Systemic Vasculitis:An Important and Underestimated Cause of Malignant Hypertension
2019-08-12QingZhuMDShashaLiuMDMulalibiekeHeizhatiMDXiaoguangYaoPhDMenghuiWangMDQinLuoMDLeiWangMDDelianZhangPhDGuijuanChangMDandNanfangLiPhDMD
Qing Zhu,MD ,Shasha Liu,MD ,Mulalibieke Heizhati,MD ,Xiaoguang Yao,PhD ,Menghui Wang,MD ,Qin Luo,MD ,Lei Wang,MD ,Delian Zhang,PhD ,Guijuan Chang,MD and Nanfang Li,PhD,MD
1 The Center for Hypertension of the People' s Hospital of Xinjiang Uygur Autonomous Region,Hypertension Institute of Xinjiang Uygur Autonomous Region,Urumqi,China
Abstract
Objectives: Malignant hypertension (MHT) is defined as severe hypertension accompanied by ischemic failure of one or more organs.The aims of this study were to evaluate the current clinical and etiologic profiles of MHT.
Methods: As a retrospective study,we selected all patients admitted to our center from January 2013 to December 2016.Seventy patients with MHT were included.
Results: The average age of the patients was 40 years,and more than half of the patients were male (78.57%).There were 24 patients with essential hypertension,accounting for 34.29% of the patients,and 46 with secondary hypertension,accounting for 65.71% of the patients.For secondary MHT,systemic vasculitis (25.57%) was the most common cause,followed by severe obstructive sleep apnea syndrome (15.71%),primary renal parenchymal hypertension (11.43%),primary aldosteronism (7.14%),and Cushing syndrome (1.43%) and nutcracker phenomenon (1.43%).Twenty patients with systemic vasculitis were characterized by severe hypertension accompanied by damage to two or more target organs of differing severity.The levels of white blood cells,hypersensitive C-reactive protein,serum creatinine,and 24-hour urinary protein were above their normal range.
Conclusion: Systemic vasculitis may be one of the main causes of MHT,and has been underestimated in the past.In future clinical work,clinicians need to pay more attention to patients with systemic vasculitis.
Keywords: malignant hypertension;cause;systemic vasculitis
Introduction
Malignant hypertension (MHT) is a condition characterized by severe hypertension and can cause retinal,neurologic,renal,and cardiac complications.If MHT is not treated,mortality is very high,the 2-year mortality being 80% [1].Despite the availability of a vast range of antihypertensive agents,MHT continues to be a significant clinical challenge.Although its prevalence is very low,the absolute number of new cases has not changed in recent decades [2 ,3].Since the clinical manifestations of MHT are not specific,when patients present with acute renal failure the underlying causes of MHT are difficult to identify.Generally,the causes of MHT are primary or secondary hypertension.A few studies showed that about 1- 5% of cases of essential hypertension may develop into MHT [4] because of patients not taking antihypertensive medications or abruptly stopping taking antihypertensive medications.For the secondary causes of MHT,some clinical case reports and studies showed that such secondary hypertension can lead to MHT as in primary aldosteronism (PA),pheochromocytoma,Cushing syndrome,obstructive sleep apnea syndrome (OSAS),renal hypertension (including renal vascular hypertension),hypothyroidism,and pregnancy [5 - 10].Recent studies have indicated that the immune system may also play an important role in the development of this condition [11].There is an increasing amount of literature on vasculitis indicating that various types of vasculitis can also cause MHT [12- 14].Therefore,our aims were to evaluate the current clinical and etiologic profiles of MHT.
Participants and Methods
Ethics Approval of the Study Protocol
This study was approved by the Ethics Committee of the People' s Hospital of Xinjiang Uygur Autonomous Region (Urumqi,China).It was conducted according to the standards of the Declaration of Helsinki.
Participants
We reviewed all patients admitted to our center for screening for the cause of hypertension between January 2013 and December 2016.Our hypertension center is the biggest hypertension center in China,and has 180 inpatient beds.Thousands of patients are referred to the center from all over China each year,and we have successfully identified the cause of secondary hypertension in more than 10,000 patients.Of these patients,some were found to have high blood pressure through physical examination,some had headache,dizziness,palpitation,fatigue,and other uncomfortable symptoms,and some appeared to have experienced stoke,myocardial infarction,chronic renal insufficiency,and other complications due to long-term hypertension.So they were admitted to our center.
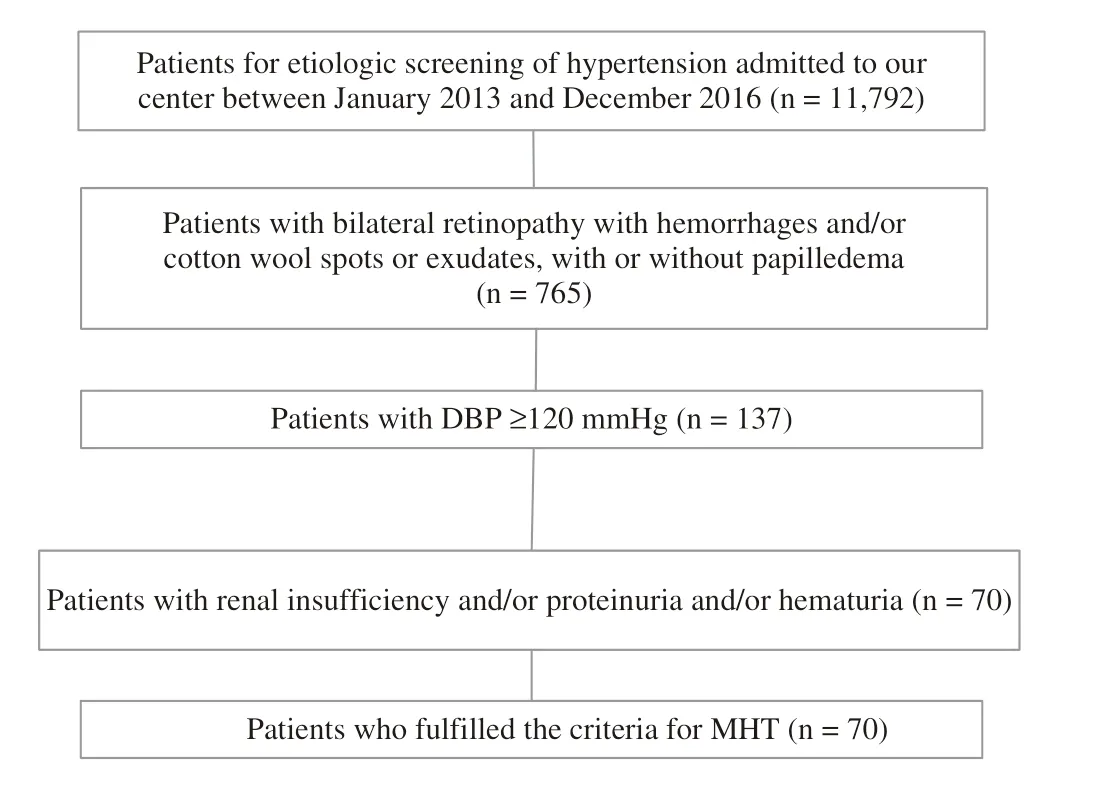
Figure 1 Flow Chart of Patients with Malignant Hypertension (MHT).
We selected patients who fulfilled the criteria for MHT,including (1) elevated diastolic blood pressure ( ≥ 120 mmHg),(2) presence of grade III or IV hypertensive retinopathy (bilateral retinopathy with hemorrhages and/or cotton wool spots or exudates,with or without papilledema),and (3) renal complications (increased creatinine concentration and/or proteinuria and/or hematuria) ( Figure 1).Patients younger than 18 years,pregnant women,and patients who were already undergoing dialysis before admission were excluded.
Diagnostic Criteria
Essential Hypertension
Patients were considered to have essential hypertension if they fulfilled the criteria for the diagnosis of MHT and secondary hypertension was excluded.
Primary Aldosteronism
The screening of patients for and the diagnosis of PA were conducted by a standard process based on the current guidelines as in a previous study from our center [15].An elevated aldosterone level (>12ng/L) and suppressed plasma renin activity (<1.0μg/Lh) or an aldosterone-to-renin ratio (the ratio of plasma aldosterone concentration to plasma renin activity) greater than 20 ng/dL per nanogram per milliliter per hour was considered as PA.PA was confirmed by a saline loading test (postinfusion plasma aldosterone concentration > 5 ng/dL).
Cushing Syndrome
The diagnosis was on the basis of symptoms,signs,serum cortisol and ACTH levels and CT/MRI findings.The qualitative diagnosis and localization diagnosis of Cushing syndrome were according to the Endocrine Society guideline [16].
Primary Renal Parenchymal Hypertension
Hypertension was diagnosed after a history of renal disease and was confirmed by kidney biopsy,excluding secondary glomerular lesions.
Systemic Vasculitis
The diagnosis of systemic vasculitis was based on the patient ' s clinical manifestations (such as malaise,weight loss,fever,arthralgia,and myalgia),laboratory test results (such as elevated erythrocyte sedimentation rate and levels of C-reactive protein and other acute-phase reactants,proteinuria,hematuria,and increased creatinine concentration),and typical imaging findings (such as artery occlusion and stenosis or arterial saccular or fusiform microaneurysms) and pathologic biopsy findings (such as vascular wall thickening,bursal stenosis,surrounded by inflammatory cell infiltration,but the lack of immune complex deposition).Diagnosis was confirmed by a rheumatologist and was in accordance with the 1990 American College of Rheumatology (ACR) criteria or the revised 2012 Chapel Hill Consensus Conference (CHCC) nomenclature of vasculitis [17- 21].Systemic vasculitis,according to the CHCC definition,is divided into seven categories.It mainly includes large-vessel vasculitis [giant cell arteritis and Takayasu arteritis (TA)],mediumvessel vasculitis [Kawasaki disease and polyarteritis nodosa (PAN)],and small-vessel vasculitis [antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV),granulomatosis with polyangiitis (GPA),eosinophilic granulomatosis with polyangiitis (EGPA),and microscopic polyangiitis (MPA)].For the classification of PAN and other necrotizing vasculitides,we referred to the consensus algorithm that was proposed by combination of ACR and CHCC criteria,ANCA testing,and surrogate markers of vascular inflammation,including clinical,laboratory,neurophysiologic,and imaging tests ( Figure 2) [22].
Takayasu Arteritis
A patient was considered have TA if at least three of these six criteria:(1) age < 40 years,(2) claudication of an extremity,(3) decreased brachial artery pulse,(4) > 10 mmHg difference in systolic pressure between arms,(5) a bruit over subclavian arteries or aorta and (6) angiographic evidence of narrowing or occlusion of the aorta or its primary or proximal branches were present [17].The presence of three or more of these six criteria demonstrated sensitivity of 91% and specificity of 98%.
Polyarteritis Nodosa
A patient was considered to have PAN if at least three of these ten criteria:(1) Weight loss 24 kg;(2) Livedo reticularis;(3) Testicular pain or tenderness;(4) Myalgias,weakness,or leg tenderness;(5) Mononeuropathy or polyneuropathy;(6) Diastolic BP > 90 mmHg;(7) Elevated BUN or creatinine;(8) Hepatitis B virus;(9) Arteriographic abnormality;(10) Biopsy of small or medium-sized artery containing polymorphonuclear neutrophils were present [18].The presence of three or more of these ten criteria demonstrated sensitivity of 82.2% and specificity of 86.6%.
ANCA-Associated Vasculitis
The diagnosis was on the basis of symptoms,signs,laboratory indicators,detection of ANCA,and pathology examination according to the related criteria.“ ANCA-associated vasculitis” (AAV) is a collective term for three diseases:MPA,GPA,and EGPA.
Obstructive Sleep Apnea Syndrome

Figure 2 Consensus Algorithm Proposed by Watts et al.[22] for the Classification of Eosinophilic Granulomatosis with Polyangiitis (EGPA),Granulomatosis with Polyangiitis (GPA),Microscopic Polyangiitis (MPA),and Polyarteritis Nodosa (PAN).Findings typical of GPA include but are not limited to imaging evidence of fixed pulmonary infiltrated nodules or cavitations,bronchial stenoses,bloody nasal discharge and crusting,nasal ulceration,chronic sinusitis,otitis media or mastoiditis,retro-orbital mass,subglottic stenosis,and saddle-nose deformity.Findings typical of MPA include alveolar hemorrhage and hematuria associated with red cell casts or 10% dysmorphic erythrocytes or proteinuria.ACR,American College of Rheumatology;ANCA,antineutrophil cytoplasmic antibodies;CHCC,Chapel Hill Consensus Conference;MPO,myeloperoxidase:PR3,proteinase 3.(Adapted from [22]).
All patients with snore underwent full-night polysomnography.OSAS was defined as an apnea-hypopnea index (AHI) of more than five events per hour and was further subclassified into mild OSAS (AHI = 5- 15),moderate OSAS (AHI = 16- 30),and severe OSAS (AHI > 30).
Nutcracker Syndrome
The diagnosis of nutcracker syndrome was based on clinical examination,followed by Doppler ultrasonography and phlebography with measurement of the renocaval pressure gradient [23].
Data Collection and Measurements
All the clinical data came from the patients' medical records during hospitalization (including demographics and clinical,biological,imaging,and biopsy findings).
The following clinical manifestations were recorded:general symptoms (fever,weakness,asitia,myalgia and arthralgia,and weight loss);peripheral neuropathy (mononeuritis multiplex,or polyneuropathy);central nervous system involvement;urologic and renal involvement (orchitis,dialysis,peripheral limb edema,and recent-onset or severe hypertension);cutaneous symptoms (nodules,purpura,erythema,and livedo reticularis);alimentary manifestations (nausea,vomiting,abdominal pain,hemorrhage,pancreatitis,and peritonitis);cardiovascular involvement (pectoralgia,cardiomyopathy,pericarditis,and ischemia);ophthalmologic involvement (retinal vasculitis/exudates,visual impairment,conjunctivitis,keratitis,and uveitis);pulmonary involvement (cough,hemoptysis,dyspnea,pleural effusion,and lung infiltrates).
The biological parameters recorded were blood cell counts,renal parameters (proteinuria,hematuria,24-hour urinary protein level,and serum creatinine concentration),erythrocyte sedimentation rate,C-reactive protein level,hypersensitive C-reactive protein level,and the presence of ANCA as tested by indirect immunofluorescence and enzyme-linked immunosorbent assay.
The diagnosis of renal vascular hypertension,TA,and PAN mostly requires vascular ultrasonography,vascular CT angiography,or angiography.The angiography results were judged as abnormal when the blood vessels were sparse,there was irregular stenosis,and/or there were microaneurysms.The chest X-ray was judged as abnormal if it showed nodules,infiltrating lesions,and/or cavitation.The result was determined by two radiologists.
Biopsy is often required for the diagnosis of renal hypertension and small-vessel vasculitis.When hypertension from these two causes is considered,renal and/or skin biopsy should be performed for a clear diagnosis.Inflammatory cell infiltration and/or formation of a crescent was present in small-vessel and medium-vessel vasculitis.Immunofluorescence demonstrated no or little immune complex deposition in the mesangial area,vascular loops,or small vascular walls.The result was determined by two pathologists.
Statistical Analysis
Data analysis was performed with SPSS Statistics for Windows (version 17.0;SPSS,Chicago,IL,USA).All continuous variables are expressed as the mean ± standard deviation (for data that were normally distributed) or the median and interquartile range (for data that were not normally distributed).The frequencies of categorical data are presented as percentages.
Results
A total of 11,972 patients were admitted to our center between January 2013 and December 2016,and 70 patients fulfilled the criteria for MHT.The clinical characteristics of the patients with MHT are shown in Table 1.The average age was 40 years,and the patients were mainly male (78.57%).They had high blood pressure and a short disease course.Sixty-three patients had grade III hypertensive retinopathy and seven patients had grade IV hypertensive retinopathy.Besides renal involvement,most patients presented with cardiac and cerebrovascular complications.A detailed breakdown of the details of the 70 patients can be found online in the Supplementary Table S1.Table 2 shows the cause distribution for the 70 patients with MHT.Essential hypertension was diagnosed in 24 patients,accounting for 34.29% of the patients,while secondary hypertension was diagnosed in 46 patients,accounting for 65.71% of the patients.For secondary MHT,systemic vasculitis (25.57%) was the most common cause,followed by severe OSAS (15.71%),primary renal parenchymal hypertension (11.43%),PA (7.14%),and Cushing syndrome (1.43%) and nutcracker phenomenon (1.43%).Among the 20 cases of vasculitis,ten cases were PAN,four cases were TA,and six cases were AAV (including one case of GPA,two cases of EGPA,and three cases of MPA).
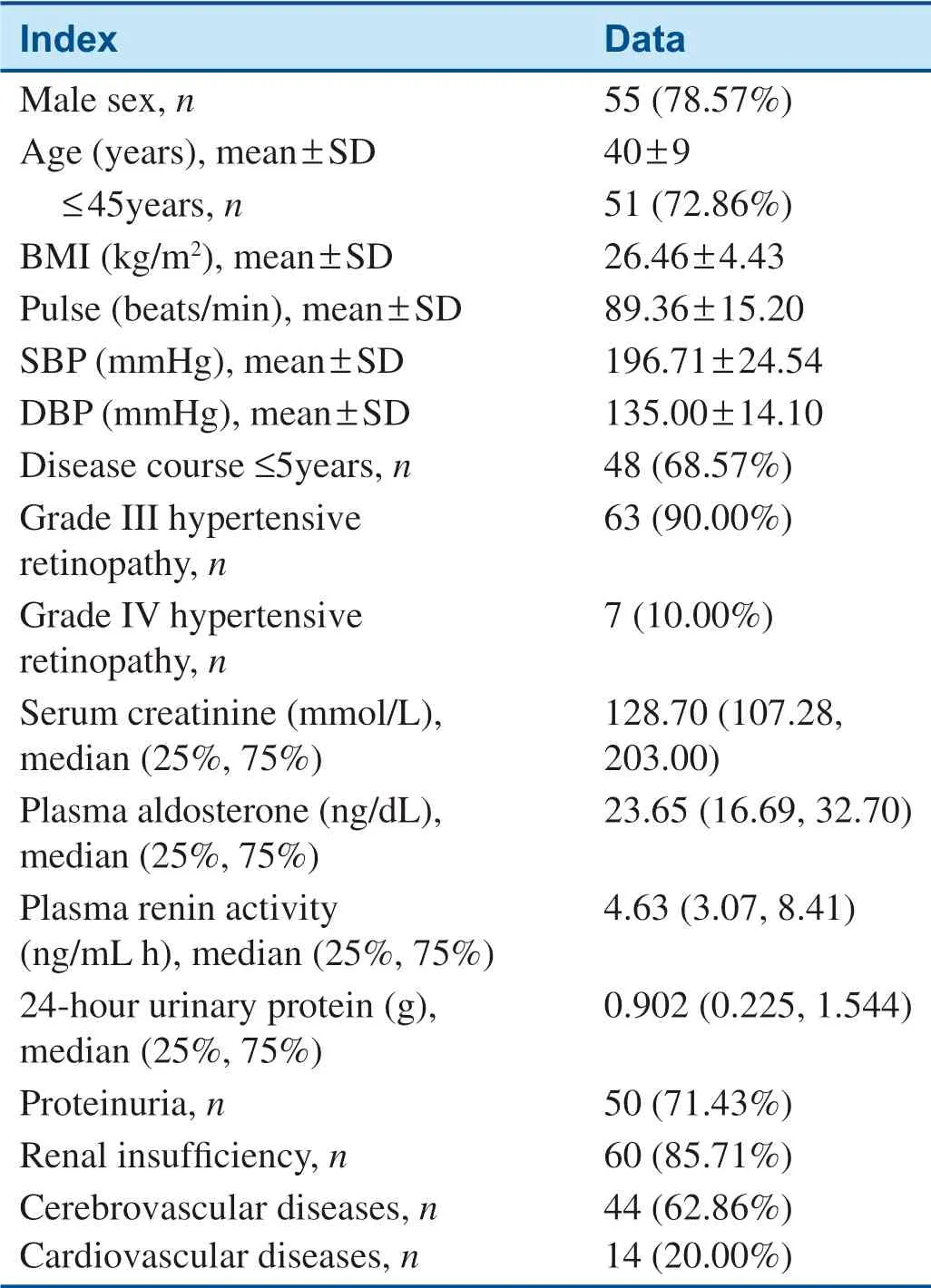
Table 1 Characteristics of 70 Patients with Malignant Hypertension.

Table 2 The Cause Distribution for 70 Patients with Malignant Hypertension.
From Table 3,we see that 20 patients with systemic vasculitis were characterized by severe hypertension accompanied by damage to two or more target organs of differing severity.Among the clinical manifestations,neurologic,cardiac,and renal manifestations were common.However,general symptoms,mainly weakness and weight loss,were present in 20% of patients.There were cutaneous manifestations (livedo reticularis,tender subcutaneous nodules) in 15% of patients.There were otolaryngologic manifestations,mainly rhinitis,sinusitis,tinnitus,and otitis media,in 40% of patients.
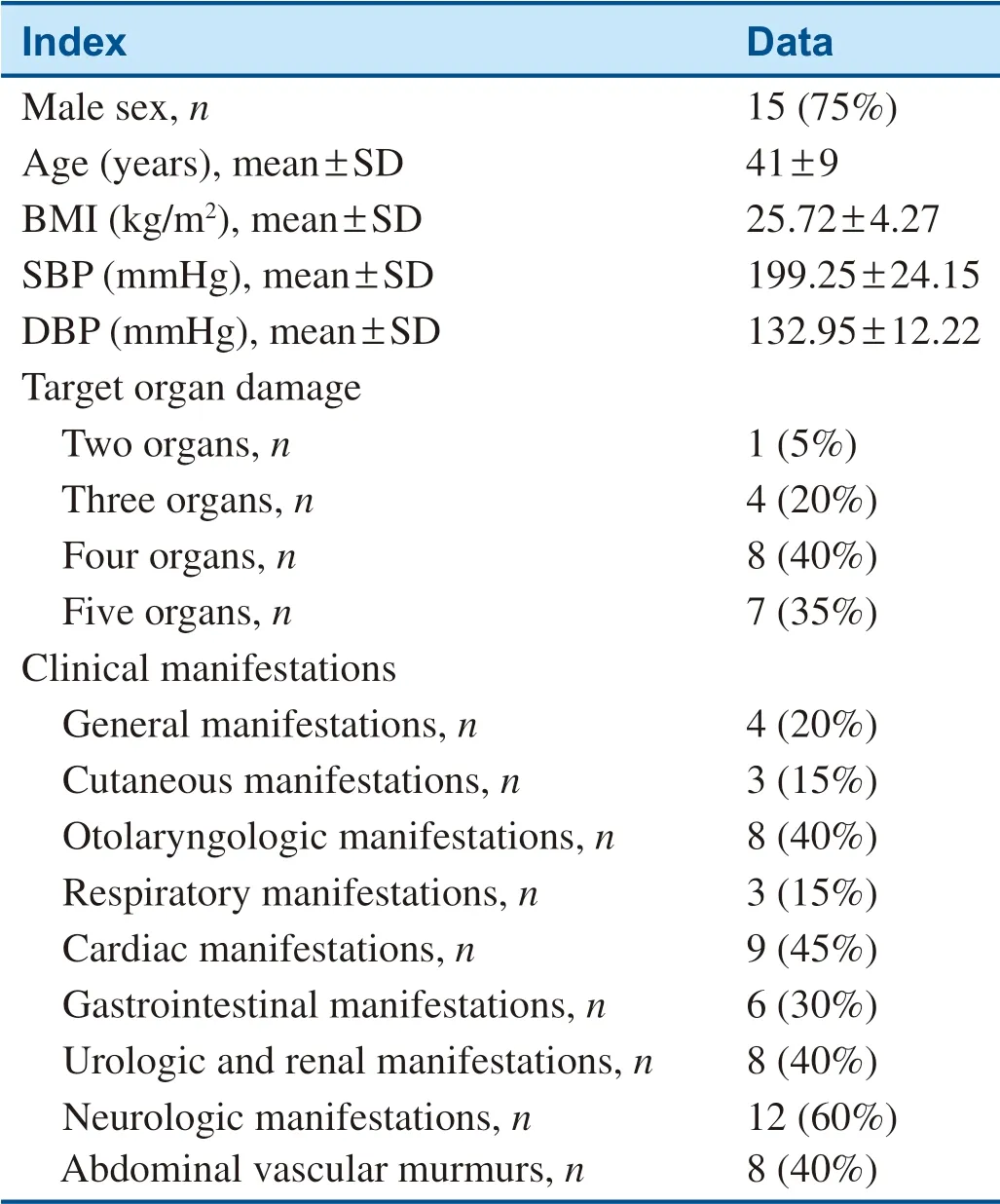
Table 3 The Clinical Features of 20 Patients with Systemic Vasculitis.
Table 4 shows the laboratory examination findings for 20 patients.The levels of white blood cells,hypersensitive C-reactive protein,serum creatinine,and 24-hour urinary protein were above their normal range.Other indicators were normal.
Discussion
MHT is the severest form of hypertension and is a lifethreatening condition.Although survival of MHT has considerably improved with the advent of antihypertensive medication,end-stage renal disease remains a significant cause of morbidity and death [24,25].In addition,there are the irregular treatment and lack of individualized treatment,whether there are other reasons for it.Patients often stop or discontinue taking the medicine by themselves because they have no discomfort or no money.Moreover,studies have suggested that some patients continue to develop progressive renal failure despite a good degree of blood pressure control [26].The reasons may be that the potential cause and the pathogenesis of MHT are not clear.While the roles of the activation of the renin-angiotensin-aldosterone system and endothelial dysfunction in the pathogenesis of MHT have been well described,recent studies have indicated that the immune system (particularly T cells) may also play an important role in the development of MHT and MHT-related kidney injury [4,27,28].They are coincident with the pathogenesis of systemic vasculitis.Systemic vasculitis is characterized by inflammation and damage of vessels,with a severe clinical course.Although the cause of vasculitis is unclear,some studies have shown that immune-mediated complement activation and endothelial dysfunction are responsible for its pathogenesis [29].Systemic vasculitis often mainly involves the skin,kidneys,lungs,nervous system,etc.,and has complex and varied clinical manifestations and causes multiple organ dysfunction in patients.When the kidneys are involved,systemic vasculitis can lead to hypertension (especially high diastolic blood pressure).Studies have shown that TA can lead to renal failure and renovascular hypertension in 60% of patients,PAN in 25% of patients,and AAV in 12% of patients.A recent single-center study showed that arterial hypertension is common during TA (45.8%) [30].In our study,for secondary MHT,most patients had a diagnosis of systemic vasculitis (43.48%).
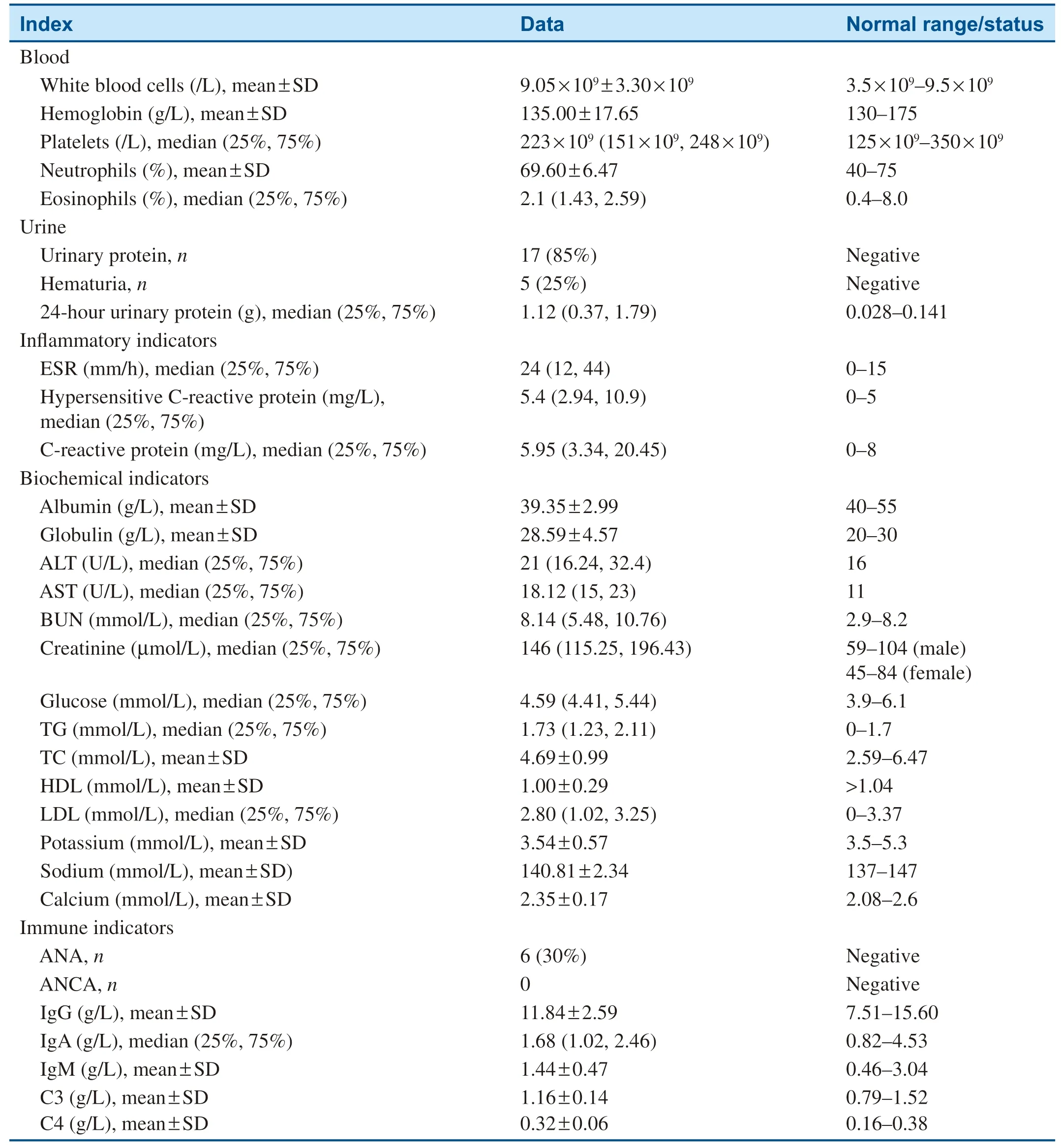
Table 4 Laboratory Examination Findings for 20 Patients.
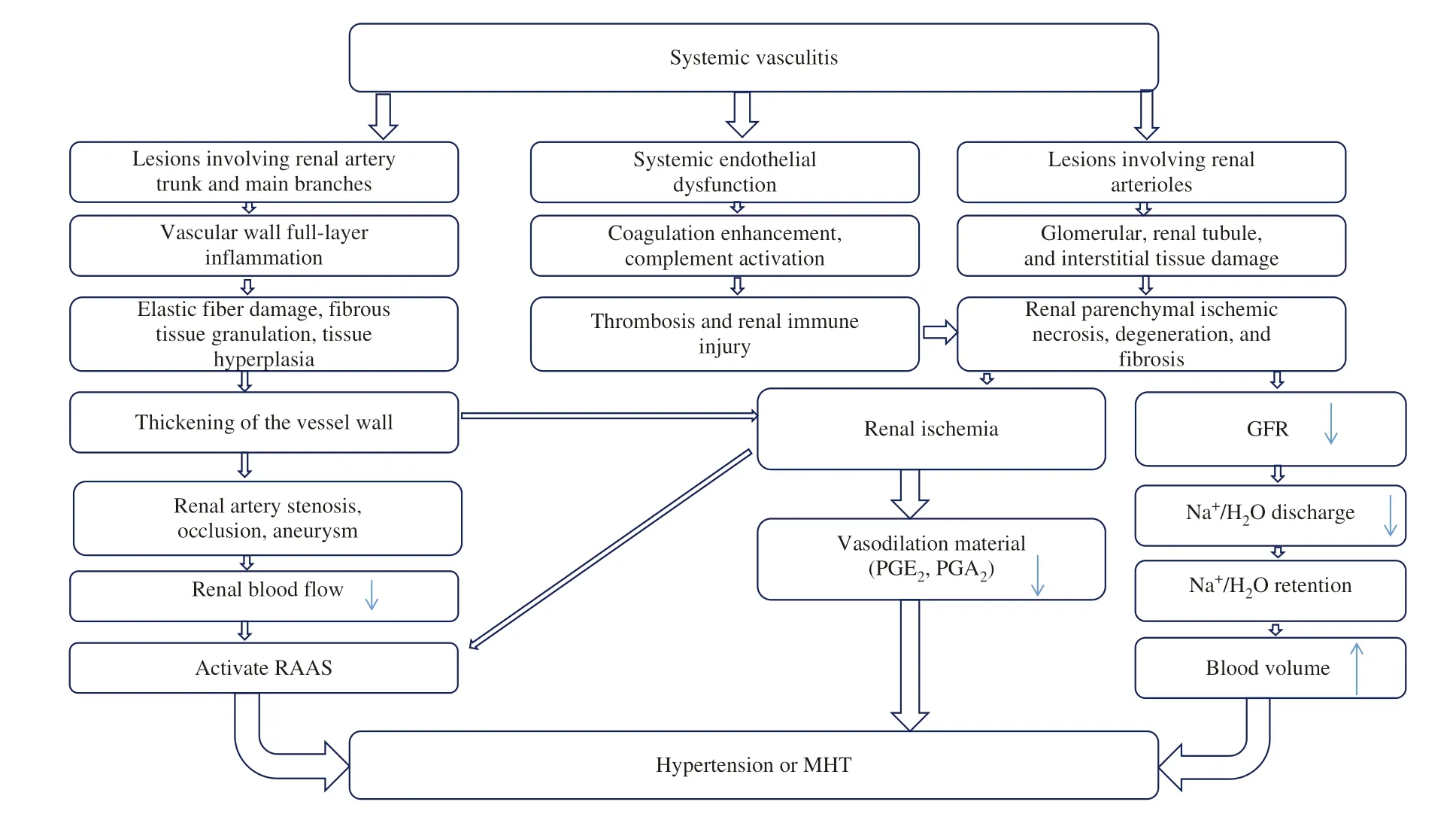
Figure 3 The Possible Pathophysiologic Mechanisms for the Development of Hypertension or Malignant Hypertension (MHT) by Vasculitis.
The pathophysiologic mechanisms for the development of hypertension or MHT by vasculitis are as follows:(1) large vascular lesions involving the renal artery trunk and main branches,which lead to renal artery stenosis and occlusion aneurysm,cause renal blood flow to decrease and activate the reninangiotensin-aldosterone system,thereby leading to high blood pressure,such as renal vascular hypertension caused by PAN,TA,etc;(2) small vascular lesions involving renal arterioles,which lead to damage of glomerular,renal tubule,and interstitial tissue,causing renal parenchymal ischemic necrosis,degeneration,and fibrosis,thereby reducing the glomerular filtration area and causing renal ischemia,leading to hypertension,such as renal parenchymal hypertension caused by allergic granulomatous vasculitis,microscopic poly angiitis,etc;(3) vascular endothelial cell damage,which leads to coagulation enhancement and activation of complement and immune regulation,results in thrombosis and renal immune injury,causing high blood pressure ( Figure 3).In addition,macrovascular lesions lead to narrowing of the aorta or the abdominal aorta,redistributed blood flow,and upper limb blood pressure significantly higher than lower limb blood pressure.Furthermore,the interaction of these mechanisms may result in higher blood pressure.
In the past,because of the lack of understanding of vasculitis,because the clinical manifestations and serologic markers of vasculitis were not specific,and because angiography and histopathology were limited by segmental and traumatic lesions,a large number of patients were often missed and there was misdiagnosis and delayed treatment.Because the pathologic characteristics of MHT (hyperplastic arteriolosclerosis and necrotizing arteriolitis,mainly involving the kidney) are similar to those of systemic vasculitis,especially small-vessel vasculitis,systemic vasculitis was not well identified in the hypertensive population.
Although uncommon,early diagnosis of systemic vasculitis is required to preserve the function of the affected organs and to decrease mortality.If systemic vasculitis is not diagnosed,evaluated,and treated properly,the outcome will be very poor.From the follow-up of our patients with vasculitis,there were five cases of adverse events (one death,one cerebral hemorrhage,one massive hemoptysis,one abdominal aortic aneurysm rupture,and one repeated fundus hemorrhage) in the 20 patients,and the prognosis was very poor.Therefore,if patients have unexplained renal atrophy,proteinuria,hematuria,deterioration of renal function,multiple organ involvement,increased inflammatory indexes,and/or antinuclear antibody and ANCA positivity,they should be highly suspected of having vasculitis.Together with skin,ear,nose,throat,eye,and other symptoms,these manifestations can help in the diagnosis of vasculitis.
Limitations
This is a single-center study in a hypertension center and so there might be some specialist bias.Because of the cross-sectional nature of the study,a causal relationship between MHT and vasculitis could not be determined.Some scholars consider that vasculitis reflects target organ damage caused by MHT or as a consequence of markedly elevated blood pressure,whereas others think the otherwise.However,because our center is a specialty center for secondary hypertension,most of the patients enrolled in this study were hospitalized because of markedly increased blood pressure with high levels of inflammatory factors,antinuclear antibody and ANCA positivity,and severe target organ damage and were found to share vasculitis as the common cause.In the future,we will confirm the relationship between MHT and systemic vasculitis through follow-up outcomes.
Conclusions
Systemic vasculitis may be one of the main causes of MHT,and was underestimated in the past.Despite clinical manifestations and laboratory indicators of systemic vasculitis not being specific,the target organ damage is great.In future clinical work,clinicians need to pay more attention to these patients with systemic vasculitis and more actively treat them.
Acknowledgments
We sincerely thank all the staff of the Center of Hypertension in Xinjiang for their support with the medical examinations and demographic data collection.This study was supported by the Special Foundation of Autonomous Region Key Laboratory of China (grant number 2014KL014) and the National Natural Science Foundation of China (grant number 81360051).
Conflict of Interest
The authors declare that they have no conflicts of interest.
REFERENCES
1.Keith NM,Wagener HP,Barker NW.Some different types of essential hypertension:their course and prognosis.Am J Med Sci 1974;268(6):336- 45.
2.Guzik T,Prejbisz A,Miko B,Jczyk T,Osmenda G,Januszewicz W.Malignant hypertension:new aspects of an old clinical entity.Pol Arch Med Wewn 2016;126(1- 2):86- 93.
3.Lane DA,Lip GY,Beevers DG.Improving survival of malignant hypertension patients over 40 years.Am J Hypertens 2009;22:1199- 204.
4.Huang H,Luo Y,Liang Y,Long X,Peng Y,Liu Z,et al.CD4 + CD25 + T cells in primary malignant hypertension related kidney injury.Sci Rep 2016;6:27659.
5.Michelli A,Bernardi S,Grillo A,Panizon E,Rovina M,Bardelli M,et al.A case report of malignant hypertension in a young woman.BMC Nephrol 2016;17:65.
6.Prejbisz A,Klisiewicz A,Januszewicz A,Lenders JW,Pregowska-Chwala B,J ó zwik-Plebanek K,et al.22-year-old patient with malignant hypertension associated with primary aldosteronism.J Hum Hypertens 2013;27:138- 40.
7.Kumar UM,Pande P,Savita SS,Ashwin PK,Yelikar BR.An extraadrenal pheochromocytoma presenting as malignant hypertensiona report of two cases.J Clin Diagn Res 2013;7:1177- 9.
8.Fern á ndez-Rodr í guez E,Villar-Taibo R,Pinal-Osorio I,Cabezas-Agr í cola JM,Anido-Herranz U,Prieto A,et al.Severe hypertension and hypokalemia as first clinical manifestations in ectopic Cushing' s syndrome.Arq Bras Endocrinol Metabol 2008;52:1066- 70.
9.Ramdoo K,Salam M,Warakaulle D,Liong WC.Subintimal renal artery angioplasty in a case of renal artery stenosis leading to malignant hypertension.JRSM Short Rep 2012;3:18.
10.Moroz LA,Simpson LL,Rochelson B.Management of severe hypertension in pregnancy.Semin Perinatol 2016;40:112- 8.
11.Rodriguez-Iturbe B.Autoimmunity in the pathogenesis of hypertension.Hypertension 2016;67:477- 83.
12.Patel B,Tiwari A,Dubey SR,Bhatt GC,Tiwari P,Bhan BD.Takayasu arteritis presenting with malignant hypertension;a rare manifestation of a rare disease:a case report and review of the literature.Trop Doct 2017;47:60- 3.
13.Blaustein DA,Kumbar L,Srivastava M,Avram MM.Polyarteritis nodosa presenting as isolated malignant hypertension.Am J Hypertens 2004;17:380- 1.
14.Kettritz R,Luft FC.Severe hypertension with large-vessel arteritis.Hypertension 2012;59:179- 83.
15.Luo Q,Li NF,Yao XG,Zhang DL,Abulikemu SF,Chang GJ,et al.Potential effects of age on screening for primary aldosteronism.J Hum Hypertens 2016;30:53- 61.
16.Nieman LK,Biller BM,Findling JW,Newell-Price J,Savage MO,Stewart PM,et al.The diagnosis of Cushing' s syndrome:an Endocrine Society clinical practice guideline.J Clin Endocrinol Metab 2008;93:1526- 40.
17.Arend WP,Michel BA,Bloch DA,Hunder GG,Calabrese LH,Edworthy SM,et al.The American College of Rheumatology 1990 criteria for the classification of Takayasu arteritis.Arthritis Rheum 1990;33:1129- 34.
18.Lightfoot RW,Michel BA,Bloch DA,Hunder GG,Zvaifler NJ,McShane DJ,et al.The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa.Arthritis Rheum 1990;33:1088- 93.
19.Masi AT,Hunder GG,Lie JT,Michel BA,Bloch DA,Arend WP,et al.The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis).Arthritis Rheum 1990;33:1094- 100.
20.Leavitt RY,Fauci AS,Bloch DA.The American College of Rheumatology 1990 criteria for the classification of Wegener' s granulomatosis.Arthritis Rheum 1990;33:1101- 7.
21.Jennette JC,Falk RJ,Bacon PA,Basu N,Cid MC,Ferrario F,et al.2012 revised International Chapel Hill Consensus Conference nomenclature of vasculitides.Arthritis Rheum 2013;65:1- 11.
22.Watts R,Lane S,Hanslik T,Hauser T,Hellmich B,Koldingsnes W,et al.Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies.Ann Rheum Dis 2007;66(2):222.e7.
23.Ananthan S,Onida AH.Davies.Nutcracker syndrome:an update on current diagnostic criteria and management guidelines.Eur J Vasc Endovasc Surg 2017;53:886- 94.
24.Van den Born BJ,Honnebier UP,Koopmans RP,van Montfrans GA.Microangiopathic hemolysis and renal failure in malignant hypertension.Hypertension2005;45:246- 51.
25.Amraoui F,Bos S,Vogt L,van den Born BJ.Long-term renal outcome in patients with malignant hypertension:a retrospective cohort study.BMC Nephrol 2012;13:71.
26.Mitchell HC,Graham RM,Pettinger WA.Renal function during longterm treatment of hypertension with minoxidil:comparison of benign and malignant hypertension.Ann Intern Med 1980;93:676- 81.
27.Januszewicz A,Guzik T,Prejbisz A,Miko ł ajczyk T,Osmenda G,Januszewicz W.Malignant hypertension:new aspects of an old clinical entity.Pol Arch Med Wewn 2016;126:86- 93.
28.Mathew RO,Nayer A,Asif A.The endothelium as the common denominator in malignant hypertension and thrombotic microangiopathy.J Am Soc Hypertens 2016;10:352- 9.
29.Strizhakov LA,Moiseev S,Semenkova EN,Kuznetsova EI.Cardiovascular complications and endothelial dysfunction in primary vasculitis.Ter Arkh 2012;84:31- 5.
30.Mammeria A,Guermazb R,Hatrib A,Kessalb F,Taharboucht S,Hamrour F,et al.Hypertension during Takayasu' s disease:an Algerian single center experience of 279 patients.Ann Cardiol Angeiol 2017:66:154- 8.
杂志排行
Cardiovascular Innovations and Applications的其它文章
- Selective Coronary Angiography Following Cardiac Arrest
- Predictive Value of Resting Pd/Pa for Fractional Flow Reserve Assessed with Monorail Pressure Microcatheter in Real-World Practice
- Ultrasound:The Potential Power for Cardiovascular Disease Therapy
- The Relationship Between Mean Platelet Volume and ln-Hospital Mortality in Geriatric Patients with ST Segment Elevation Myocardial lnfarction Who Underwent Primary Percutaneous Coronary lntervention
- Giant Aneurysm of a Coronary-Pulmonary Artery Fistula:A Rare Cause of a Diastolic Murmur
- Superior Vena Cava Occlusion as a Complication of Transvenous Cardiac Device Implantation:A Case Report and Brief Review