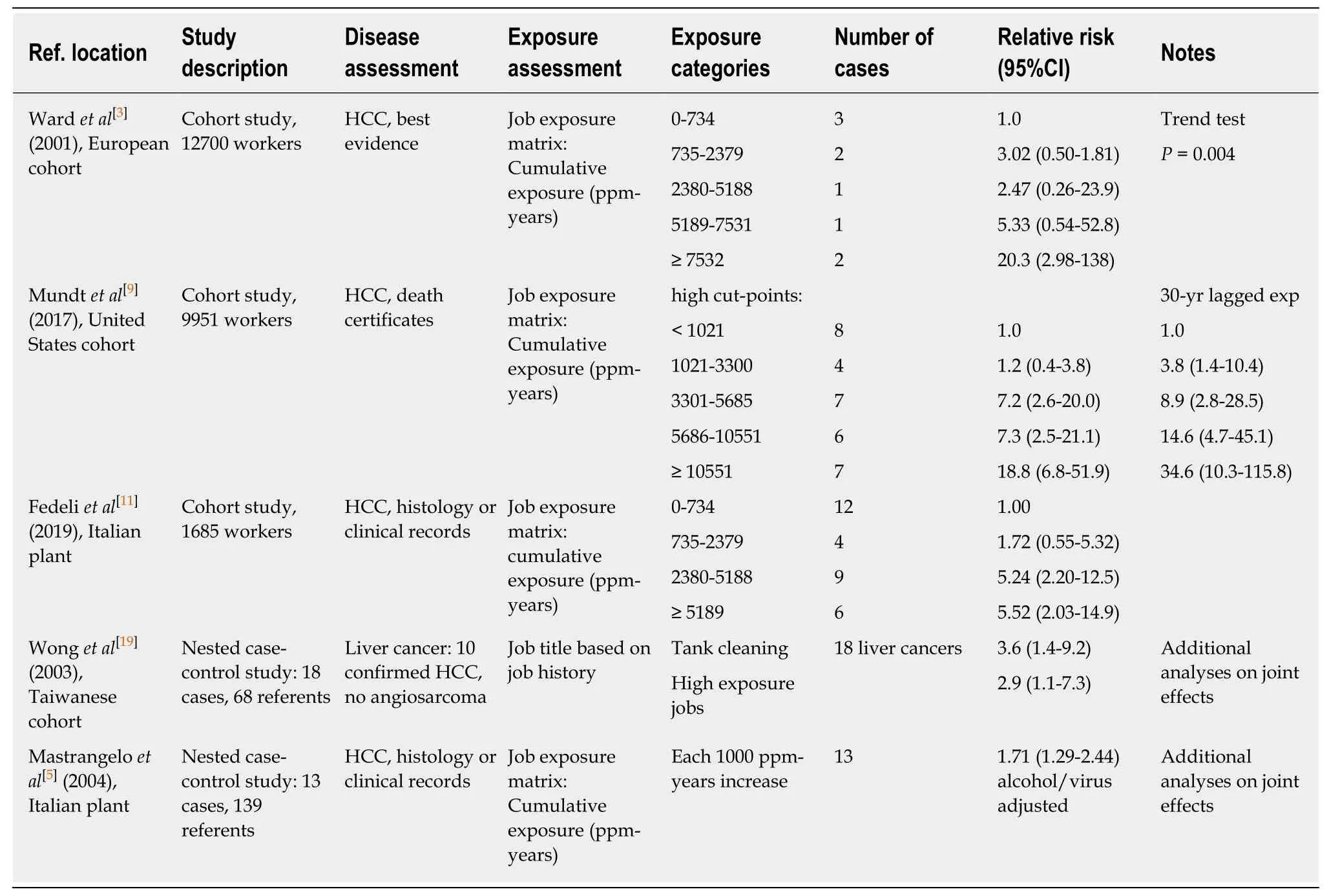
Table 1 Studies investigating the association between occupational exposure and hepatocellular carcinoma in vinyl chloride workers
CHRONIC LIVER DISEASE
Portal hypertension and fibrosis at liver biopsy have been reported among VCM production workers since the 1970s[20]. Thereafter, multiple studies adopting different approaches have investigated the association between occupational exposure to VCM and chronic liver disease: Prevalence surveys among active workers, cohort mortality studies, nested case-control studies. Ultrasonography was advocated as the preferred method for health surveillance of workers exposed to VCM since the mid-1970s:Enlarged portal vein, splenomegaly, and changes in hepatic structure were the most commonly observed abnormalities; by contrast, liver function tests were reported to be unsuitable for the detection of VCM-associated liver diseases[21]. Subsequent studies reported contrasting results for liver function tests, and a possible role for cholestasis indices was suggested for the surveillance of exposed workers[22]. In spite of the early recognition of the role of liver ultrasonography, only a few studies describing the findings associated with VCM exposure have been published. An increased prevalence of periportal liver fibrosis among workers with past high VCM exposure was reported among 757 Italian workers, whereas no association with steatosis and changes in liver function tests was observed[23,24]. Among 347 male workers in Taiwan,those with a history of high VCM-exposure jobs were at a higher risk of liver fibrosis(a category combining cirrhotic and pre-cirrhotic sonographic changes of the liver).Other risk factors for liver fibrosis included overweight/obesity and HBV/HCV infection; workers with both viral infection and high exposure were at the highest risk of liver fibrosis[25]. A possible role of genetic polymorphism of Cytochrome P450 2E1(CYP2E1) in the development of VCM-induced liver fibrosis was suggested[26]. Among Taiwanese workers, a synergistic effect between high VCM exposure and hepatitis viral infection was also found responsible for increased transaminase levels[27]. The association between occupational VCM exposure and chronic liver disease was confirmed by higher rates of hospital admissions for cirrhosis with respect to nonexposed reference workers[28]. Lastly, an increasing prevalence of abnormalities (all types) was detected at liver ultrasonography across workers with no, low, and high VCM exposures in China; once again, a joint effect with CYP2E1 polymorphism was reported[29].
The studies investigating ultrasonography findings among VCM workers still employed in Western countries and Taiwan were carried out about twenty years after the end of high exposure periods, with a possible underestimation of risks due to workers quitting job as a consequence of liver diseases[25]. More recently, Cave and colleagues reviewed slides from liver biopsies and analyzed frozen sera obtained during 1974-1977 from 25 United States workers with extremely high exposure submitted to intensive medical surveillance (four had concomitant ASL, with a fifth case developing ASL in subsequent years)[30]. Steatohepatitis was observed in 20 (80%)biopsies, among which, liver fibrosis was present in 11. Notably, among these cases,called “Toxicant Associated Steatohepatitis” (TASH), serum transaminases were not altered with respect to healthy chemical workers. TASH, the consequence of current high VCM exposures, may not always be reversible after exposure has been withdrawn and may further evolve into progressive liver injury and fibrosis[30].
The role of VCM exposure in the development of chronic liver disease has been confirmed by a case-control study carried out within an Italian cohort of VCM workers[5]. The case group comprising 40 patients with cirrhosis diagnosed at histology or on a clinical basis was compared to 139 reference workers without any liver disease. Cumulative VCM exposure was an independent risk factor for cirrhosis,interacting with both alcohol consumption and viral infection.
By contrast, cohort studies on vinyl chloride workers usually report a risk of mortality from liver cirrhosis/chronic liver disease lower than the expected based on rates registered in the general population; this finding can be attributed to the healthy worker effect[7]. Within-cohort analyses avoiding bias derived from comparison with an external reference have been performed in the European and the United States cohorts. In both cohorts, increased mortality rates were observed in highly exposed groups with respect to the reference group having the lowest exposure (Table 2),although a linear trend across the categories of cumulative exposure could not be demonstrated[3,9]. It must be remarked that mortality from cirrhosis can be underestimated especially among highly exposed workers. In the presence of ASL or HCC, liver cancer will be selected as the underlying cause of death, whereas the coexisting chronic liver disease will be mentioned only as a concomitant cause (or even omitted)[11,31]. To overcome this limit, deaths from liver cirrhosis were analyzed together with the deaths of patients with histologically or clinically evident cirrhosis,yet having liver cancer as the underlying cause: A strong association with cumulative VCM exposure was demonstrated[11].
CONCLUSION
Occupational exposure to VCM causes a substantial burden of liver diseases; in the last update of an Italian cohort, as much as 29% of overall deaths among workers in the highest exposure category were from liver cancer (all types) or liver cirrhosis[11].Available original studies reviewed by IARC and published after the IARC assessment confirm the association between occupational VCM exposure and chronic liver disease as well as HCC. Further research is warranted to assess the disease risk in the lower range of cumulative exposure and to investigate the pattern of risk with the time elapsed since exposure. The evidence of additive or multiplicative interactions with other known risk factors should prompt health surveillance and promotion programs among exposed workers, aimed at reduction of alcohol consumption and body weight, and identification and treatment of chronic viral infection.
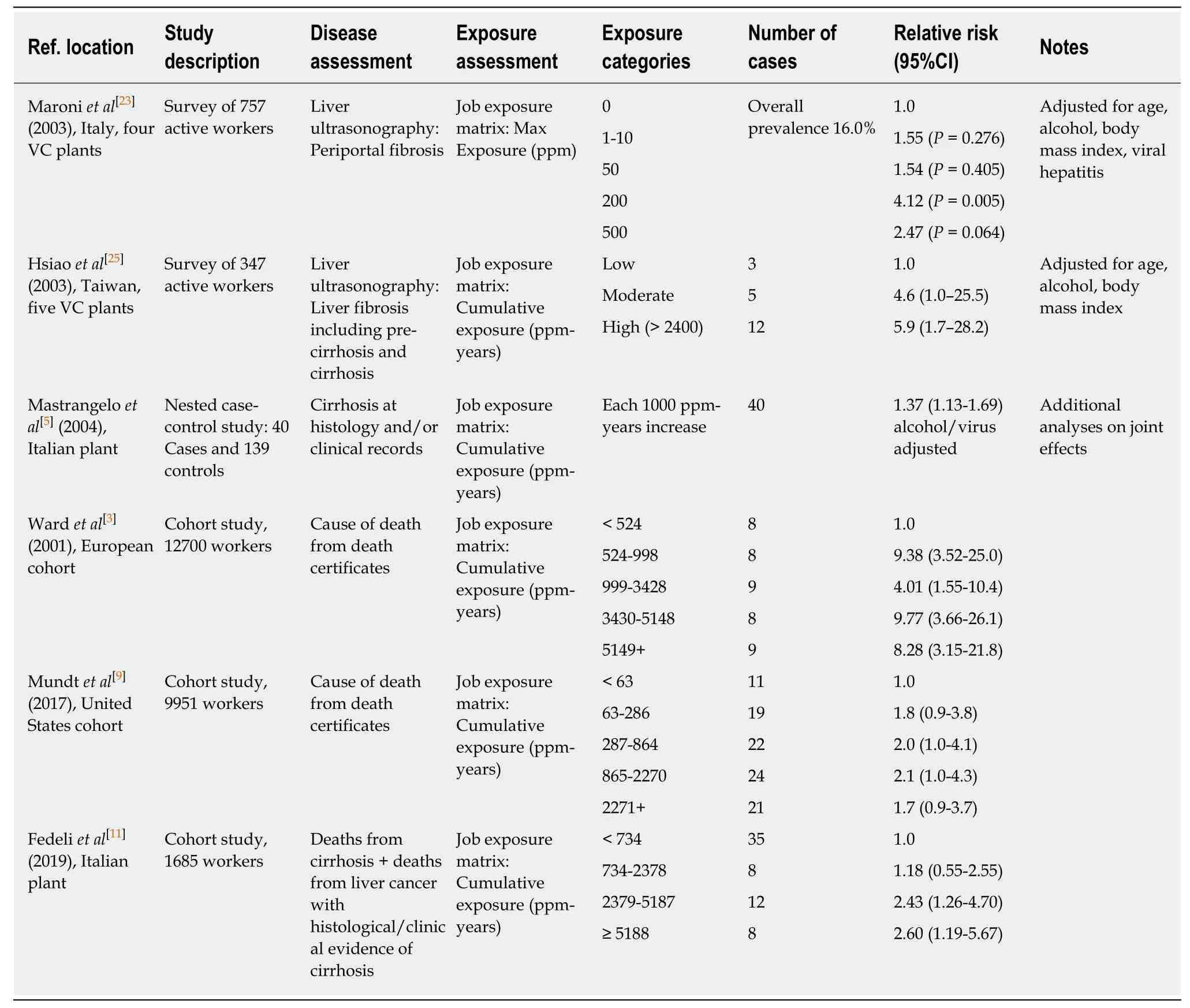
Table 2 Studies investigating the association between occupational exposure and liver fibrosis/liver cirrhosis in vinyl chloride workers
杂志排行
World Journal of Gastroenterology的其它文章
- Role of NLRP3 inflammasome in inflammatory bowel diseases
- Gastroesophageal reflux disease, obesity and laparoscopic sleeve gastrectomy: The burning questions
- Intestinal permeability in the pathogenesis of liver damage: From non-alcoholic fatty liver disease to liver transplantation
- Crosstalk network among multiple inflammatory mediators in liver fibrosis
- Neoadjuvant radiotherapy for rectal cancer management
- Helicobacter pylori virulence genes
