Delirium after emergency hip surgery - common and serious,but rarely consented for
2019-06-20LouisKoiziaFayeWilsonPeterReillyMichaelFertleman
Louis J Koizia,Faye Wilson,Peter Reilly,Michael B Fertleman
Abstract
Key words: Delirium;Proximal femoral fractures;Consent;Hip surgery;Montgomery;Medicolegal
INTRODUCTION
The care and management of patients with femoral neck fractures have been the focus of growing interest over the past twenty years[1].Early intensive geriatric input following hip fractures has been shown to reduce mortality and medical complications[2].Similarly,multidisciplinary,collaborative models of care have been shown to decrease the incidence of postoperative complications and readmission rates[3].Multidisciplinary care involving orthopaedic surgeons,geriatricians,therapists and discharge co-ordinators,allow regular discussion of patients and planning for discharge.Agreed standards of care now exist jointly written by geriatricians,orthopaedic surgeons and anaesthetists,a nationwide data collection system keeping track of management and outcomes (the National Hip Fracture Database) and a payment system that rewards trusts adhering to best practice care[4].There is an evidence base to guide practice and also scores that may predict poor outcomes[1,5].
One predictor of poor outcome is post-operative delirium,which can affect a large proportion of patients post operatively,yet is rarely mentioned to patients or families when the treatment and recovery from a proximal femoral fracture is discussed[6].Delirium is defined as a “clinical syndrome characterised by disturbed consciousness,cognitive function or perception,which has an acute onset and fluctuating course”[7].
INCIDENCE AMONGST OLDER ADULTS
Many studies have looked at delirium rates amongst older adult inpatients,and estimates of prevalence vary from 29% to 64% amongst medical wards,with patients being admitted for a number of reasons and not primarily delirium[8-10].The variance is thought to be due to heterogeneous or poorly defined diagnostic criteria used in different clinical trials,often leading to under diagnosis.Surgical patients are no different,with studies of post-operative cardiac bypass patients detecting it in up to 52% of subjects[11].A meta-analysis looking at incidence of delirium post hip fracture in elderly patients found an accumulated incidence of 24%[12].
There are many triggers for developing delirium,including infection,myocardial and cerebral ischaemia,electrolyte abnormalities,commencement of new medications,withdrawal from alcohol or drugs (such as benzodiazepines),pain,constipation and urinary retention[13].Certain patient characteristics also predispose to developing delirium;these include advanced age,pre-existing cognitive impairment,sensory impairment (from visual and hearing loss),poly-pharmacy,and medical comorbidities[14].Specifically related to hip fractures,the mechanism of injury,the fracture,the operation and anaesthetic can all increase the risk of developing delirium[12,15,16].
DIAGNOSING DELIRIUM - CRITERIA AND PATHOPHYSIOLOGY
In clinical trials the incidence of diagnosed delirium varies widely,even when the diagnosis is being actively sought as an outcome measure,implying that in the everyday ward-based setting diagnosis may be even more elusive[17].Most healthcare professionals would recognise that the agitated,aggressive patient keeping the ward awake at night is unwell,but how many accurately diagnose hyperactive delirium?The sleepy patient,“just not herself”,refusing therapy and staying in bed may have hypoactive delirium,but this is less likely to be diagnosed and treated appropriately[18].
The Confusion Assessment Method (CAM) is a quick,accurate and frequently used tool to recognise and diagnose delirium[19].It can be incorporated into routine assessment of patients and has been shown to have high sensitivity,specificity and interrater reliability[20].The CAM algorithm is based on:(1) Acute onset and fluctuating course;(2) Inattention;(3) Disorganised thinking;and (4) Altered consciousness[21].A diagnosis of delirium requires the presence of features 1,2 and either 3 or 4 (Table 1).
Hyperactive and hypoactive subtypes are broadly defined according to psychomotor activity,with clinical features varying accordingly,but mixed delirium,with features of both,also exist[22].The pathophysiology of delirium is not fully understood,and of the many theories none explain the variation in presentation and severity.Current theories centre on deranged neurotransmission and signalling pathways,as well as neuroinflammation and glial activation,which appear to be pivotal in the post-operative period[22].
CONSEQUENCES OF DELIRIUM ARE AS SERIOUS AS INFECTION OR THROMBOEMBOLIC EVENTS
Does confusion matter in the context of breaking a hip and having a major operation,and is it important enough to mention during the consent process? Are the consequences of deep wound infection,thromboembolic events and bleeding more severe,necessitating their inclusion on consent forms over delirium?
Whilst it is true that a large pulmonary embolus (PE) can be fatal,and revision surgery to replace an infected implant can be catastrophic for functional recovery and is associate with poorer outcomes,there is evidence that delirium also has a major and long-lasting effect[23].Suffering from an episode of delirium has an impact on length of stay,post discharge institutionalisation and mortality[24].Patients require greater input from nursing staff on the ward,both to provide personal care and to ensure safety.They are less able to work with physiotherapists leading to longer periods of therapy being required and cost of admission[25].A substantial proportion of those who eventually return home will require extra assistance,both formally from social services and also informally from family and friends[26].Delirium is an independent marker for increased 12 month mortality following a hospital admission,with the effect more marked for patients without pre-existing dementia[27].
As well as a change in dependency and social circumstances,quality of life can be directly affected by the psychological impact of delirium itself,both during the actual episode and also in the longer term[28].A study looking at cancer patients suffering delirium identified that patients recalled their episodes of delirium,and expressed distress as a result[29].Patients commonly describe concerns with day-night orientation,communication difficulties and delusional thoughts[30].The longer lasting psychological impact of delirium,is not only experienced by patients but members of staff and patient relatives;caregiver distress as a result of delirium has been identified as being even higher than patient distress[28].
MANAGEMENT STRATEGIES FOR DELIRIUM
Once delirium has developed there is limited evidence that medications such as benzodiazepines or neuroleptics are beneficial and they are associated with severe side effects,particularly in the elderly population[31].The main stay of pharmacological measures is to treat causative factors,such as using antibiotics to treat an underlying infection[22].Proactive geriatric consultation can reduce episodes of delirium by 40% in patients with proximal femoral fractures[6].The Hospital Elder Life Program reduced the number and duration of episodes by using delirium prevention strategies (such as maintaining orientation,reducing sensory deficits,ensuring adequate nutrition and hydration) to improve the overall hospital experience[32].
The best management strategy for delirium is prevention in the first place.Early orthogeriatric input as part of a multidisciplinary team has been found to prevent delirium[33].The comprehensive geriatric assessment focuses on eliminated unnecessary medication,early identification and treatment of complications and mobilisation.
Specifically,in patients with femoral neck fractures,adequate pain management and analgesics have effect on delirium.Yanget al[12]identified patients receiving morphine were three times more at risk of developing delirium after hip fracture surgery than nonusers.Despite it being important to rationalise and ensure safe prescribing in our population group to prevent delirium,undertreated pain and inadequate analgesia appear to be risk factors for developing delirium in frail older adults[34,35].The analgesic,pain and delirium association remains inconsistent.Therefore,a fine balance with regular review of patients is imperative.
Prophylactic pharmacological therapies have been trialled,but showed no efficacy in reducing the incidence of delirium[36].One important element for the prevention of delirium,is education of the medical staff.An education program can lead to an increase in detection of delirium as more cases are recognised,yet a decrease in point prevalence (19.5% to 9.8%) due to a more proactive approach[37].Multidisciplinary teaching programs are also essential,as other members of the team who spend a proportionally large amount of time with patients,play an important role in implementing management and prevention strategies.
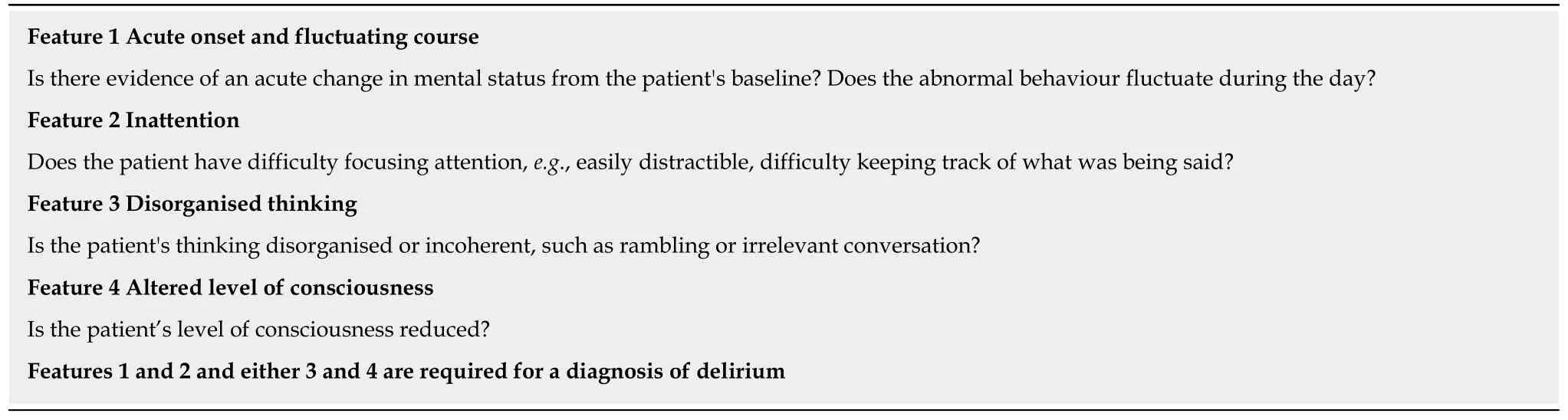
Table 1 Confusion assessment method - adapted from lnouye et al[20]
CONSENT PROCESS
Patient autonomy is one of the four pillars of modern medical ethics and stemming from this is the right of the patient to determine whether they wish to undergo any medical intervention.In order to give consent for surgery,patients must be presented with sufficient information about the proposed procedure and the treatment options,to be able to determine the pros and cons of either giving or refusing their permission[38].The Courts have long-held that the potential complications which should be mentioned are both the common and the rare but serious[39].In hip fracture the emphasis is slightly different,as the surgery is fundamentally essential,and outcomes worsen as surgery is delayed[40].However,the premise that both common and serious complications should be mentioned still holds true.
Traditionally patients giving their consent sign a consent form as part of this process,but the varying standards of the quality of information provided to the patient are well documented[41].A review of 100 consent forms of patients undergoing surgery for hip fracture,looked at the quality of documentation of patient and procedure details,as well as which potential complications were mentioned[42].The number of complications mentioned ranged from four to eleven,with infection,thromboembolic complications,and bleeding most commonly included.In total 30 different complications were stated,with not a single mention of post-operative confusion or delirium.Rates of PE and deep wound infection are far lower than delirium,at under 7% and 3.6% respectively,but these complications are almost always mentioned[43-45].
Since 2008,the British Orthopaedic Association has endorsed the use of standardised,pre-printed consent forms for common operations,in order to improve the information given to patients prior to consent[46].This was initially designed to reduce litigation and induce a standard amongst surgeons[46].However,the consent form for fixation of a fractured hip does not mention delirium as a complication.
The 2015 supreme court case of Montgomery changed the way surgeons should approach consent.This was an obstetric case where a woman with diabetes had a complicated vaginal delivery that resulted in complications of shoulder dystocia and cerebral palsy.The mother sued for negligence stating that if she had known of the increased risk,in her case she would have requested a caesarean section.The supreme court held that doctors are required to take “care to ensure that the patient is aware of any material risks involved in any recommended treatment,and of any reasonable alternatives or varied treatments”[47].The ruling established a duty to warn of material risks,with a material risk being defined as something that a patient would consider relevant.Effectively,Montgomery changed consent in the United Kingdom from what the reasonable doctor would tell a patient,to what a reasonable patient would want to know.All interventions must be based on individualized discussions and be patient centred,allowing shared decision-making.
PARADOX - COULD SURGERY BE A PREVENTER TO DEVELOPING DELIRIUM?
Today,the vast majority of patients are managed following a hip fracture with an operation;this stems from the greater mortality in those patients not operated[48].In addition,the operation provides fixation of the underlying fracture and reduces pain overall.Therefore,a hip operation following a hip fracture reduces mortality,pain,length of stay and increases mobility[49-51].The operation aids recovery and therefore possibly reduces the risk of delirium from increased analgesic use,medical complications and prolonged hospitalisation.So therefore,should we be consenting for delirium preoperatively if it could be seen to reduce delirium occurring? The simple answer remains yes.The perioperative period brings its own risks for developing delirium,anaesthetic,theatre environment,stress and thus patients should be informed.In addition,a similar conundrum could be considered for VTE.As previously mentioned,VTE is nearly always discussed during the consent process.However,the risk of VTE following a hip fracture without an operation remains present due to prolonged immobility.
RECOMMENDATIONS
As highlighted,delirium is a common complication with consequences for the patient.The General Medical Council view on consent is that all possible adverse outcomes should be discussed with patients.It is for this reason that all patients should be consented for delirium in advance of surgery to repair a proximal femoral fracture.
As Montgomery emphasised the duty to inform a patient of a particular risk lies with the operating surgeon.Given the surgery is being performed by the orthopaedic team,it is their duty to inform and consent patients for possible delirium.That beings said,it is the job of the multidisciplinary team including physicians,anaesthetists,therapists and nurses to reduce risks of developing delirium and manage as best as possible.
CONCLUSION
In summary,delirium is a common complication of emergency hip surgery,with serious and long-lasting effects that have a significant and deleterious impact on patients' lives.It occurs as frequently as DVT,infection,haemorrhage and PE combined,currently the most commonly mentioned potential complications of emergency hip surgery.However,at present delirium is rarely,if ever,mentioned by surgeons to patients or their families during the consent process,despite being a good predictor of poor outcome and being very distressing to the patient,their relatives,and carers.
The United Kingdom Supreme Court and General Medical Council state that patients should be properly informed about risks of operations prior to surgery.A failure to mention delirium exposes the operating surgeon to risks of allegations of negligence and could be interpreted as unethical behaviour.
A further benefit of delirium being mentioned routinely by senior surgeons during the consent process would be to increase awareness of delirium and its consequences amongst junior doctors and allied health care professionals.In many centres they provide the routine day-to-day care of frail elderly patients following surgery for a proximal femoral fracture,yet receive little training on how to recognise or manage delirious patients.Whilst geriatric consultation is beneficial and improves outcomes,this service is not available out of hours in the majority of hospitals,and the initial investigations and management are often simple measures such as treating infection,anaemia,alcohol withdrawal,dehydration,pain and constipation.