颈椎前路手术减压程度对神经根型颈椎病的影响
2019-09-09刘亚东孔超崔利宾彦辉陈学明
刘亚东 孔超 崔利宾 彦辉 陈学明

[摘要] 目的 探討颈椎前路手术的减压程度对神经根型颈椎病的影响。 方法 84例神经根型颈椎病患者2016年1月~2018年1月于首都医科大学附属北京潞河医院完成颈椎前路减压融合手术。根据术后随访时患者对手术疗效的主观缓解程度分为完全缓解组(73例)和未完全缓解组(11例)。分别记录测量每位患者术前及术后随访时手术节段MRI轴位像上致压物的面积、视觉模拟评分(VAS)和颈椎功能障碍指数(NDI)评分。记录每位患者术中出血量及手术时间,观察围术期及近中期并发症。 结果 所有患者均顺利完成手术,平均手术时间为(131.45±9.45)min,平均术中出血量为(51.23±31.16)mL。两组术后VAS及NDI评分均较术前降低,致压物面积较术前减小,差异有统计学意义(P < 0.05)。完全缓解组术后VAS及NDI评分均较未完全缓解组降低,致压物面积较未完全缓解组减小,差异有统计学意义(P < 0.05)。所有患者中无椎动脉损伤,围术期无术后血肿形成。 结论 颈椎前路手术是治疗神经根型颈椎病的有效手段,但部分患者术后症状的残留可能与术中减压不彻底有关,彻底减压不会明显增加术后并发症。
[关键词] 神经根型颈椎病;颈椎前路;减压程度;临床症状
[中图分类号] R681.5 [文献标识码] A [文章编号] 1673-7210(2019)06(c)-0073-04
Effect of decompression extent of cervical anterior approach on cervical spondylotic radiculopathy
LIU Yadong1 KONG Chao2 CUI Libin1 WANG Yanhui1 CHEN Xueming1
1.Department of Spinal Surgery, Bone Center, Beijing Luhe Hospital, Capital Medical University, Beijing 101149, China; 2.Department of Orthopedics, Beijing Xuanwu Hospital, Capital Medical University, Beijing 100053, China
[Abstract] Objective To investigate the effect of decompression extent of cervical anterior approach on cervical spondylotic radiculopathy (CSR). Methods From January 2016 to January 2018, 84 CSR patients were performed with anterior cervical discectomy and fusion (ACDF) in Beijing Luhe Hospital, Capital Medical University. According to degree of remission at the postoperative follow-up, the patients were divided into two groups (complete remission group, 73 cases and incomplete remission group, 11 cases). Compressive areas in operative level, visual analogue scale (VAS) and neck disability index (NDI) of patients were recorded at pre-operation and postoperative follow-up. Intra-operative blood loss and duration of operation were recorded. The post-operation and on short and midium term complications were also concerned. Results All of the patients were performed with operation successfully, average of duration of operation was (131.45±9.45) min and average of intra-operative blood loss was (51.23±31.16) mL. Postoperative VAS and NDI scores in both groups were lower than those before operation, and the area of pressure substance in both groups was smaller than that before operation, there was significant difference between two groups (P < 0.05). Postoperative VAS and NDI scores of complete remission group were lower than those of incomplete remission group, and the area of pressure substance of complete remission group was smaller than that of incomplete remission group, there was significant difference between two groups (P < 0.05). There was no vertebral artery injury or hematoma formation during perioperative period in all patients. Conclusion ACDF is a valid method for the therapy of CSR, but residual symptom of partial patients may be related with incomplete decompression. Complete decompression would not markedly increase the complications.
[Key words] Cervical spondylotic radiculopathy; Anterior approach; Decompression extent; Clinical symptom
神经根型颈椎病(cervical spondylotic radiculopathy,CSR)是最常见的一种颈椎病,主要表现为受累神经根分布区域的疼痛、麻木、无力等[1-2]。保守治疗是CSR的首选治疗方法,但对上肢顽固性疼痛、肌力减退且经保守治疗无效患者,手术可能是缓解症状最有效的方法[3]。颈椎前路手术有直接解除压迫、改善颈椎曲度、稳定颈椎的作用,在临床中应用广泛。颈椎前路手术需要彻底去除神经根前方的压迫,如果神经根减压不充分,可导致症状残留,达不到患者预期疗效,而过度减压有可能导致椎动脉及神经根的损伤[4]。因此颈椎前路手术治疗CSR的减压程度一直存在争议,大多数术者主要依靠临床经验,并没有客观依据。本研究回顾性随访了首都医科大学附属北京潞河医院(以下简称“我院”)行颈椎前路减压融合术的CSR患者,比较其术前和术后颈椎MRI上手术节段致压物的面积,评价减压程度对临床疗效的影响,并观察围术期及近中期并发症,以提高颈椎前路手术治疗CSR的安全性和有效性。
1 资料与方法
1.1 一般资料
2016年1月~2018年1月共有97例符合纳入标准的CSR患者在我院接受颈椎前路椎间盘切除减压椎间融合术,其中84例(86.6%)患者获得半年以上随访且资料完整,随访时间7~29个月,平均(15.8±5.0)个月。纳入本研究的84例患者中,男31例,女53例,年龄32~73岁,平均(54.3±7.8)岁。根据术后随访时患者对手术疗效的主观缓解程度分为完全缓解组(73例)和未完全缓解组(11例)。纳入标准:①结合症状、体征及影像学表现,临床诊断为单节段单侧CSR;②经正规保守治疗后症状缓解不满意;③手术方式为颈椎前路椎间盘切除减压椎间融合术。排除标准:①脊髓型、混合型等其他类型的颈椎病;②双侧症状患者或者两个节段及以上患者;③颈椎后路手术患者。
1.2 手术方法
所有患者均全麻下手术。术前根据责任节段确定前路手术切口位置,逐层分离颈阔肌、封套筋膜至椎体前方,透视下定位,确定责任节段,采用撑开器撑开椎间隙。切除椎间盘至钩椎关节后,以直径4.5 mm磨钻将钩突基底部内侧磨平,充分显露钩突后部、上位椎体后下角及钩椎关节间隙,用大小不等的正、反向刮勺自内向外上方逐渐刮除上位椎体后下角及部分增生的钩突,直至椎间孔通畅,完成神经根减压。紧贴骨面减压以避免或减少出血。如术中出血用蘸凝血酶的明胶海绵压迫5 min。减压后均行椎间隙植入自体髂骨或椎间融合器植骨,并行前路钛板内固定。
1.3 评价指标
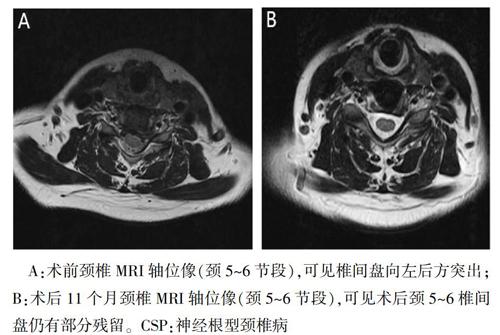
对符合纳入标准的患者,采用Surgimap软件测量其术前及术后随访时手术节段MRI轴位像上致压物的面积(图1~2)。评估每位患者术前及术后随访时神经功能评价指标:视觉模拟评分(visual analogue scale,VAS)[5]和颈椎功能障碍指数(neck disability index,NDI)评分[6]。记录每位患者术中出血量及手术时间,观察围术期及近中期并发症。
A:术前颈椎MRI轴位像(颈5~6节段),可见椎间盘向左后方突出;B:术后11个月颈椎MRI轴位像(颈5~6节段),可见术后颈5~6椎间盘仍有部分残留。CSP:神经根型颈椎病
1.4 统计学方法
采用SPSS 22.0软件进行统计学分析,计量资料用均数±标准差(x±s)表示,采用t检验,计数资料采用χ2检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 一般情况
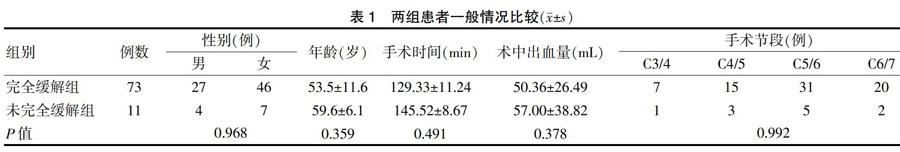
所有患者均顺利完成手术,平均手术时间为(131.45±9.45)min,平均术中出血量为(51.23±31.16)mL,平均住院天数为(6.87±2.33)d。手术节段分别为C3/4节段8例,C4/5节段18例,C5/6節段36例,C6/7节段22例。两组患者性别、年龄、手术时间、术中出血量、手术节段比较差异无统计学意义(P > 0.05),具有可比性。见表1。
2.2 临床疗效评价
两组术后VAS及NDI评分均较术前降低,致压物面积较术前减小,差异有统计学意义(P < 0.05)。完全缓解组术后VAS及NDI评分均较未完全缓解组降低,致压物面积较未完全缓解组减小,差异有统计学意义(P < 0.05)。见表2。
2.3 术后并发症情况
所有患者均无椎动脉损伤,围术期无术后血肿形成,两组中分别有1例患者出现手术节段神经根支配肌力的下降,均在3个月内完全恢复正常。
3 讨论
CSR是指一根或多根颈神经根受压和/或受刺激引起的一侧或双侧上肢放射性疼痛的退行性疾病,其主要致病因素是突出髓核和增生的骨赘对神经根的压迫[7-8]。近年来,随着人们生活方式的变化,CSR呈现增长的趋势。长期以来,该病多以保守治疗为主[7],但近年来随着诊断水平提高及技术水平提升,对存在上肢顽固性疼痛、肌力减退且经保守治疗无效CSR患者近年多行手术治疗[9]。
临床上主要根据患者的临床症状、致压物、术者的习惯来选择具体术式。颈椎前路手术的目的在于彻底解除神经根的压迫以及稳定颈椎[10-12]。颈椎后路手术是通过扩大椎管及椎间孔、解除神经根的压迫来缓解患者症状。然而,后路手术容易因广泛切除后路结构导致椎体不稳定,可能引起患者术后颈椎后凸畸形或因广泛软组织剥离增加颈椎轴性症状[13]。颈前路椎间盘切除融合术起于20世纪50年代,其原理是通过前入路切除病理性椎间盘、解除神经根的压迫达到治愈目的。颈前路椎间盘切除融合术包括两种最常用的方法,即1955年Robinson和Smith等描述的颈前路椎间盘切除取髂骨植骨融合术以及1958年Cloward等描述的颈前路椎间盘切除Cage植骨融合术。颈前路椎间盘切除融合术可以切除突出的椎间盘和椎体后缘增生骨赘,借以解除该节段及其紧邻之神经根、脊髓的压迫,同时,通过撑开植入髂骨或Cage可间接减压椎间孔、恢复颈椎前凸。对于单节段神经根型颈椎病具有良好的植骨融合率和临床效果。由于颈前路手术为直接减压,且术后颈部的轴性疼痛等并发症较少,目前更多采用前路手术治疗。
頸椎前路手术需要彻底去除神经根前方的压迫,如减压不够、神经根减压不充分,可导致症状残留,达不到患者预期疗效。颈前路充分减压不但需要足够的减压长度,而且需要足够的减压宽度,但过度向外减压有可能导致椎动脉的损伤[14]。据统计,医源性椎动脉损伤的发生率为0.3%~0.5%[15]。同时,过度减压还可能因硬膜向前侧移位引起神经根牵拉伤[16]。因此,在保证充分减压又安全的情况下,减压程度的确定对手术的成功有重要意义。然而,在实际工作中,由于过度担心因减压范围过大致椎动脉损伤引起致残甚至致死性并发症发生而导致对神经根减压不彻底、患者术后症状缓解不满意的现象更有可能发生。因此,对CSR患者前路减压术中正确判断减压程度十分必要。
目前颈椎前路手术治疗CSR的减压范围一直存在争议,大多数术者主要依靠临床经验或者个人习惯,并没有客观依据。文献报道颈前路减压的安全范围为距离椎体中线15~19 mm、距离椎体边缘不超过5 mm[17-19]。然而,由于个体差异,椎体大小不同、致压物大小、性质、部位的不同,减压范围也会不同。本研究回顾性随访了84例单节段单侧症状的CSR患者,根据随访时的临床疗效分为完全缓解组和未完全缓解组,发现两组患者术前神经根受压迫程度无明显差别,但术后随访时未完全缓解组患者MRI显示致压物残留较大,手术减压程度较差,这可能是引起术后临床疗效不满意的主要原因。
此外,颈椎神经根管内的压迫容易忽视,即使压迫面积并不大,也可能由于神经根躲避空间小而导致症状难以缓解。Ebraheim等[20]将颈椎间孔和颈神经沟分为3个区:内侧区(椎弓根区)、中间区(椎动脉孔区)和外侧区。内侧区与颈椎间孔相一致,该区与神经根型颈椎病的病因密切相关。Tanaka等[21]将内侧区分为入口区和出口区。陈学明等[22]在研究中将颈椎椎间孔内的压迫分为软性压迫、硬性压迫和混合性压迫,认为不同性质的压迫对手术疗效也有影响。
总之,颈椎前路手术是治疗CSR的有效手段,但部分患者术后症状的残留可能与术中减压不彻底有关,彻底减压不会明显增加术后并发症。
[参考文献]
[1] 李增春,陈德玉,吴德升,等.第三届全国颈椎病专题座谈会纪要[J].中华外科杂志,2008,46(23):1796-1799.
[2] 赵定麟.颈椎伤病学[M].上海:上海科技教育出版社,1994:160.
[3] Sun Y,Muheremu A,Yan K,et al. Effect of different surgical methods on headache associated with cervical spondylotic myelopathy and/or radiculopathy [J]. BMC Surg,2015,15(1):105.
[4] Tasiou A,Giannis T,Brotis AG,et al. Anterior cervical spine surgery-associated complications in a retrospective case-control study [J]. J Spine Surg,2017,3(3):444-459.
[5] Huskisson EC. Measurement of pain [J]. Lancet,1974,2(7889):1127-1131.
[6] Vernon H,Mior S. The neck disability index:a study of reliability and validity [J]. J Manipulmive Physiol Ther,1991,14(7):409-415.
[7] Truumees E,Herkowitz HN. Cervical spondylotic myelopathy and radiculopathy [J]. Instr Course Lect,2000,49:339-360.
[8] Ando T. Diagnosis and management of cervical spondylosis [J]. Rinsho Shinkeigaku,2012,52(7):469-479.
[9] Boyce RH,Wang JC. Evaluation of neck pain,radiculopathy,and myelopathy:imaging,conservative treatment,and surgical indications [J]. Instr Course Lect,2003,52:489-495.
[10] Nikolaidis I,Fouyas IP,Sandercock PA,et al. Surgery for cervical radiculopathy or myelopathy [J]. Cochrane Database Syst Rev,2010,20(1):CD001466.
[11] Schroeder GD,Kurd MF,Millhouse PW,et al. Performing an anterior cervical discectomy and fusion [J]. Clin Spine Surg,2016,29(5):186-190.
[12] Liu WJ,Hu L,Chou PH,et al. Comparison of anterior cervical discectomy and fusion versus posterior cervical foraminotomy in the treatment of cervical radiculopathy:a systematic review [J]. Orthop Surg,2016,8(4):425-431.
[13] Wang T,Wang H,Liu S,et al. Incidence of C5 nerve root palsy after cervical surgery:a meta-analysis for last decade [J]. Medicine(Baltimore),2017,96(45):e8560.
[14] Obermuller T,Wostrack M,Shiban E,et al. Vertebral artery injury during foraminal decompression in "low-risk" cervical spine surgery:incidence and management [J]. Acta Neurochir(Wien),2015,157(11):1941-1945.
[15] Schelfaut S,Verhasselt S,Carpentier K,et al. Subaxial rotational vertebral artery syndrome:resection of the uncinate process and anterior fusion can be sufficient:case report and review of the literature [J]. J Spinal Disord Tech,2015,28(2):66-70.
[16] Kim HJ,Nemani VM,Piyaskulkaew C,et al. Cervical radiculopathy:incidence and treatment of 1,420 consecutive cases [J]. Asian Spine J,2016,10(2):231-237.
[17] Geck MJ,Eismont FJ. Surgical options for the treatment of cervical spondylotic myelopathy [J]. Orthop Clin North Am,2002,33(2):329-348.
[18] Rao RD,Currier BL,Albert TJ,et al. Degenerative cervical spondylosis:clinical syndromes,pathogenesis,and management [J]. J Bone Joint Surg Am,2007,89(6):1360-1378.
[19] Siemionow KB,Neckrysh S. Anterior approach for complex cervical spondylotic myelopathy [J]. Orthop Clin North Am,2012,43(1):41-52.
[20] Ebraheim NA,An HS,Xu R,et al. The quantitative anatomy of the cervical nerve root grove and the intervertebral foramen [J]. Spine,1996,21(14):1619-1623.
[21] Tanaka N,Fujimoto Y,An HS,et al. The anatomic relation among the nerve roots,intervertebral foramina,and intervertebral discs of the cervical spine [J]. Spine,2000,25(3):286-291.
[22] 陳学明,冯世庆,许崧杰,等.神经根型颈椎病椎间孔内神经根受压的原因分析及减压方式选择[J].中国脊柱脊髓杂志,2015,25(2):103-108.
