Immunotherapy in colorectal cancer: Available clinical evidence,challenges and novel approaches
2019-08-20JosephTintelnotAlexanderStein
Joseph Tintelnot, Alexander Stein
Abstract In contrast to other tumor types, immunotherapy has not yet become a relevant part of the treatment landscape of unselected colorectal cancer. Beside the small subgroup of deficient mismatch repair or microsatellite instable tumors (about 5%) as a surrogate for high mutational burden and subsequently high neoantigen load and immunogenicity, inhibitors of programmed death 1 (PD-1),programmed death ligand 1 (PD-L1) and/or cytotoxic T lymphocyte-associated antigen-4 were not or only modestly effective in metastatic colorectal cancer.Thus, a variety of combination approaches with chemotherapy, targeted therapy,toll-like receptor agonists, local ablation or oncolytic viruses is currently being evaluated in different disease settings. Despite several encouraging single arm data already presented or published, available randomized data are unimpressive. Adding PD-1/PD-L1 inhibitors to fluoropyrimidines and bevacizumab maintenance showed no beneficial impact on delaying progression.In refractory disease, the combination of PD-1/PD-L1 and MEΚ inhibitor was not different from regorafenib, whereas a PD-1/PD-L1 and cytotoxic T lymphocyteassociated antigen-4 inhibitor combination demonstrated better overall survival compared to supportive care alone. Clinical trials in all disease settings applying different combination approaches are ongoing and may define the role of immunotherapy in colorectal cancer.
Key words: Immunotherapy; Combination; Colorectal cancer; Metastatic; Adjuvant
INTRODUCTION
The first clinical evidence for the effectiveness of immunotherapy in solid tumors dates back to 1891 when Coley et al[1]first injected streptococcal bacteria into patients with inoperable sarcomas and observed shrinkage of some tumors. Despite this early success it took over a century and the breakthrough discovery of immune checkpoints, namely programmed death 1 (PD-1), programmed death ligand 1 (PDL1) and cytotoxic T lymphocyte-associated antigen-4 (CTLA-4), to relevantly change the treatment of different malignancies like melanoma, renal, bladder and lung cancer or Hodgkin’s disease. This breakthrough discovery was recently rewarded by the Nobel Prize for James P Allison and Tasuku Honjo in 2018.
In metastatic colorectal cancer (MCRC), only a minority of patients respond to immune checkpoint inhibition[2]. However patients who had a high tumor mutational burden and a high infiltration of T cells expressing checkpoint receptors (e.g., PD-1,PD-L1 or CTLA-4) mainly found in the subset of mismatch repair-deficient (dMMR)tumors with high levels of microsatellite-instability (MSI-H) responded to the immunotherapy[3-5]. Intriguingly, activated T cells directly recognized neoantigens that evolved from somatic mutations in gastrointestinal malignancies[6]or melanoma[7,8].The highest rates of neoantigen load were observed in frameshift mutated tumors through insertions or deletions[9].
In an attempt to define molecular subgroups of CRC, dMMR and MSI-H tumors cluster into the consensus molecular subtype (CMS) 1 of CRC[10], named as the immune subtype due to the high infiltration of lymphocytes. However, some CMS1 CRCs show a proficient mismatch repair (pMMR) system but harbor polymerase proofreading domain mutations that lead to even greater tumor mutational burden.Therefore they may be susceptible to immunotherapy as well[11,12]. These findings led to the approval of both PD-1 inhibitors pembrolizumab and nivolumab for the treatment of dMMR or MSI-H treatment-refractory MCRC in 2017.
Immunotherapy has no relevance in the canonical (CMS2), metabolic (CMS3) or mesenchymal subgroup (CMS4) of CRC[13]. Therefore the majority of CRC patients will not respond to this therapy. Combinatorial strategies to enhance the immunogenicity and infiltration by lymphocytes (e.g., combination with EGFR antibodies, radiotherapy, oncolytic viruses, adoptive cell therapy, tyrosine kinase inhibitors or toll-like receptor (TLR) agonists) have been recently addressed although their clinical relevance has yet to be determined. The present article summarizes current clinical evidence of immunotherapy in CRC and reviews ongoing clinical challenges and novel approaches. Published clinical data from PubMed, ESMO(Annual Symposium, World Congress on Gastrointestinal Cancer) and ASCO(Annual Meeting, Gastrointestinal Cancers Meeting) have been systematically collected and reviewed for the years 2012-2019.
IMMUNOTHERAPY IN DMMR/MSI-H MCRC
Monotherapy with PD-1 inhibitors (pembrolizumab or nivolumab)
The first interim data reported from the ΚEYNOTE (ΚN)-016 trial of pembrolizumab in treatment-refractory dMMR/MSI-H MCRC showed an overall response rate (ORR)of 40% (n = 10) in comparison to a missing response in pMMR or microsatellite stable(MSS) tumors (n = 18)[5]. In total, 40 MCRC patients (dMMR/MSI-H) were treated in ΚN-016 as part of 86 patients (dMMR/MSI-H) with 11 tumor types that led to the first ever agnostic (i.e. histology and tumor-site independent) approval of a cancer drug in 2017 in the United States[14]. The second cohort came from a part of the Check-Mate(CM)-142 phase II clinical trial with 74 MCRC patients (dMMR/MSI-H) after at least one prior systemic treatment who were treated with nivolumab. This trial led to the approval of nivolumab in 2017 in the United States[15]. These studies together with data from 61 treatment-refractory MSI-H patients (ΚN-164)[16]provided the current clinical evidence for treating dMMR/MSI-H MCRC patients with PD-1 inhibitors. An ORR of 31% in CM-142 or 28% in ΚN-164 were observed. Strikingly, progression free survival (PFS) at 12 mo was high with 50% and 34%, respectively as well as 1-year overall survival (OS) of 73% and 72%, respectively. Although generally well tolerated,the clinical response came at a cost of all grade drug-related adverse events (AEs) like fatigue (23%), diarrhea (21%), pruritus (14%) or rash (11%). Increase in lipase (8%) or amylase (3%) were the most frequent observed grade 3 or 4 AEs[15].
Combination of PD-1 (nivolumab) and CTLA-4 inhibitors (ipilimumab)
Recent evidence for the combination of nivolumab and ipilimumab in MCRC patients(dMMR/MSI-H) came from two further cohorts of the CM-142 study. In the treatment refractory cohort comprising of 119 patients with at least two prior therapies, an ORR of 55% and a 12-wk disease control rate of 80% were reported. Moreover, PFS rates of 71% and OS of 85% after one year were reached independent of ΚRAS or BRAF mutational status, PD-L1 tumor expression or family history of Lynch syndrome.Although no randomized data is currently available, ORR of 55% and 1-year OS of 85% compares favorably to an ORR of 31% and 1-year OS of 72% in single-agent PD-1 inhibitor treatment. Despite the expected increase in treatment-related AEs that occurred as grade 3 or 4 AEs in 32% of all patients, all AEs were manageable in the chosen regimen of nivolumab (3 mg/kg week 1 and every 2 wk from week 13) and ipilimumab (1 mg/kg on week 1, 4, 8 and 11). Recently, a third cohort with 45 previously untreated dMMR/MSI-H MCRC patients was reported showing an ORR of 60% (27/45), 1-year PFS of 77% and 1-year OS of 83%[17]. Notably, a low dose ipilimumab regimen was applied with 1 mg/kg every 6 wk continuously in combination with nivolumab 3mg/kg every 2 wk resulting in a very low rate of treatment-related grade 3/4 AEs of 16%.
In the nonmetastatic setting, 4 wk of neoadjuvant treatment with nivolumab 3 mg/kg (day 1 and 15) and ipilimumab 1 mg/kg (day 1) was tested in seven dMMR/MSI-H (stage II and III) CRC patients[18]. Four out of those seven patients showed non-vital tumor cells after resection whereas all remaining patients showed relevant downstaging and histological regression of their tumors (1%-2% vital tumor cells). Although limited by the small number, this dramatic pathological regression after 4 wk of treatment questions the objective response rates determined by imaging with checkpoint inhibition in dMMR/MSI-H MCRC. Data for selected PD-1 inhibitor+/- CTLA-4 inhibitor trials are displayed in Table 1.
Combination of PD-L1 inhibitor (atezolizumab) with anti-angiogenic VEGF-antibody(bevacizumab)
The combination of PD-L1 inhibitors and anti-angiogenic antibody bevacizumab showed favorable results in renal cancer. Recently, this combination was tested in ten dMMR/MSI-H MCRC patients in a phase Ib study. The combination was well tolerated and disease control was reached in 90% of patients with an ORR of 30%[19].
Ongoing clinical trials
A phase III study is currently observing the combination of atezolizumab, 5-fluorouracil, folinic acid and oxaliplatin (FOLFOX) in the adjuvant setting of stage III lymph node metastasized CRC (ATOMIC trial-NCT02912559). In MCRC, the ΚN-177 trial is investigating the addition of pembrolizumab to the first line standard of care therapy with FOLFOX or 5-fluorouracil, folinic acid and irinotecan alone or in combination with bevacizumab or cetuximab (NCT02563002). After completing the recruitment, results are expected this year. Furthermore, another phase II study is evaluating FOLFOX and bevacizumab and/or atezolizumab compared to FOLFOX and bevacizumab in the first line treatment of CRC (NCT02997228). In the second line treatment setting, the FFCD SAMCO trial is investigating the PD-L1 inhibitor avelumab compared to standard chemotherapy (NCT03186326).
IMMUNOTHERAPY IN PMMR/MSS MCRC
Monotherapy or combination of PD-1 (nivolumab and pembrolizumab) or PD-L1(durvalumab) inhibitors and CTLA-4 (ipilimumab and tremelimumab) inhibitors
The above mentioned studies (ΚN-016 and CM-142) that evaluated pembrolizumab(ΚN-016) or the combination of nivolumab and ipilimumab (CM-142) also included some pMMR/MSS MCRC patients[5,15]. In contrast to the appealing results in dMMR/MSI-H MCRC, pMMR/MSS MCRC patients did not respond to checkpoint inhibition, highlighting the predictive value of the dMMR/MSI-H status.
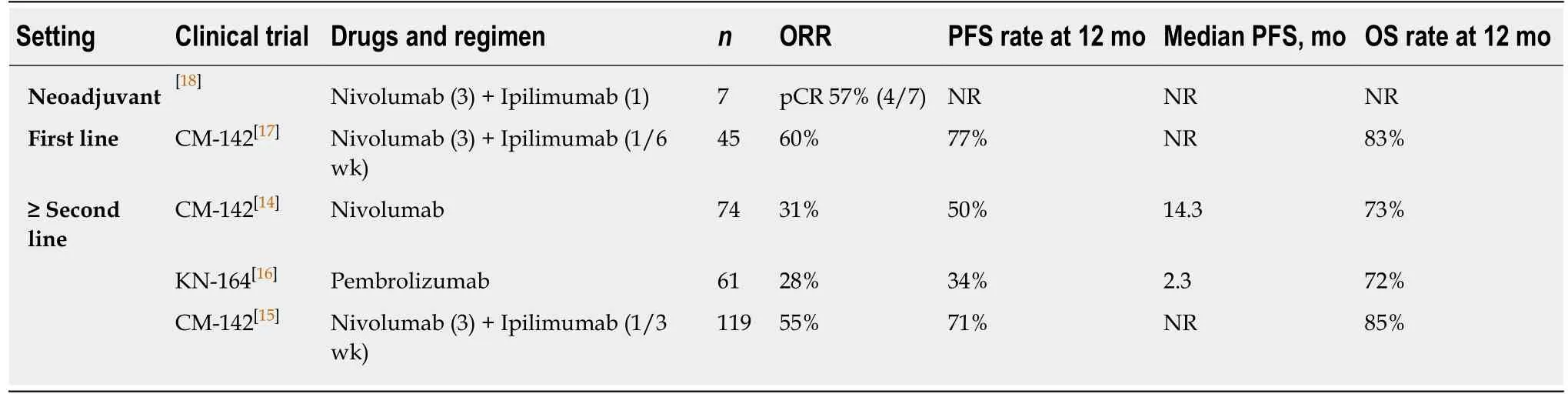
Table 1 Selected trials on immunotherapy in mismatch repair-deficient/microsatellite-instability metastatic colorectal cancer
A phase I study further evaluated the combination of durvalumab (PD-L1) and tremelimumab (CTLA-4) in 18 unselected MCRC patients. Although an ORR of 11%(2/18) was observed results can hardly be interpreted due to missing MMR/MSIstatus[20]. Recently, a randomized trial comparing best supportive care +/-durvalumab and tremelimumab in 180 patients, excluding patients with known MSIH status, was presented[21]. Despite similar ORR and PFS, OS was improved [4.1 vs 6.6 mo, hazard ratio: 0.72, 90% confidence interval: 0.54-0.97], reawakening the interest in this combination in pMMR/MSS MCRC.
COMBINATION STRATEGIES TO ENHANCE IMMUNOGENICITY IN PMMR/MSS OR UNSELECTED MCRC PATIENTS
As indicated by the results of the above-mentioned clinical studies, response to checkpoint inhibition is restricted to dMMR and MSI-H tumor patients.Unfortunately, this subset of patients only accounts for approximately 5% of MCRC cases. Because of the infiltration and activation of T cells, the recognition of neoantigens or tumor associated antigens has led the way to effective immunotherapy of solid tumors. Different combinatorial studies have been conducted or are still ongoing with the ultimate goal to enhance immunogenicity of CRC.
Checkpoint inhibition and local ablation
The abscopal effect was first described by Mole in 1953[22]as a phenomenon observed by local radiation of immunogenic tumors (renal cell carcinoma, melanoma or hepatocellular carcinoma) that led to shrinkage of distant tumors through the activation of immune effector cells[23]. It is unknown whether non-immunogenic tumors like CRC respond in a similar fashion. However, local ablation or radiotherapy may lead to cell death and the release of antigens and type I interferon,which induces maturation of dendritic cells and activation of CD8+T cells[24].
A small phase II clinical study used radiotherapy or radiofrequency ablation in addition to pembrolizumab in heavily pre-treated MCRC patients. Unfortunately, the ORR was as low as 5%. Similarly, an approach using a PD-L2-Fc fusion protein in combination with radiotherapy did not result in a relevant response[25]. Still, the dual checkpoint inhibition with durvalumab (PD-L1) and tremelimumab (CTLA-4)combined with local ablation is currently being evaluated in the EORTC ILOC phase II study (NCT03101475).
Checkpoint inhibition with chemotherapy +/- VEGF-inhibitor (bevacizumab) or EGFR-antibody (cetuximab)
The induction of immunogenic cell death by oxaliplatin or changes in the immune contexture by 5-fluouracil showed synergistic effects with checkpoint inhibition in mice models of CRC[26]. Further, the addition of the EGFR antibody, cetuximab may lead to antibody dependent cellular cytotoxicity[27], and anti-angiogenic treatment with bevacizumab may lead to favorable changes in the microenvironment[28]. A combination of pembrolizumab (PD-1) with chemotherapy FOLFOX in 30 MCRC patients (including 3 MSI-H patients)[29]resulted in a 43% ORR and 16.9 mo PFS.Further, FOLFOX and VEGF-inhibitor bevacizumab in combination with atezolizumab (PD-L1) led to a 52% ORR and 14.1 mo PFS in 23 patients[30].
However, the addition of atezolizumab to maintenance therapy with fluoropyrimidines and bevacizumab after 3-4 mo induction treatment with FOLFOX and bevacizumab did not result in an improvement of PFS [7.2 mo in the experimental arm vs 7.4 mo in the control arm (hazard ratio: 0.96, 95% confidence interval: 0.77-1.20), measured from randomization] (MODUL study, NCT02291289)[31]after median follow up of 18.7 mo. In total 445 MCRC patients (BRAF wildtype) were included and randomized (2:1 for atezolizumab treatment) in the largest randomized trial on immunotherapy in MCRC. Notably, OS curves split late after a similar median of 22.1 versus 21.9 mo resulting in a hazard ratio of 0.86 (95% confidence interval: 0.66-1.13).
Interesting results came from a single arm trial in the first line treatment of MCRC of applying an upfront combination of avelumab (PD-L1) with FOLFOX and the EGFR antibody cetuximab. An interim ORR of 75% in the first 20 patients[32]has been reported. Further clinical trials will evaluate the combination of avelumab and cetuximab in first line treatment setting or in the advanced disease setting with 5-fluorouracil, folinic acid and irinotecan (planned FIRE 6 study)[33].
Checkpoint inhibitors with tyrosine kinase inhibitors
In preclinical studies, enhanced T cell infiltration, upregulation of major histocompatibility complex and activation of antigen presenting cells was seen by combining MEΚ-inhibitors with PD-1/PD-L1 inhibitors[34,35]. In line with these results,a phase Ib study showed meaningful results using the combination of cobimetinib(MEΚ inhibitor) and atezolizumab (PD-L1) in 20 pretreated ΚRAS mutated MCRC patients with an ORR of 20% (4/20)[36]. However, the consecutive phase II clinical trial(IMblaze 370) did not show any difference in comparison to regorafenib (tyrosine kinase inhibitor) alone[37]. Although results from the maintenance treatment with cobimetinib and atezolizumab in comparison to 5-fluouracil and bevacizumab after 3-4 mo of FOLFOX treatment (MODUL study-NCT02291289) are still pending, the combination of MEΚ inhibitors with checkpoint inhibition is not expected to enter clinical use due to results from the IMblaze 370 trial.
TLR agonists
The innate immune system and especially dendritic cells are critical to mount proper immune responses under immune checkpoint inhibition[38]. TLR agonists stimulate the maturation of dendritic cells and account for the production of pro-inflammatory cytokines like IFN- This stimulates the adaptive immune system[39]. The IMPALA study (NCT02077868) evaluated maintenance treatment with MGN1703 (TLR-9 agonist) in comparison to investigator choice after at least stable disease following first line standard induction. Despite promising preliminary results from a single arm phase II study[40], results from the confirmatory IMPALA study are still pending.
Checkpoint inhibition and oncolytic viruses
A variety of viruses termed oncolytic viruses are used in clinical trials to specifically lyse tumor cells and stimulate the anti-cancer immune reaction, thereby acting as an in situ tumor vaccine[41]. Heavily pretreated CRC patients were treated with the oncolytic vaccinia virus (engineered to express GM-CSF, a hematopoietic growth factor that increases dendritic cell differentiation, maturation and function and induced tumor reactive T cells[42]and β-galactosidase) and reached stable disease in 67% (n = 10) of patients. The biweekly injection did not lead to dose-limiting toxicities in this phase Ib study alone[43]or in a phase I/II study in combination with checkpoint inhibitors tremelimumab (CTLA-4) and durvalumab (PD-L1)[44]. As seen in melanoma[45], the combination with checkpoint inhibitors further promises an increase in effectiveness. However, the first results using the combination of the vaccinia virus with checkpoint inhibitors are still pending (NCT03206073).
Adoptive cell therapy
In 2017, the FDA licensing of two chimeric antigen receptor (CAR) T cell products targeting CD19 for the treatment of acute refractory leukemia in children and B cell lymphoma in adults opened the field of adoptive cell therapy in clinical use.However, treatment of solid tumors is much more challenging due to limited trafficking and persistence of T cells into the tumor and an immunosuppressive environment[46,47]. Evidence for the impact of adoptive cell therapy in CRC comes from isolation, ex vivo expansion and re-infusion of tumor infiltrating lymphocytes[48].Despite this elaborate work some quite encouraging results have been obtained. For example, after re-infusion of tumor reactive lymphocytes from tumor draining lymph nodes of MCRC patients an increase in OS from 14 mo (control, n = 16) to 28 mo (n =9) was observed, although statistical significance was not reached[49]. More specifically,Tran et al[50]isolated, expanded and reinfused polyclonal CD8+ T cells from metastatic lung lesions of a MCRC patient reactive against mutant ΚRAS G12D. Subsequently six out of seven lung metastasis were eradicated with one remaining that lost the chromosome 6 haplotype to escape reactive T cells.
Another approach transferring ex vivo expanded natural killer cells after treatment with IgG1 antibodies trastuzumab (HER2) or cetuximab (EGFR) and chemotherapy was well-tolerated, showed anti-tumor immune induction, and preliminary antitumor activity. Stable disease was observed in 67% (n = 6) of patients with advanced gastric or CRC[51].
CAR T cells in CRC are limited to the target antigen because tumor specific neoantigens are promising but not conserved between different patients. Tumorassociated antigens like CEA, EGFR or MUC1 are rather unspecific and could lead to AEs as seen by one death induced by ERBB2-specific CAR T cells[52]or respiratory toxicity by CEACAM5-specific CAR T cells[53]. However, the ERBB2-related death may have been due to the use of an excessive number of CAR T cells because ERBB2-specific CAR T cells were recently proven safe in sarcoma patients[54]. These potential toxicities in addition to the complex production of CAR T cell products further limit the breakthrough in CRC (despite the clinical potential that was validated for CEAspecific CAR T cells after percutaneous intra-artery infusion in a phase I study with an average decrease in CEA levels of 37% in 3 patients with high hepatic metastatic burden)[55]. In essence, CAR T cells, transfer of tumor infiltrating lymphocytes or natural killer cells are not yet ready for clinical use, but phase I or II studies may open up new avenues for future developments and are reviewed elsewhere[48].
FUTURE DEVELOPMENT
Future treatment strategies using immunotherapy to treat CRC will integrate the everimproving knowledge about the molecular mechanisms that exclude or dampen the immune response in MCRC. Immune signatures revealed that TGF-β signaling is key in the development of CMS4 CRC and led to enhanced tumor metastatic capacities[13].Preclinical models could show that targeting TGF-β can reset this immune excluding phenotype and may restore susceptibility to checkpoint inhibition[56]. Therefore, it presents an interesting target in future immune oncology of CRC.
Other promising strategies to target the “cold” lymphocyte excluded tumor microenvironment of pMMR/MSS CRC like chemotherapy, targeted therapy,oncolytic viruses, local ablation or TLR agonists already show some promise in early clinical or pre-clinical studies in combination with checkpoint inhibitors but are not yet ready for clinical use. Novel checkpoints like LAG-3[57]may further add to the arsenal of immune oncology in MCRC.
Together, targeting the immune exclusive microenvironment and the quality of tumor reactive T cells of pMMR/MSS CRC is promising, but most approaches still have to find their way from pre-clinical to clinical use. Therefore, approaches that combine already licensed targeted treatments, e.g., EGFR-antibodies or VEGFantibodies, and chemotherapy with checkpoint inhibitors might enter clinical use earlier if results can be confirmed.
杂志排行
World Journal of Gastroenterology的其它文章
- Improving cirrhosis care: The potential for telemedicine and mobile health technologies
- Lumen-apposing metal stents for malignant biliary obstruction: Is this the ultimate horizon of our experience?
- Pharmacogenetics of the systemic treatment in advanced hepatocellular carcinoma
- Consensus on management of hepatitis C virus infection in resource-limited Ukraine and Commonwealth of Independent States regions
- Hepatocellular carcinoma in the post-hepatitis C virus era: Should we change the paradigm?
- Honokiol-enhanced cytotoxic T lymphocyte activity against cholangiocarcinoma cells mediated by dendritic cells pulsed with damage-associated molecular patterns
