Effect of prophylactic clip placement following endoscopic mucosal resection of large colorectal lesions on delayed polypectomy bleeding: A meta-analysis
2019-06-04FaresAyoubDonevanWesterveldJustinFordeChristopherForsmarkPeterDraganovDennisYang
Fares Ayoub, Donevan R Westerveld, Justin J Forde, Christopher E Forsmark, Peter V Draganov, Dennis Yang
Abstrac t BACKGROUND The role of prophylactic clipping for the prevention of delayed polypectomy bleeding (DPB) remains unclear and conclusions from prior meta-analyses are limited due to the inclusion of variety of resection techniques and polyp sizes.AIM To conduct a meta-analysis on the effect of clipping on DPB following endoscopic mucosal resection (ΕMR) of colorectal lesions ≥ 20 mm.METHODS We performed a search of PubMed and the Cochrane library for studies comparing the effect of clipping vs no clipping on DPB following endoscopic resection. The Cochran Q test and I2 were used to test for heterogeneity. Pooling was conducted using a random-effects model.RESULTS Thirteen studies with a total of 7794 polyps were identified, of which data was available on 1701 cases of ΕMR of lesions ≥ 20 mm. Prophylactic clipping was associated with a lower rate of DPB (1.4%) when compared to no clipping (5.2%)(pooled OR: 0.24, 95%CI: 0.12-0.50, P < 0.001) following ΕMR of lesions ≥ 20 mm.There was no significant heterogeneity among the studies (I2 = 0%, P = 0.67).CONLUSION Prophylactic clipping may reduce DPB following ΕMR of large colorectal lesions.Future trials are needed to further identify risk factors and stratify high risk cases in order to implement a cost-effective preventive strategy.
Key words: Meta-analysis; Clipping; Endoscopic resection; Endoscopic mucosal resection Commons Attribution Non Commercial (CC BY-NC 4.0)license, w hich permits others to distribute, remix, adapt, build upon this w ork non-commercially,and license their derivative w orks on different terms, provided the original w ork is properly cited and the use is non-commercial. See:http://creativecommons.org/licen ses/by-nc/4.0/
INTRODUCTION
Colonoscopy has been show n to decrease the risk of death from colorectal cancer through the early id entification and removal of p re-malignant or early stage cancerous lesions[1]. Εndoscopic resection (ΕR) is the preferred first-line treatment for most of these superficial neoplasms and is associated with lower costs, morbidity, and mortality w hen compared to surgery[2,3]. Most colonic polyps are less than 10 mm and can be safely and effectively resected w ith conventional snare p olyp ectomy.Conversely, larger lateral spreading lesions (LSLs) or sessile polyps, particularly those≥ 20 mm in size, are usually removed by endoscop ic mucosal resection (ΕMR) or endoscopic submucosal dissection (ΕSD). While ΕSD continues to gain traction as an alternative for lesions w ith suspected superficial invasion or subtypes of non-granular LSLs[4,5], its d efinitive role in Western clinical practice is yet to be d efined. Hence,w ide-field ΕMR remains the p referred therap y for large non-cancerous colorectal lesions.
Bleed ing is the most common ad verse event follow ing ΕR of colorectal lesions.Bleeding can be immediate (during the procedure) or delayed (post-operatively), and has been estimated to occur in 1%-6% of cases[6,7]. In the absence of coagulopathy, the risk of delayed polypectomy bleed ing (DPB) is nearly negligible for the resection of small polyps < 10 mm. Conversely, the incidence of DPB increases with polyp size[8-10].Several studies have evaluated the effect of prophylactic clipping on DPB follow ing ΕR, w ith mixed results[11-13]. The inclusion of small polyps and different ΕR techniques(i.e., conventional polypectomy, ΕMR, ΕSD) significantly limits the interpretability of the data. The primary aim of this study was to conduct a meta-analysis on the effect of p rop hylactic clip p ing on DPB follow ing ΕMR of colorectal lesions ≥ 20 mm. A second ary aim w as to evaluate the effect of clipp ing on the incid ence of ad verse events follow ing colorectal ΕR.
MATERIALS AND METHODS
Search strategy and study selection
We id entified stud ies through a literature search of tw o d atabases (MΕDLINΕ through PubMed and the Cochrane Library) w ith the last search p erformed in January 2018. The PubMed search strategy was constructed by using the follow ing string of search terms: (“clip” OR “clipp ing”) AND (“colon” OR “colorectal” OR“colonic”) AND (“end oscopic”). The search of the Cochrane library w as conducted using similar search terms. A review of the reference list of includ ed stud ies w as p erformed to id entify any relevant articles missed through the original search strategy. Titles and abstracts were screened by two investigators (F.A. and D.R.W) for relevance to the study. The full text of potentially eligible studies w as subsequently reviewed by the two investigators (F.A and D.R.W). Disagreements were resolved by consensus or by consulting with a third investigator (D.Y).
Inclusion and exclusion criteria
Studies eligible for inclusion w ere: (1) Prospective or retrospective, case-control, or cohort studies and clinical trials; (2) stud ies reporting incidence of DPB follow ing ΕR;and (3) those that included outcomes on both patients w ith prophylactic clipping vs non-clipping after resection. Εxclusion criteria were: (1) Case reports; (2) single arm retrospective or prospective case series; (3) studies not reporting incidence of DPB; (4)reviews, commentaries, surveys; and (5) duplicate studies.
Data extraction
Data from each eligible study were extracted using a standardized data extraction sheet. The extracted data included: (1) Study authors; (2) year of publication; (3)setting (location); (4) study period; (5) patient demographics (age, gender); (6) number of patients/lesions; (7) lesion characteristics (size, location, morphology); (8) type of ΕR (conventional polypectomy, ΕMR, ΕSD); (9) incidence of adverse events, including DPB and perforation; and (10) follow-up period.
Outcomes and definitions
The aim of this stud y w as to conduct a meta-analysis stud ying the effect of prophylactic clipping on DPB follow ing ΕMR of colorectal lesions ≥ 20 mm. A secondary aim was to evaluate the effect of prophylactic clipping on the incidence of ad verse events follow ing colorectal ΕR. Prophylactic clip ping w as d efined as endoscopic clipping performed with the aim of reducing the risk of delayed (postoperative) adverse events. DPB was defined as bleeding occurring post-operatively(up on conclusion of the ΕR and after scop e w ithd raw al from the p atient).Conventional polypectomy w as defined as removal of a colorectal lesion w ith a forceps or snare without prior submucosal injection. In contrast, ΕMR was defined as resection achieved by first lifting the target lesion w ith a submucosal injection follow ed by snare polypectomy. ΕSD w as d efined as any resection in w hich submucosal dissection was performed.
Assessment of methodologic quality
For prospective trials, the quality of each study was assessed using the risk-of-bias tool as outlined in the Cochrane Handbook for Systematic Reviews of Interventions(version 5.1.0). The methodologic quality of retrospective studies was assessed using the New castle-Ottaw a scale[14]. The quality of all stud ies w as assessed by 3 investigators (F.A, D.R.W, J.J.F). Funnel plots were generated to evaluate for any potential publication bias. Visual inspection of the funnel plot w as used detect significant publication bias when less than 10 studies were available for meta-analysis as recommended by the Cochrane Handbook. Εgger's regression test was used when more than 10 studies were included in the meta-analysis.
Statistical analysis
We obtained or calculated the proportions and 95%CI for each categorical variable and the mean or med ian for continuous d ata when possible. The pooled means and OR w ere calculated utilizing a random effects model. The random effects model was used regard less of underlying statistical testing of heterogeneity since it provides more conservative estimations of the pooled effects that are more likely to contain the true effect. The Cochran Q test and I2w ere used to assess heterogeneity of includ ed studies. I2values of < 25%, 25%-50% and > 50% w ere consid ered to represent low,mod erate and high heterogeneity, resp ectively. P values < 0.05 w ere consid ered significant and all tests w ere two tailed. The study w as performed in accordance w ith the PRISMA recommendations for reporting systematic review s and meta-analyses.Analysis w as cond ucted using Stata, version 15 (Stata Corp, College Station, TX,United States) and Rev Man 5.3 (The Cochrane Collaboration, Copenhagen).
RESULTS
Search results
Figure 1 depicts the study selection flow diagram. Overall, 255 studies were identified using our search strategy, of w hich 110 w ere duplicates. Of the remaining 145 studies,120 w ere exclud ed after screening titles and abstracts. Full text review w as then performed on 25 studies using the predefined inclusion and exclusion criteria, after w hich 13 studies w ere retained. Of the 13 studies, 7 w ere randomized control trials(RCTs)[13,15-21]and 6 were cohort studies (2 prospective, 4 retrospective)[11,12,22-25]. Studies w ere published betw een 2003 and 2017. Nine stud ies w ere conducted in Asia, 2 in Εurope, and 2 in the United States. These 13 stud ies w ere includ ed in the metaanalysis evaluating the impact of prophylactic clipping on adverse events follow ing colorectal ΕR. Of these, 4 studies w ith available data on specific parameters (lesion size, typ e of ΕR, clipp ing vs no clipp ing, incid ence of DPB) w ere includ ed in the analysis on the effects of prophylactic clipping on DPB after ΕMR of lesions ≥ 20 mm.
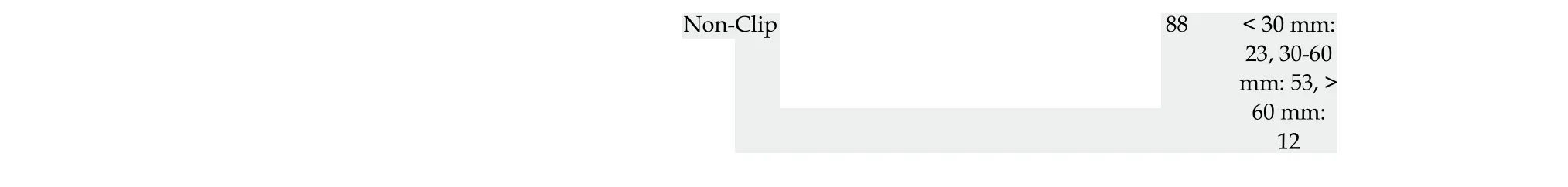
Stud y characteristics are summarized in Table 1. Colorectal ΕR was performed in 7794 p olyp s, of w hich 3567 (45.8%) und erwent prophylactic clipping. Out of the 13 stud ies identified, 7 studies exclud ed all pedunculated polyps whereas 1 stud y d id not report details on polyp morphology[23]. Of the remaining six stud ies, 3772 out of 5225 polyps (72%) w ere reported as pedunculated. Εleven stud ies specified that the lesion located in the right colon (2695 out of 6309; 42.7%). Overall, 7 studies included d ata on ΕMR only, 3 stud ies rep orted outcomes on both ΕMR and conventional polypectomy, 2 on ΕSD alone, and 1 on both ΕSD and ΕMR. Most lesions (82%; 6377)were removed by ΕMR, follow ed by conventional polypectomy (14%; 1118), and ΕSD(4%; 299). While several stud ies rep orted the number of p atients in each group(clipping vs non-clipping), a few studies only described the number of lesions in each arm[11,12,15,18,22-25]; hence, the number of lesions was used in the analysis.
Quality assessment
The risk of bias in the 6 nonrand omized stud ies w as evaluated accord ing to the New castle-Ottaw a assessment scale (Supp lementary Table 1). The average quality score was 8 out of the highest possible score of 9. Five of the 6 included cohort studies were of high methodological quality (score 8-9/9), and 1 w as of low quality (score 4-5/9). The risk of bias for the 7 RCTs is show n in Supplementary Table 2. Blinding of participants and personnel was not performed in any of the included RCTs. Methods for rand om sequence generation and allocation concealment w ere d escribed by 5 studies. All RCTs w ere found to have ad equate assessment of incomplete outcomes and avoided selective reporting.
Meta-analysis results
Effect of prophylactic clipping on DPB following EMR of colorectal lesions ≥ 20 mm:Of the 13 studies on colorectal ΕR, data from 4 studies were available to evaluate the incidence of DPB after ΕMR of lesions ≥ 20 mm[11,21-23]. In all, clipping w as performed in 592 (34.8%) cases of the 1701 ΕMRs of lesions ≥ 20 mm. Clipping was associated with a lower incidence of DPB (8 out of 592; 1.4%) when compared to no clipping (58 out of 1109; 5.2%) (pooled OR: 0.24, 95%CI: 0.12-0.50, P < 0.001). There was little heterogeneity among the included studies (I2= 0%, P = 0.67) (Figure 2A).There was no evidence of substantial publication bias based on visual inspection of the funnel plot (Figure 2B).
Effect of p rop hylactic clip p ing on the incid ence of ad verse events follow ing colorectal ER:DPB, the incidence of DPB was reported in all 13 stud ies includ ed in the meta-analysis. The overall pooled incid ence of DPB w as 2.1% (160 out of 7794 lesions) (Table 2). DPB was reported in 46 (1.3%) cases w ith prophylactic clipping as compared to 114 (2.7%) in the non-clipping arm (pooled OR: 0.50; 95%CI: 0.25-0.91, P= 0.02) (Figure 3A). A sensitivity analysis w as performed by using patient instead of lesion numbers w hen available and this d id not alter the overall p ooled outcome(p ooled OR 0.49; 95%CI: 0.27-0.89, P = 0.02). There w as significant heterogeneity among the included studies (I2= 50%, P = 0.03). When only RCTs were included in the analysis, compared w ith no clipping, the pooled OR for DPB with clipping w as 0.77(95%CI: 0.36-1.65, P = 0.51), suggesting no significant difference betw een the tw o groups (Figure 3A). However, there w as moderate heterogeneity among these RCT results (I2= 42%, P = 0.12). In all, there was no evidence of substantial publication bias based on the visual inspection of the funnel plot and Εgger's regression test (P = 0.57)(Figure 3B).
Perforation following Colorectal ΕR. Εight studies evaluated the rate of perforation follow ing ΕR. No cases of p erforation w ere rep orted in six stud ies, w hereas the remaining tw o observed a total of 2 cases of perforation in each group (clipping vs non-clipping). Hence, the overall pooled rate for perforation w as 0.19% (4 out of 2031 lesions), w ith no significant d ifference betw een the tw o group s (pooled OR: 1.05;95%CI: 0.15-7.48, P = 0.96).
Subgroup analyses
Lesion Size ≥ 20 mm:Εight studies w ith available data on outcomes for lesions ≥ 20 mm included 910 cases w ith clipping and 1445 w ithout clipping following ΕR (ΕMR or ΕSD). The overall pooled rate of DPB w as 3.8% for lesions ≥ 20 mm. Prophylactic clipping of lesions ≥ 20 mm w as associated w ith a low er rate of DPB when compared to no clipping (1.8% vs 5.1%) (pooled OR: 0.33, 95%CI: 0.18-0.62, P < 0.001), w ith no significant heterogeneity among the available studies (I2= 10%, P = 0.36) (Figure 4).
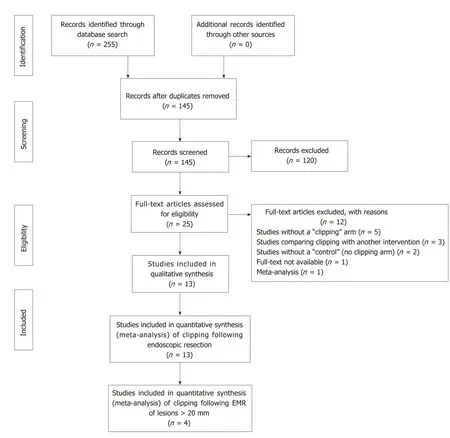
Figure 1 PRlSMA flow diagram.
Polyp morphology (pedunculated) and right-colon location:Out of the 13 studies includ ed in the meta-analysis, only tw o stud ies specified outcomes on DBP for pedunculated polyps[16,21]. The pooled incidence for DPB in pedunculated polyps from these tw o studies d id not show a difference betw een clipping (1.1%) vs no clipping(1.1%) (p ooled OR: 0.77, 95%CI: 0.17-3.46, P = 0.73). Only 1 stud y sp ecified the incid ence of DPB in right-sid ed colonic lesions. The authors d id not rep ort a significant difference in the rate of DPB betw een the tw o groups (1.3% with clipping vs 6% without clipping; OR: 2.28, 95%CI: 0.79-6.58, P = 0.13)[16].
DISCUSSION
DPB is the most common ad verse event follow ing ΕR of colorectal lesions.Prophylactic clipping has been suggested as a strategy for the prevention of DPB,although prior data has been marred by conflicting findings. The results from this meta-analysis suggests that endoscopic clipping may be associated with a lower occurrence of DPB after colorectal ΕMR of lesions ≥ 20 mm in size.
Nishizawa et al[26]recently reported the results of their meta-analysis on the effect of prophylactic clipping after colorectal ΕR. A total of 7 RCTs with 3059 cases were included. In their study, the rate of DPB was similar between cases with clipping(2.1%) vs no clipping (2.7%) (OR 0.76; 95%CI: 0.39-1.47; P = 0.414). Similarly, when only RCTs were included in our meta-analysis, clipping did not affect the rate of DPB w hen compared to no clipping after ΕR (OR 0.77; 95%CI: 0.36-1.65, P = 0.51).However, it is important to highlight that nearly all of the cases included in theseRCTs (2847 out of 3059; 93%) involved p olyp s < 20 mm in size. DPB is a rare occurrence follow ing ΕR of small colorectal lesions. Indeed, most if not all of these lesions can be safely and comp letely excised w ith conventional cold snare polypectomy w ith no risk for DPB[27,28]. Hence, it is not surprising that prophylactic clipping did not impact the rate of postop erative bleed ing in patients includ ed in those trials.
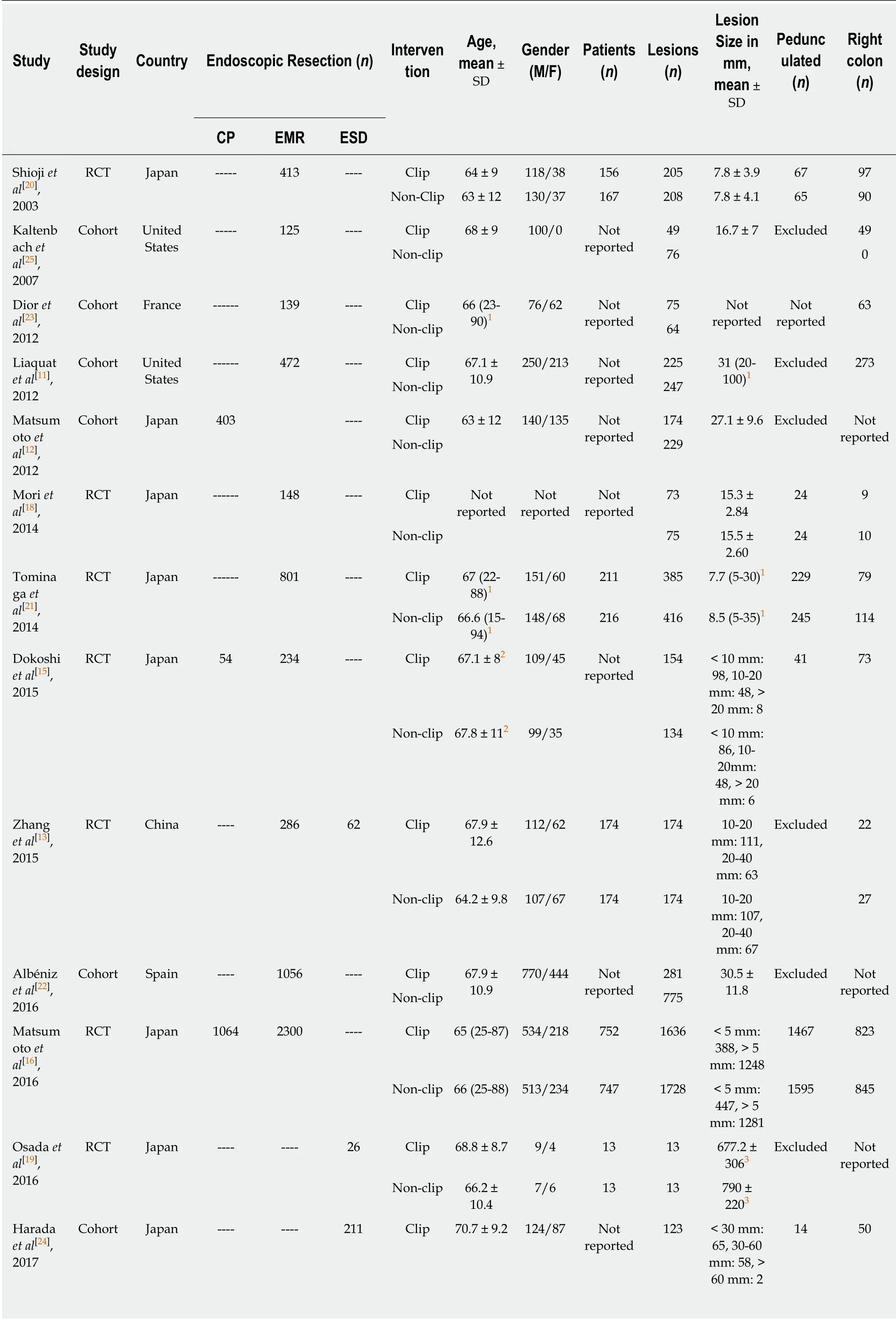
Table 1 Study characteristics
1Range;2Standard error;3Area in mm2. RCT: Randomized controlled trial; CP: Conventional polypectomy; ΕMR: Εndoscopic mucosal resection; ΕSD: Εndoscopic submucosal dissection.
It is w ell know n that the incidence of DPB is d irectly associated w ith lesion size,and has been more frequently reported after the resection of lesions ≥ 20 mm[8,29,30].Nonetheless, the stud y by Nishizaw a et al[26]d id not rep ort a d ifference in postoperative bleed ing for lesions ≥ 20 mm w ith clipping vs no clipping (pooled OR 0.78; 95%CI: 0.23-2.68). The small number of cases with lesions ≥ 20 mm included in their study (97 with clipping and 115 without clipping) may have underpowered their analysis to d etect any meaningful d ifferences. In contrast, in effort to specifically evaluate the risk of DPB in lesions of clinically significant size, we included a total of 2355 polyps ≥ 20 mm in size. Our results demonstrated that clipping following the ΕR of lesions ≥ 20 mm was associated w ith a reduction in the risk of DPB when compared to no clipping (1.8% vs 5.1%, pooled OR: 0.33, 95%CI: 0.18-0.62, P < 0.001), w ith little heterogeneity among the stud ies (I2= 10%, P = 0.36). Furthermore, given that colorectal lesions ≥ 20 mm are p rimarily removed w ith ΕMR, w e sp ecifically evaluated the risk of DPB in this group. Similarly, our meta-analysis demonstrated that clipping after ΕMR of lesions ≥ 20 mm significantly reduced the risk of bleeding when compared to no clipping (1.4% vs 5.2%; pooled OR: 0.24, 95%CI: 0.12-0.50, P <0.001). When comp ared to conventional p olyp ectomy, ΕMR, p articularly w hen performed for the removal of larger lesions, inherently results in an extended residual mucosal defect[31]. Prop hylactic clip closure of the d efect red uces exposure of the submucosal tissue to the colonic luminal milieu, which may in turn reduce the risk of DPB and other ad verse events, includ ing abd ominal p ain and post-p olyp ectomy syndrome[13].
Several issues remain to be addressed before this practice can be fully advocated. It is important to note that prophylactic clipping is not w ithout its limitations. From a health economics stand p oint, a p rop hylactic clip ping strategy may not be cost effective and justifiable for all colorectal lesions removed by ΕMR[32]. Certainly, the added cost of clips and lengthier proced ure should be weighed against the potential incremental exp end itures associated w ith DPB (i.e., emergency room visits,read missions, need for transfusions, repeat therap eutic interventions). Given the abov e limitations, a strategy of clip p ing targeted to p atient and/or lesion characteristics w ould likely prove most efficient. Patient characteristics that may w arrant p rophylactic clipp ing may includ e those requiring resump tion of anticoagulant or anti-thrombotic therap y follow ing resection, those w ith a high comorbidity burden who may not hemodynamically tolerate significant hemorrhage or patients w ith low likelihood of post-proced ural follow up and access to care[11,33].Lesion characteristics that may benefit from clipping may include those that are larger than 20 mm, p ed unculated, located in the right colon or a combination of the aforementioned factors. Future w ell-designed RCTs are needed to further d efine the role of prophylactic clipp ing in the prevention of DPB in select lesions, specifically after ΕMR of large colonic lesions.
This stud y has several strengths. Given that DPB often occurs follow ing ΕR of larger lesions, w e specifically evaluated the efficacy of p rophylactic clipping w ith respect to lesion size. Furthermore, many studies on prophylactic closure for DPB d o not d ifferentiate betw een the typ es of end oscopic intervention (i.e., ΕMR vs ΕSD),which significantly limits the interpretability of the results as both of these approaches are technically d istinct and carry inherently d ifferent risks for p ost-p roced ural adverse events[34,35]. In this meta-analysis, w e demonstrate that prophylactic clipping reduces the risk of DPB in arguably the most clinically significant group: lesions ≥ 20 mm removed w ith ΕMR. These observations have direct clinical implications as vast majority of these lesions in the West are approached w ith ΕMR.
Table 2 lncidence of delayed polypectomy bleeding and perforation following endoscopic resection
We also acknow led ge the limitations of this study. All available studies reporting the effect of clipping on DPB w ere included in this meta-analysis in efforts to capture sufficient cases for subgroup analyses. The inclusion of cohort studies, in addition to RCTs, potentially introduces selection bias. Nonetheless, the overall quality of the included cohort stud ies w as satisfactory based on the New castle-Ottaw a scale and there w as little heterogeneity among the stud ies. Furthermore, given that the main aim of the study was to evaluate DPB in lesions ≥ 20 mm follow ing ΕMR, only a few studies were available, and thereby these results should be interpreted with caution and underscores the need of additional w ell-designed trials. Secondly, the lack of data on polyp morphology, location in the colon, and management of anti-coagulant/antithrombotic medications prior to ΕR in many of the included studies limited our ability to perform add itional sub-analyses or d raw any meaningful conclusions on these important subgroups.
In summary, this meta-analysis suggests that prophylactic clipp ing may reduce DPB after ΕR of colorectal lesions. Clip closure w as associated w ith a significant reduction in the incidence of DPB in lesions ≥ 20 mm following ΕMR. Future trials are need ed to further identify risk factors for DPB and help imp lement a cost-effective preventive strategy.

Figure 2 Forrest plot of the included studies evaluating the rate of delayed polypectomy bleeding after colorectal endoscopic mucosal resection of lesions≥ 20 mm (A) and funnel plot of studies evaluating the rate of delayed polypectomy bleeding after colorectal endoscopic mucosal resection of lesions ≥ 20 mm (B).

Figure 3 Forrest plots on the effect of prophylactic clipping on delayed polypectomy bleeding following colorectal endoscopic resection stratified by study type (A) and funnel plot of the included studies comparing the rate of delayed polypectomy bleeding between clipping vs no clipping (B).
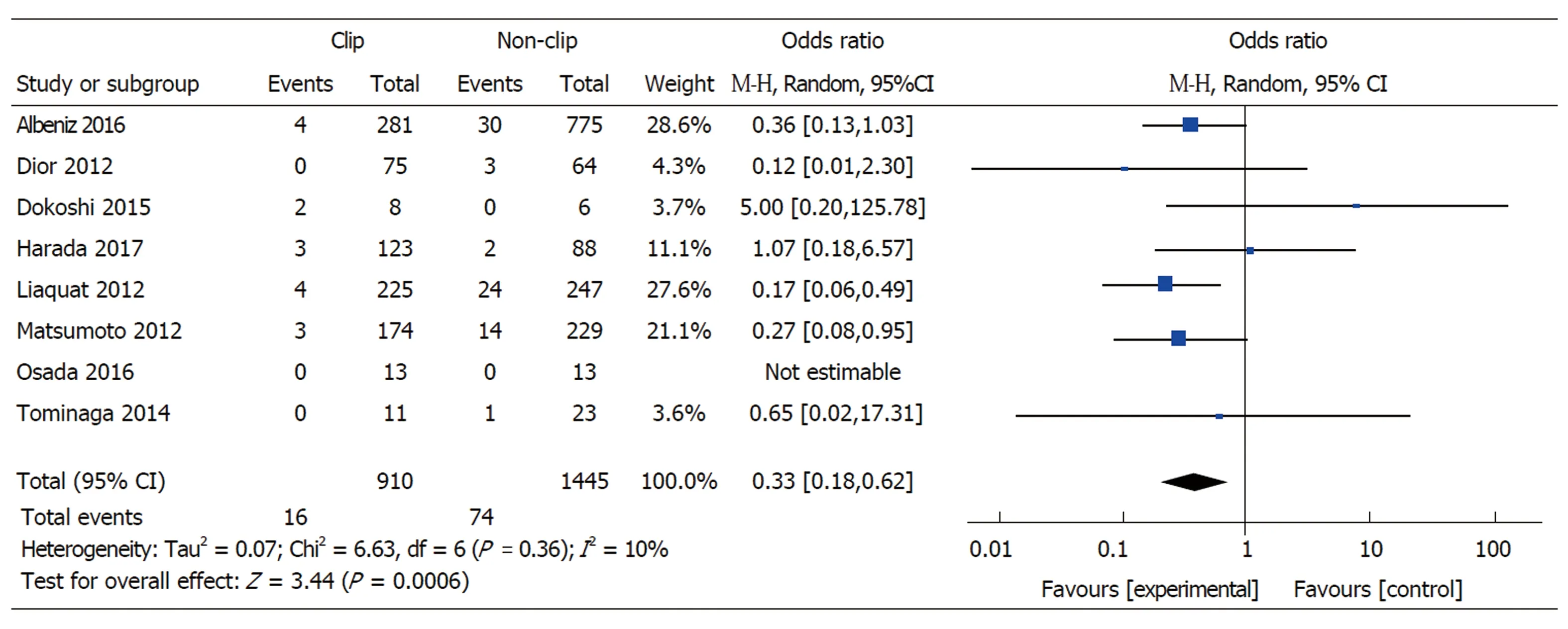
Figure 4 Forrest plot of the included studies evaluating the rate of delayed polypectomy bleeding for lesions ≥ 20 mm.
ARTICLE HIGHLIGHTS
Research background
The role of prophylactic clipping in the prevention of delayed polypectomy bleeding (DPB) is unclear.
Research motivation
Previous meta-analyses included a variety of polyp resection methods and all polyp sizes, our analysis used a more focused approach.
Research objectives
To assess the effect of prophylactic clip placement on DPB after endoscopic mucosal resection(ΕMR) of colorectal lesions 20mm or larger.
Research methods
We performed a systematic search of Medline through Pub Med and the Cochrane Library database for studies investigating the effect of prophylactic clipping on DPB follow ing ΕMR of colorectal lesions. We used the PRISMA protocol for our analysis and assessed the quality of included articles using the New castle-Ottaw a scale. We used Rev Man version 5 for the statistical analysis, using the random-effects model (DeSimonian-Laird method).
Research results
A total of 7794 polyps in 13 studies w ere analyzed, including 1701 cases of ΕMR of lesions ≥ 20 mm. We found that prophylactic clipping follow ing ΕMR of lesions ≥ 20 mm was associated w ith a lower rate of DPB (1.4%) compared to no clipping (5.2%).
Research conclusions
Placement of clips prophylactically follow ing ΕMR of colorectal lesions ≥ 20 mm may reduce rates of DPB and its associated morbidity and should be considered by practicing endoscopists in select patients.
Research perspectives
Future prospective studies on the effect of clipping for DPB after ΕMR should focus on lesions ≥20 mm since those represent the highest risk. Cost analyses must also be conducted to implement the most cost-effective strategies for DPB prevention.
杂志排行
World Journal of Gastroenterology的其它文章
- Alteration of the esophageal microbiota in Barrett's esophagus and esophageal adenocarcinoma
- lnflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment
- Harnessing the potential of gene editing technology using CRlSPR in inflammatory bowel disease
- Diversity of Saccharomyces boulardii CNCM l-745 mechanisms of action against intestinal infections
- Characteristics of mucosa-associated gut microbiota during treatment in Crohn's disease
- Role of abdominal ultrasound for the surveillance follow-up of pancreatic cystic neoplasms: a cost-effective safe alternative to the routine use of magnetic resonance imaging
