Proton pump inhibitor use increases hepatic encephalopathy risk: A systematic review and meta-analysis
2019-06-13YunJieMaZongXunCaoYongLiShunYiFeng
Yun-Jie Ma, Zong-Xun Cao, Yong Li, Shun-Yi Feng
AbstractBACKGROUND Several studies have been conducted to explore the association between the use of proton pump inhibitors (PPIs) and hepatic encephalopathy (HE) risk in patients with liver cirrhosis. However, their results are controversial.AIM To perform a systematic review and meta-analysis to evaluate the HE risk among PPI users.METHODS A systematic search on PubMed, Web of Science, EMBase, and ScienceDirect databases was conducted up to December 31, 2018 for eligible studies involving PPI use and HE risk. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated using the fixed or random effects model. Publication bias was evaluated using Begg's test, Egger's test, and trim-and-fill method.RESULTS Seven studies with 4574 patients were included in the present meta-analysis. The meta-analysis results indicated a significant association between the PPI use and HE risk (OR = 1.50; 95%CI: 1.25-1.75) with low heterogeneity (I2 = 14.2%, P =0.321). Although publication bias existed when Egger's tests were used (P =0.005), the trim-and-fill method verified the stability of the pooled result.Sensitivity analyses suggested that the results of this meta-analysis were robust.CONCLUSION The current evidence indicates that PPI use increases HE risk in patients with liver cirrhosis. Further studies with a large data set and well-designed models are needed to validate our findings.
Key words: Proton pump inhibitors; Hepatic encephalopathy; Meta-analysis
INTRODUCTION
Proton pump inhibitors (PPIs) are the first choice of treatment for esophagitis and peptic ulcer disease, as well as the prevention of nonsteroidal anti-inflammatory drug associated ulcers, Zollinger-Ellison syndrome, and functional dyspepsia[1]. In acidrelated diseases, the benefits of PPI use outweigh their potential harm. Unfortunately,the negative effects of PPI use are generally underestimated due to marketing strategy and neglected reporting bias in published trials. Thus, not all PPIs are used following evidence-based guidelines in the clinical setting, and PPIs are overprescribed in both inpatient and outpatient settings[2-4].
Accumulating data illustrate the potential risks associated with long-term PPI therapy, including pneumonia, spontaneous bacterial peritonitis, gastric cancer,vitamin B12 deficiency, Clostridium difficile-associated diarrhea, myocardial infarction,hypomagnesemia, chronic kidney disease, and hip fracture[5-10]. Regarding concerns over liver adverse effects, a previous meta-analysis showed that PPIs increase the risk of hepatic encephalopathy (HE) in patients with hepatic failure[11]. However, the results are restricted because of the inclusion of a relatively small number of studies.New primary studies[12-15]have also been recently published, and their results are controversial.
Therefore, in this meta-analysis, we aimed to update, compile, and critically review the existing evidence on the HE risk in patients with liver cirrhosis and PPI use and provide a quantitative estimate of the relationship between PPI use and HE risk.
MATERIALS AND METHODS
This systematic review was performed in accordance with the standards of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses[16]. Ethical approval was not sought for this study because all the data came from published studies, and no individual-level data were used. The systematic review registration number is CRD42019120845.
Literature search
A systematic search on PubMed, Web of Science, Embase, and ScienceDirect databases was conducted up to December 31, 2018 for eligible studies involving PPI use and HE risk. The following keywords were used to search for the related literature: “proton pump inhibitors” and “hepatic encephalopathy.” The reference lists of the identified articles were also manually searched to identify additional relevant studies.
Study selection
Two reviewers independently screened the titles and abstracts of the retrieved studies. Studies were considered eligible if they met the inclusion criteria, as follows:Studies assessed the association between PPI and HE risk, those with full text access,and those which included sufficient data to calculate odds ratios (ORs) and 95%confidential intervals (CI) for extraction. Among duplicate studies, the most recent study was included in this meta-analysis. The exclusion criteria were as follows:Insufficient data for extraction, articles that are available only in abstracts, case reports, conference papers, editor comments, reviews, meta-analysis, and inclusion of duplicate data in other studies.
Data extraction
Data were extracted independently by two reviewers using the data extraction tables.The results were compared, and disagreements were discussed. The following data were extracted: First author's name, publication year, region, number of patients, age,sex, PPI use duration, HE level, and outcomes.
That was not a loving speech, said Sophy, nor spoken like aChristian. In a future state, where there is neither marrying norgiving in marriage, but where, as you say, souls are attracted to eachother by sympathy; there everything beautiful develops itself, andis raised to a higher state of existence: her soul will acquire suchcompleteness that it may harmonize with yours, even more than mine,and you will then once more utter your first rapturous exclamationof your love, Beautiful, most beautiful!
Bias risk
To evaluate the methodological quality of the included studies, we used the Newcastle-Ottawa scale (NOS)[17]. The range of NOS scores was from 0 to 9, and a score ≥ 6 was defined as “high quality”[18,19].
Statistical analysis
Statistical analyses were performed using STATA version 12.0 (Stata Corporation,College Station, TX, United States), and two-sided P < 0.05 was considered statistically significant. Pooled ORs with 95%CIs were utilized to evaluate the relationship between PPI use and HE risk. Statistical heterogeneity was assessed based on P- and I2-values by using the standard Chi-squared test. Low, moderate, or high heterogeneity among studies was defined as I2< 25%, 50%-75%, and > 75%, respectively.When I2> 50%, P < 0.1 was considered significantly heterogeneous, and the random effects model was used for meta-analysis; otherwise, the fixed effects model was used.We performed a sensitivity analysis by excluding one study at a time to assess the effect of individual studies on the summary estimates. Publication bias was evaluated using Begg's test, Egger's test, and trim-and-fill method.
RESULTS
Study selection
The details of study identification, screening, and selection are presented in Figure 1.The initial database search yielded 888 records, of which 107 duplicates were excluded. Then, 771 records, including 768 irrelevant studies and 3 reviews, were removed through the primary screening of titles and abstracts. After assessing ten full-text studies, two conference abstractions and one editor comment were excluded.Finally, seven articles[12-15,20-22]involving 4574 patients were included in this metaanalysis.
Study characteristics
The characteristics of the included studies are summarized in Table 1. The seven included studies[12-15,20-22]were published within the last 5 years, altogether involving 4574 patients. Among the seven articles[12-15,20-22], three were based on Asian populations[15,21,22], and four involved Europeans[12-14,20]. Out of the seven included studies[12-15,20-22], six were retrospective[13-15,20-22], and one was prospective[12]. The NOS scores of the eligible studies[12-15,20-22]ranged from 7 to 9, with a mean of 7.9, thereby indicating that the included studies were of high quality (Table 2).
Figure 2 shows the pooled results from the fix-effects model combining ORs for HE risk. Our meta-analysis result indicated a significant association between PPI use and HE risk (OR = 1.50; 95%CI: 1.25-1.75; Figure 2) with low heterogeneity (I2= 14.2%, P =0.321).
Sensitivity analysis and publication bias
Sensitivity analyses showed that pooled OR for PPI use and HE risk association and the corresponding 95%CIs were unaltered substantially by removing one study,thereby suggesting that the results of this meta-analysis were robust (Figure 3).Although publication bias existed as indicated by the results of the Egger's tests(Egger's tests, P = 0.005; Begg's tests, P = 0.133), the trim-and-fill method verified the stability of the pooled result, and the pooled OR was unaffected (1.58, 95%CI: 1.36-1.85; Figure 4).
DISCUSSION
In this study, we performed a meta-analysis to observe HE alterations in patients with liver cirrhosis and explore the relationship between PPI use and HE risk. The findings from this study indicated an increase of 50% risk of HE among PPI users, which was consistent with the results obtained in a previous study[11]. Our meta-analysis expanded the results of previous studies and increased the statistical power to evaluate the effects.
The mechanisms of PPIs on the occurrence of HE in cirrhosis are unclear. However,as proposed, PPI use can contribute to the gut dysbiosis that generally exists in patients with cirrhosis, whereas altered gut microbiota can induce or exacerbate HE occurrence[23,24]. Intestinal bacteria in the colon produce ammonia from glutamine and nitrogenous source catabolism. An increased ammonia level in the brain results in HE occurrence by primarily influencing the brain energy metabolism and central nervous system[25,26]. PPI use also inhibits neutrophil-endothelial cell interactions and reduces natural killer cell activities and neutrophils[27], thereby possibly promoting HE occurrence due to the failure of local and systemic immune defense[28].
Low heterogeneity was detected among the included studies and meta-regression analysis was not required. However, we were also concerned about the effect of publication bias because positive results are likely to be published. Although publication bias existed when Egger's tests were used, the trim-and-fill method verified the stability of the pooled result.
Considering that PPI use is associated with an increased risk of HE occurrence in patients with liver cirrhosis, physicians should ban PPI use in these patients and those with portal hypertension when PPIs are used without specific indications[29]. Adhering to evidence-based guidelines is the only way to ensure effective and safe PPI use[30].Regulatory authorities should also assume supervision and management responsibilities to avoid inappropriate PPI use[31].
This study has several potential limitations. First, given the heterogeneity of the studies included, some of the results should be regarded with caution. Second, we included only trials published in English. Third, the number of included studies was relatively small. Although we conducted a comprehensive literature search, only seven studies were included.
In conclusion, the results of our meta-analysis suggests that PPI use is independently associated with HE risk. Therefore, randomized multicentric studies with a large sample size should be conducted to provide further insight into the potential impact of PPIs on HE.
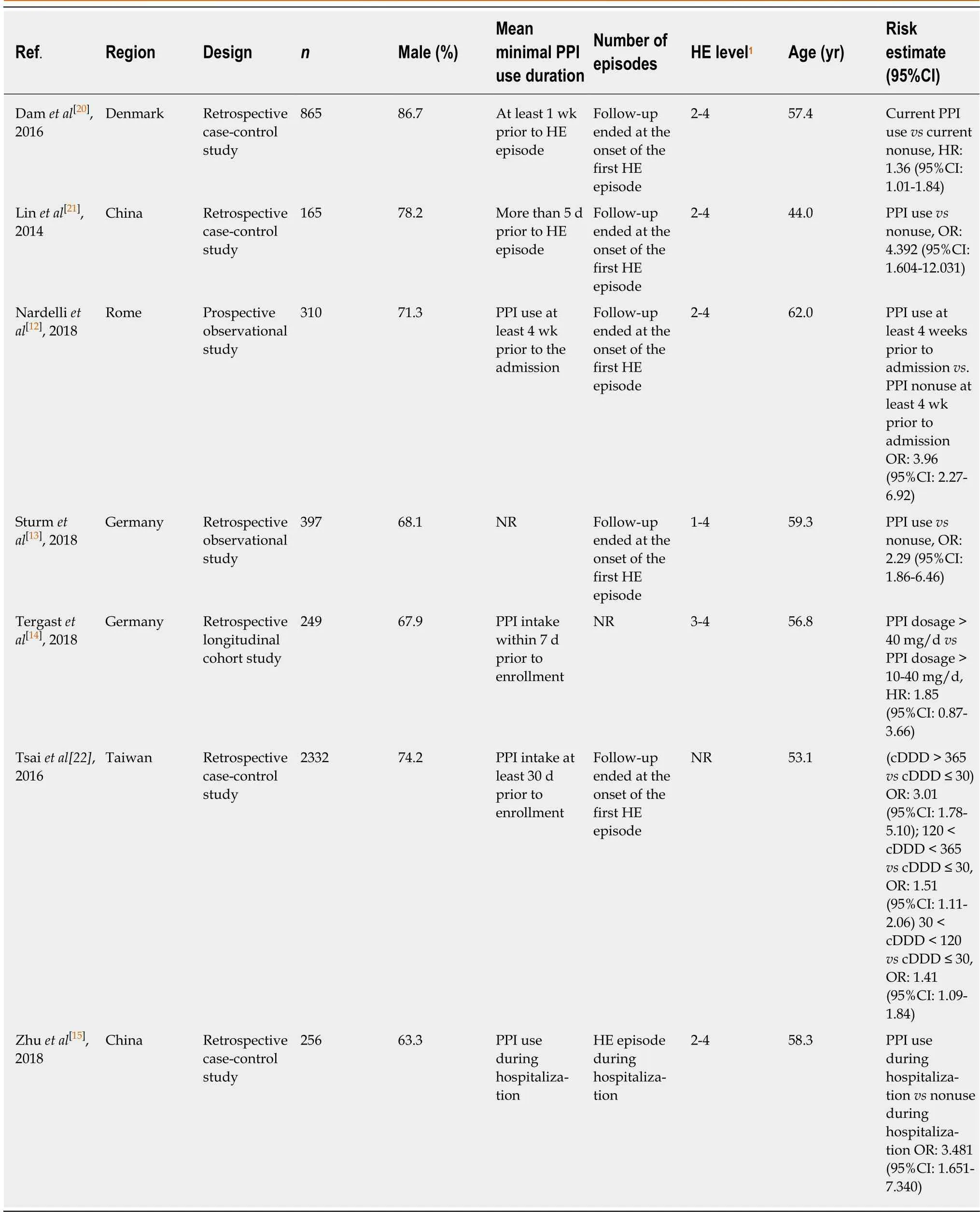
Table 1 Characteristics of included studies
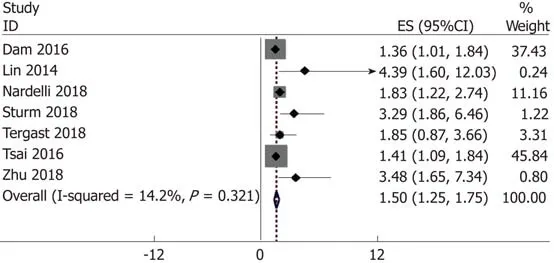
Figure 2 Forest plot of proton pump inhibitor use and hepatic encephalopathy risk. CI: Confidence interval.
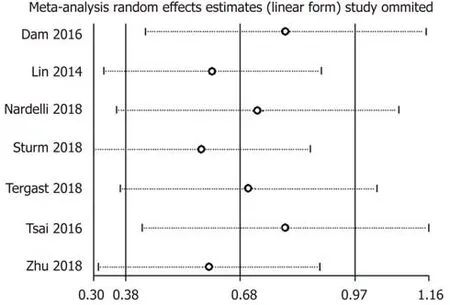
Figure 3 Funnel plot of sensitivity analysis.
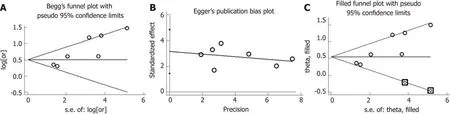
Figure 4 Publication bias funnel plot. A: Begg's test; B: Egger's test; C: Trim-and-fill method.
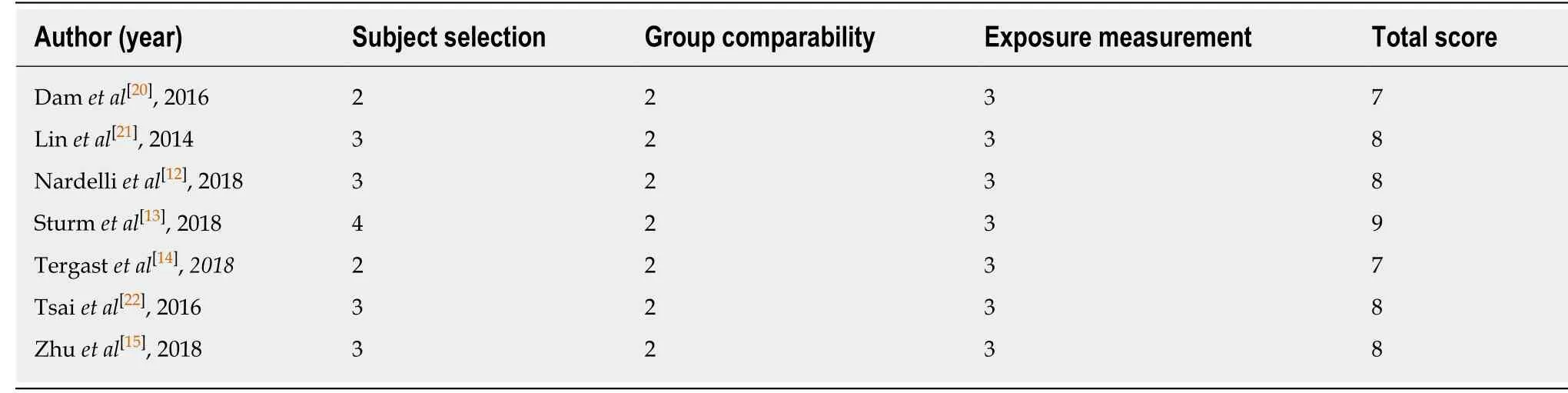
Table 2 Quality assessment of included studies using the Newcastle-Ottawa scale
ARTICLE HIGHLIGHTS
Research background
Proton pump inhibitors (PPIs) are the first choice of treatment for esophagitis and peptic ulcer disease, as well as the prevention of nonsteroidal anti-inflammatory drug associated ulcers,Zollinger-Ellison syndrome, and functional dyspepsia. In acid-related diseases, the benefits of PPI use outweigh their potential harm. Unfortunately, the negative effects of PPI use are generally underestimated due to marketing strategy and neglected reporting bias in published trials. Thus, not all PPIs are used following evidence-based guidelines in the clinical setting, and PPIs are overprescribed in both inpatient and outpatient settings.
Research motivation
Regarding concerns over liver adverse effects, a previous meta-analysis showed that PPIs increase the risk of hepatic encephalopathy (HE) in patients with hepatic failure. However, the results are restricted because of the inclusion of a relatively small number of studies. New primary studies have also been recently published, and their results are controversial.
Research objectives
In this meta-analysis, we aimed to update, compile, and critically review the existing evidence on the risk of HE in patients with liver cirrhosis and PPI use and provide a quantitative estimate of the relationship between PPI use and HE risk.
Research methods
A systematic search on PubMed, Web of Science, EMBase, and ScienceDirect databases was conducted up to December 31, 2018 for eligible studies involving PPI use and HE risk. The odd ratios (ORs) and 95% confidence intervals (CIs) were calculated using the fixed- or randomeffects model. Publication bias was evaluated using the Begg's, Egger's tests, and trim-and-fill method.
Research results
The findings from this study indicated an increase of 50% risk of HE among PPI users, which is consistent with the results obtained in a previous study.
Research conclusions
Our meta-analysis expanded the results of previous studies and increased the statistical power to evaluate the effects.
Research perspectives
Randomized multicentric studies with a large sample size should be conducted to provide further insight into the potential impact of PPIs on HE.
杂志排行
World Journal of Gastroenterology的其它文章
- Predicting (side) effects for patients with inflammatory bowel disease: The promise of pharmacogenetics
- Diagnostic and therapeutic challenges of gastrointestinal angiodysplasias: A critical review and view points
- Colorectal cancer screening from 45 years of age: Thesis, antithesis and synthesis
- Gastric per-oral endoscopic myotomy: Current status and future directions
- Liver transplantation for hepatocellular carcinoma: Where do we stand?
- Systems pharmacology approach reveals protective mechanisms of Jian-Pi Qing-Chang decoction on ulcerative colitis
