Recurrent surgical site infection after anterior cruciate ligament reconstruction:A case report
2019-06-20DonKohShiMingTanAndrewHweeChyeTan
Don Koh,Shi Ming Tan,Andrew Hwee Chye Tan
Abstract
Key words: Chronic surgical site infection;Anterior cruciate ligament reconstruction;Surgical site infection;Graft preservation;Enterobacter cloacae complex;Septic arthritis;Case report
INTRODUCTION
Surgical site infections following arthroscopic anterior cruciate ligament (ACL)reconstruction are uncommon.Current literature suggests the incidence rate to be around 1.7%[1-3]with almost all cases presenting in the acute or subacute postoperative periods[1,2,4-6].Prompt diagnosis and treatment are necessary to avoid devastating consequences such as septic arthritis and its sequelae[7].
Various management protocols have been described in the literature with limited consensus on the best practice.Controversy remains with regards to the decision for graft-sparing versus graft-sacrificing surgery,especially for recurrent infections.Most authors,however,agree on the need for early irrigation and debridement as well as culture-directed antibiotic therapy[8].
While Gram-positive cocci are the most frequently encountered pathogens in surgical site infections,members of the Enterobacteriaceae family,namely Enterobacter cloacae complex (ECC),have also been reported[6,9].ECC is a major cause of nosocomial and opportunistic infections,but its involvement in joint and graft infections is rare[6,9].Its ability to form biofilms,produce cytotoxins and its intrinsic resistance to multiple beta-lactam antibiotics make this pathogen difficult to eradicate and treat effectively[10].To date,there is a paucity of literature describing chronic or delayed surgical site infections after ACL reconstruction.We describe the first case of a delayed,recurrent infection involving both the tibial and femoral surgical sites which occurred at four and nine years respectively following an ACL reconstruction.
CASE PRESENTATION
Chief complaints
A 33-year-old gentleman who presents with a history of recurring ACL surgical site infections.
History of present illness
This patient underwent left knee ACL reconstruction,using a hamstring tendon autograft with Endobutton fixation to the distal femur and interference screw fixation to the proximal tibia.He had an uneventful recovery and was able to return to his pre-injury activity level.Four years after his index surgery,he developed a left proximal tibial abscess over the interference screw site.He underwent incision and drainage of the tibial abscess.Intraoperatively,a remnant non-absorbable Ethibond suture was found at the base of the abscess.This remnant suture was removed and there was no infective extension into the tibia tunnel or graft.Tissue cultures grew ECC.He completed a two-week course of culture-directed oral Ciprofloxacin and was subsequently noted to be well during outpatient follow-up.
Nine years after the index surgery,this patient spontaneously developed left lateral thigh swelling (Figure 1).Magnetic resonance imaging (MRI) revealed a large rimenhancing fluid collection form the femoral tunnel extending to the subcutaneous tissue with marrow enhancement adjacent to the femoral tunnel.An incision and drainage were performed and initial wound cultures yielded no bacterial growth.This was complicated by persistent discharge and the formation of a sinus tract over the lateral thigh wound.Patient subsequently presented to our clinic seeking a second opinion.
Physical examination
Clinical examination revealed a discharging sinus over the left lateral thigh wound.He was afebrile,ambulated well,demonstrated good range of motion in the left knee and anterior drawer test was negative.There was no clinical evidence suggesting septic arthritis.
Laboratory examination
Laboratory investigations revealed elevated C-reactive protein (CRP) of 17.8 mg/L but normal erythrocyte sedimentation rate (ESR) of 1.0 mm/hr as well as total white cell count (TW) of 5.70 × 109/L.
在施工过程中,存在砂浆配合比误差较大的现象,砂浆分布不均匀就会出现强度偏低的现象,从而使得建筑物出现基础裂缝。另外,建筑物的围护结构和混凝土墙柱的铺设与规定不符,使得受力不均匀,也会导致地基基础发生不均匀沉降。
Imaging examination
Repeat MRI showed a fistulous communication between the lateral thigh wound extending toward the femoral tunnel with early features of osteomyelitis with no evidence of graft infection (Figure 2).
FINAL DIAGNOSIS
Recurrent surgical site infection after ACL reconstruction.
TREATMENT
The patient was counselled extensively for further debridement and understood the potential need for graft removal should there be evidence of intra-articular involvement.Arthroscopic exploration and washout as well as lateral thigh wound redebridement,wound exploration,excision of sinus tract and removal of Endobutton was performed.Intra-operatively,the graft was noted to be in tact with no evidence of infection within the knee (Figure 3).In addition,the sinus tract led to the Endobutton site.The tract was excised in its entirety and the Endobutton removed.Underlying bone was curetted and noted to be healthy.
OUTCOME AND FOLLOW-UP
Tissue cultures from the sinus tract grew ECC,demonstrating similar antibiotic sensitivities to the tibial abscess cultures done in 2012.Joint fluid cultures,however,did not grow any organisms.Antibiotic therapy was escalated to Ertapenem in view of the recurrent nature of the infection.He completed a six-week course of antibiotics.Six months after surgery,his wound had healed well (Figure 1) and the inflammatory markers had normalised (CRP 4.6 mg/L,ESR 2 mm/h and TW 5.51 × 109/L).He remains asymptomatic with excellent knee function and has returned to his normal activities.
DISCUSSION

Figure 1 Wound site throughout recovery.
Majority of post-ACL reconstruction surgical site infections occur acutely (< 2 wk after surgery) and sub-acutely (between 2 wk and 2 mos after surgery)[4,6,11].Pathogens commonly identified are skin commensals associated with peri-operative inoculation.Graft contamination can occur at any point during its harvest,preparation and reintroduction.Prior to a graft's re-incorporation,its lack of blood supply makes it a potential nidus for infection[4,12].Another source of infection includes the surgical incisions or arthroscopic portals.The use of long instruments is also a potential source of intra-articular inoculation[4,12,13].
Mouzopouloset al[4]postulated that late infections (> 2 mo) are often extra-articular in origin.The tibia and femoral tunnels are potential tracks for infections - bridging extra-articular infections with the intra-articular environment.The relatively superficial position of the interference screws and metallic endobutton,coupled with local tissue injury,predisposes to wound complications and infections.Juddet al[13]reported similar findings after noting eight out of eleven intra-articular infections having concomitant extra-articular wound complications - both of which having similar causative organisms on culture.McAllisteret al[14]recommended the use of non-cannulated interference screws suggesting cannulated screws are a potential conduit for extra-articular pathogens.
In patients with extra-articular infection after ACL graft reconstruction,the risk of intra-articular involvement is ever present.Communication of the extra-articular with the intra-articular space via both tibial and femoral tunnels is a constant risk factor.The presence of foreign material such as sutures promote bacterial seeding and limits the effect of antibiotic clearance.In a recurrent case of infection,we suggest the removal of hardware with a view of graft removal should its integrity be compromised or if there is evidence of intra-articular involvement.
In our patient,the first surgical site infection involved the tibial interference screw site and occurred four years after the index surgery,with a subsequent infection five years later on the femoral site,centred around the Endobutton.Reaction to the implants and suture material and seeding of bacteria around these implants may be the cause of the infection on both occasions.Some studies have demonstrated increased risk of infection with hamstring autograft use[2,5,13].Kimet al[2]hypothesised that the relative short length of the harvested hamstring autograft results in additional suture and hardware within the bone tunnels[5].The increased foreign body load -both graft and hardware,increases both infection risks and foreign body reactions[2,5,15].Even when sterile,foreign body reaction can stimulate inflammatory mediators,activating multinucleated giant cells.This produces a reaction of varying severity,ranging from oedema,sinus development to destruction to local structures[13,16].
In view of the chronic and indolent nature of the infection in our patient,incomplete eradication of the infection remained a concern.Our patient was counselled extensively pre-operatively and was agreeable for graft removal should there be a clinical indication.
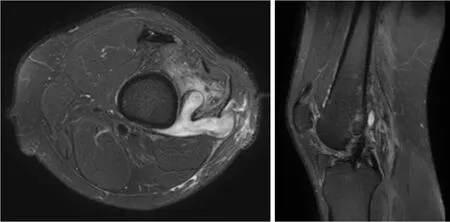
Figure 2 Magnetic resonance imaging knee showing a fistulous communication of a complex Y-shaped abscess in the lateral aspect of the distal thigh extending towards the femoral tunnel of the anterior cruciate ligament reconstruction.
The management of septic arthritis after ACL reconstruction remains controversial.Multiple management protocols have been proposed with limited consensus amongst authors.The main debate involves graft preservation versus graft removal in recurrent infections.Most authors to date opt for graft preservation treatment protocols involving long-term culture-directed antibiotics,arthroscopic irrigation and debridement as the first line of action.Should recurrent infections occur,this process is repeated until the complete eradication of infection.Proponents for graft preservation recommend such a protocol,boasting success rates of 85%[17].This pathway is most agreeable amongst most authors and patients as it avoids morbidity from graft removal and the need for a staged reconstruction.
Opponents of graft preservation argue that the graft,if left in place,will remain a source of infection[1].Kimet al[2]reported that an average of 1.9 procedures were needed for complete eradication of infection.Failure to eradicate the pathogen completely would result in repeated infections thereby requiring additional procedures.In patients with recurrent infections,risk of graft failure,loss of hyaline cartilage,damage to menisci and arthrofibrosis are complications that these group of authors strive to avoid[4,17,18].Prompt removal of the infected graft and early reconstruction have also demonstrated good outcomes.
Intra-articular involvement can be ascertained through thorough history taking;detailed clinical examination and obtaining pertinent laboratory tests (e.g.,CRP,ESR and TW).Arthroscopy can be performed to visualise the intra-articular structures and study the ACL graft.Joint fluid can also be collected for culture and to ascertain bacterial antibiotic sensitivities.In our patient,it was only after establishing that this was an extra-articular infection that the decision made intra-operatively to proceed with debridement,graft preservation and removal of implant.
Interestingly,ECC was cultured from affected tissue on both occasions.WhileStaphylococcus aureusand coagulase-negativeStaphylococcusare the commonest skin flora accounting for up to 88% of post-arthroscopic infections,there are reports involving gram-negative bacteria as well[6].However,the literature detailing gramnegative pathogens such as ECC is scarce,limiting our understanding of its true incidence and pathogenicity[10].ECC comprises of six species showing genetic relatedness toE.cloacae- namelyE.ludwigii,E.nimipressuralis,E.kobei,E.asburiae,E.cloacaeandE.hormaechei[19].ECC are commensals of the gut,but is known to cause up to 5% of hospital-acquired sepsis[5,6].The gastrointestinal tract as well as our skin are common sites whereby ECC is contracted[1,19].Other sources include medical devices as well as intravenous products.It is a pathogen of increasing interest,due to its ability to form biofilms,secrete various cytotoxins as well as its innate resistance to beta-lactams due to AmpC beta-lactamase production[10,20].These traits make it a potentially difficult pathogen to treat,especially after it has colonised an implant.This may explain the insidious onset of symptoms and chronic nature of this case.
The attributes ofE.cloacaemake complete eradication challenging,especially in setting of implant involvement.Unlike common pathogens (e.g.,Staphylococcus aureusand coagulase-negativeStaphylococcus),E.cloacaepresents as an indolent chronic infection presenting years after initial inoculation.The cause remains unclear.However,in the setting of prior infection,incomplete eradication is the most likely cause for recurrent surgical site infection.In addition,foreign body reaction played an important role in the initial swelling and effusion over the interference screw and Endobutton sites.Non-involvement of the graft,noted during arthroscopy,suggests that the graft did not serve as a conduit for infection.The authors have demonstrated that favourable outcomes can be achieved with graft preservation when the graft is not compromised,even with chronic recurrent surgical site infections.

Figure 3 Arthroscopic images of the left knee joint.
CONCLUSION
This report illustrates an unusual case of recurrent infections involving both the tibial and femoral surgical sites years after an ACL reconstruction.It emphasizes the importance of prompt and accurate diagnosis - especially the exclusion of intraarticular infection.The authors have demonstrated that in cases without graft involvement,debridement with graft preservation,removal of implants and a course of antibiotics may be a suitable treatment option.