Nested case-control study on risk factors for opportunistic infections in patients with inflammatory bowel disease
2019-06-04ShanShanGongYiHongFanQingQingHanBinLvYiXu
Shan-Shan Gong, Yi-Hong Fan, Qing-Qing Han, Bin Lv, Yi Xu
Abstrac t BACKGROUND When opportunistic infections occur, patients with inflammatory bowel disease(IBD) commonly display a significantly increased rate of morbidity and mortality.With increasing use of immunosuppressive agents and biological agents,opportunistic infections are becoming a hot topic in the perspective of drug safety in IBD patients. Despite the well-established role of opportunistic infections in the prognosis of IBD patients, there are few epidemiological data investigating the incidence of opportunis-tic infections in IBD patients in China. Besides, the risk factors for opportunistic infection in Chinese IBD patients remain unclear.AIM To predict the incidence of opportunistic infections related to IBD in China, and explore the risk factors for opportunistic infections.METHODS A single-center, prospective study of IBD patients was conducted. The patients were followed for up to 12 mo to calculate the incidence of infections. For each infected IBD patient, two non-infected IBD patients were selected as controls. A conditional logistic regression analysis was used to assess associations between putative risk factors and opportunistic infections, which are represented as odds ratios (OR) and 95% confidence intervals (CIs).RESULTS Seventy (28.11%) out of 249 IBD patients developed opportunistic infections.Clostridium difficile infections and respiratory syncytial virus infections were found in 24 and 16 patients, respectively. In a univariate analysis, factors such as the severity of IBD, use of an immunosuppressant or immunosuppressants, high levels of fecal calprotectin, and C-reactive protein or erythrocyte sedimentation rate were individually related to a significantly increased risk of opportunistic infection. Multivariate analysis indicated that the use of any immunosuppressant yielded an OR of 3.247 (95%CI: 1.128-9.341), whereas the use of any two immunosuppressants yielded an OR of 6.457 (95%CI: 1.726-24.152) for opportunistic infection. Interestingly, when immunosuppressants were used in combination with infliximab (IFX) or 5-aminosalicylic acid, a significantly increased risk of opportunistic infection was also observed. The relative risk of opportunistic infection was greatest in IBD patients with severe disease activity(OR = 9.090; 95%CI: 1.532-53.941, relative to the remission stage). However, the use of IFX alone did not increase the risk of opportunistic infection.CONCLUSION Factors such as severe IBD, elevated levels of fecal calprotectin, and the use of immunosuppressive medications, especially when used in combination, are major risk factors for opportunistic infections in IBD patients. The use of IFX alone does not increase the risk of opportunistic infection.
Key words: Nested case-control study; Opportunistic infections; Inflammatory bowel disease
INTRODUCTION
Opportunistic infection refers to any infection caused by a weakened immune system and typically does not occur in people with normal immune function[1]. When they occur, p atients presenting w ith opportunistic infections commonly display a significantly increased rate of morbid ity and mortality. With increasing use of immunosuppressive agents and biological agents, opportunistic infections are becoming a hot topic in the perspective of drug safety in patients with inflammatory bowel disease (IBD). Studies have shown that opportunistic infections are closely related to the recurrence of IBD[2,3]. Severe opportunistic infection was observed in 3%of IBD patients, significantly increasing their mortality[4]. According to the consensus of The Εuropean Crohn's and Colitis Organization on opportunistic infections in IBD,IBD patients taking glucocorticoids, immunomodulators, and biologic therapies are all at an increased risk of opportunistic infection. Malnutrition and old age are also key risk factors for opportunistic infections[5]. A multicenter prospective study conducted in Japan followed 570 patients w ith IBD for one year and observed 52(9.1%) cases of opportunistic infection. Further analysis found that being over 50 years of age and the use of immunosuppressive agents are contributing risk factors for opportunistic infections in patients with IBD[6]. A study conducted by Tourner et al[7]also concluded that immunosuppressive medications and increased patient age are related with an increased risk of opportunistic infections in IBD patients. On the other hand, positive prevention, early diagnosis, and timely control of opportunistic infections are the current focuses for improving the prognosis of IBD patients.
Despite the well-established role of opportunistic infections in the prognosis of IBD p atients, there are few ep id emiological d ata investigating the incid ence of opportunistic infections in IBD patients in China. The level of fecal calprotectin (FC) is a commonly used d iagnostic measure for patients w ith IBD as its levels generally increase in patients with IBD. It is generally accepted that FC levels are a stable and reliable measure of IBD severity with a high sensitivity and specificity. How ever, the relationship betw een FC levels and the incidence of op portunistic infections in IBD has never been studied.
Therefore, this stud y sought to investigate the relationship betw een IBD and opportunistic infections from a cohort of patients with IBD using a nested case-control method. Specifically, we sought to predict the incidence of oppor-tunistic infections in p atients w ith IBD in China, and d etermine the relationship betw een FC and op portunistic infection, w ith an aim to provid e a scientific basis for the effective prevention and control of opportunistic infections in patients with IBD.
MATERIALS AND METHODS
Research design and patient groups
This study involving 301 IBD patients [139 with ulcerative colitis (UC) and 162 with Crohn's disease (CD)] enrolled from January to December 2017. The probability of an opportunistic infection w as calculated during a one-year follow-up period. Common opportunistic infections in patients w ith IBD include viral infections (herpes viruses,human p ap illomavirus, influenza v irus, and JC virus), bacterial infections(tuberculosis, nocardia, Clostridium difficile, pneumococcus, legionella, and listeriosis),fungal infections (histop lasmosis, cryp tococcosis, Pneumocystis jirovecii infection,asp ergillosis, and cand id iasis), and parasite infections (Strongyloides stercoralis)[8].Patients w ere screened for opportunistic infection before enrollment to exclude those currently infected. Infection w as based on laboratory results, in w hich viral IgM p ositivity and DNA cop y w ere d iagnosed as viral infection. The d iagnosis of tuberculosis w as based on the d etection of Tubercle bacillus. Clostridium difficile w as d etected by PCR. Positive fecal cultures of mold and cand id a w ere d iagnosed as fungal infections. Clinical visits were conducted once a month. Clinical follow-up and laboratory examinations [including routine blood examination, C-reactive p rotein(CRP), hepatic and renal function, FC, infection indicators, etc.] were conducted once a month. In add ition, d isease activity w as assessed at each follow-up. Truelove and Witts d isease severity classification criteria[9]and CD activity ind ex (CDAI)[10]w ere used to evaluate the disease activity of patients w ith UC and CD, respectively. These diagnoses and disease activity index were admitted by the attending physician.
This study w as ap proved by the ethics committee of First Affiliated Hosp ital of Zhejiang Chinese Medical University, and patients under the age of 16 were admitted to our study with the consent from their parents or guardians.
Case-control study
IBD patients with opportunistic infections were selected as the case group. For each case, two uninfected patients were chosen as controls and were matched according to age (at an interval of 10 years; ≤ 19, 20-29, 30-39,40-49, and ≥ 50 years).
Data collection
The demographic characteristics of patients were collected, including age, gender,course of the disease, current smoking habits, previous bowel surgery, comorbidity,disease activity, the type of IBD, and current medications. All patients were diagnosed with UC or CD based on the previously criteria[11].
Statistical analysis
Demographic characteristics w ere analyzed by the t-test. The univariate and multivariate analyses were performed with SPSS version 23 (SPSS, Tokyo, Japan).
RESULTS
IBD patients’ demographic and clinical features
A total of 301 IBD patients w ere enrolled in this stud y, 52 of w hom w ere lost to follow-up. Of the remaining 249 patients, 119 had UC and 130 had CD. The patients'ages ranged from 12 to 78 years (mean age, 45.24 years). During one year of followup, we found 70 IBD patients who developed an opportunistic infection (Table 1). The incidence of opportunistic infections w as 28.11%. Clostridium difficile infection w as found to be the most common opp ortunistic infection in patients w ith IBD (9.64%),follow ed by respiratory syncytial virus infection (6.43%). Fifteen (6.02%) and eleven(4.42%) patients w ere infected with Εpstein-Barr virus and Fungal, respectively. One patient developed active tuberculosis.
There w ere 70 p atients in the case group, includ ing 33 UC patients and 37 CD patients. In contrast, the control group consisted of 140 patients, includ ing 66 UC patients and 74 CD patients. Selected demographic and clinical characteristics of cases and controls are provided in Table 2. There were no statistically significant differences betw een the tw o groups in age, gend er, typ e of IBD, duration of IBD, d uration of medication use, prior surgery or smoking history. The data of the tw o groups w ere well balanced and comparable.
Severe disease activity is a risk factor for opportunistic infections in IBD patients
Patients' gend er, age, typ e of IBD, d uration of med ication, course of the d isease,history of prior surgery, and smoking habits w ere not related to increased risk of opportunistic infections, according to the univariate analysis. However, severe disease activity in IBD patients w as related to an increased rate of opportunistic infections (P< 0.001, OR = 18.404; 95%CI: 3.833-88.375). Multivariate analysis also indicated that severe IBD w as the greatest risk factor for opportunistic infections (P < 0.001, OR =18.404; 95%CI: 3.833-88.375).
Elevated level of FC is a risk factor for opportunistic infections in IBD patients
In our study, FC higher than normal levels (>200 µg/g) was related to an increased risk of opportunistic infections both in our univariate analysis (P < 0.001, OR = 4.431;95%CI: 2.265-8.667) and multivariate analysis (P = 0.023, OR = 2.467; 95%CI: 1.133-5.373).
Immunosuppressive medications, especially when used in combination, are risk factors for opportunistic infections in IBD patients
Compared w ith the use of 5-aminosalicylic acid (5-ASA), the use of infliximab (IFX) or 5-ASA+ IFX w as not related to the incid ence of op p ortunistic infections in our univariate analysis (Table 3) and multivariate analysis. On the contrary, the use of any immunosup p ressant (steroid s, azathiop rine, tacrolimu s, thalid omid e, or methotrexate) was related to a significantly increased odd for opportunistic infection,compared with the use of 5-ASA both in univariate analysis (P < 0.047, OR = 2.668;95%CI: 1.012-7.033) (Table 3) and multivariate analysis (P = 0.029, OR = 3.235; 95%CI:1.125-9.306) (Figure 1). Εspecially w hen tw o or more immunosuppressants were used in combination, it rep resented the second largest risk factor for op p ortunistic infections in both univariate analysis (P < 0.001, OR = 10.375; 95%CI: 2.948-36.508)(Table 3) and multivariate analysis (P = 0.006, OR = 6.462; 95%CI: 1.727-24.172)(Figure 1). In ad dition, the use of 5-ASA and any immunosuppressant(s) or IFX with any immunosuppressant(s) was related to significantly increased infection rates both in univariate analysis (P < 0.01) (Table 3) and multivariate analysis (P < 0.05) (Figure 1).
High levels of CRP and erythrocyte sedimentation rate (ESR) are not related to a significantly increased risk of opportunistic infection
Our univariate analysis showed that high levels of CRP (OR = 3.98; 95%CI: 1.994-7.944) and ΕSR (OR = 3.744; 95%CI: 1.87-7.494) were related to an increased risk of opportunistic infections (Table 3). However, the results of multivariate analysis did not confirm this finding (Figure 1).
DISCUSSION
In our study, we prospectively predicted the occurrence of opportunistic infections in IBD patients. A total of 70 (28.11%) of the 249 patients developed opportunistic infections. Currently, there are few epidemiological data on the rate of opportunistic infection in IBD patients in China. In a study performed at Ruijin Hospital affiliated to Shanghai Jiao Tong University, of 130 patients with IBD, 12.3% developed CD infection[12]. In another study, positive serum IgG for cytomegalovirus (CMV) was found in 73% of UC patients in Wuhan, China and 89% of CD patients, and the rate in the healthy population was 50.69%[13]. Data from Peking Union Medical College Hospital indicated that the CMV infection rate in UC patients undergoing surgical operations w as 46.2%[14], compared to 36.7% among refractory UC patients in Tianjin[15]. A multicenter prospective study conducted in Japan included 570 IBD patients who were followed for one year, and the authors observed 52 cases (9.1%) of opportunistic infection[7]. Separately, a national study in France found that theincid ence of op portunistic infections in IBD patients w as 7.9% after five years of follow-up[16]. The high incidence of opportunistic infection in IBD patients in China may be related to the level of economic d evelopment and the abuse of antibiotics. In most regions of China, exp ensive biological agents are not covered by med ical insurance, which limits their extensive use in China. How ever, most immunosuppressants, such as steroids and azathioprine, are cheap and are accepted by the majority of IBD p atients. China is know n to be one of the countries w ith the w orst rates of antibiotic abuse in the w orld. It is estimated that China produced 248000 tons of antibiotics in 2013[17], and the per capita consumption of antibiotics was 10 times that of the United States[18]. The direct consequence of abuse of antibiotics is w idespread bacterial d rug resistance, w hich results in an increased rate and severity of opportunistic infections.
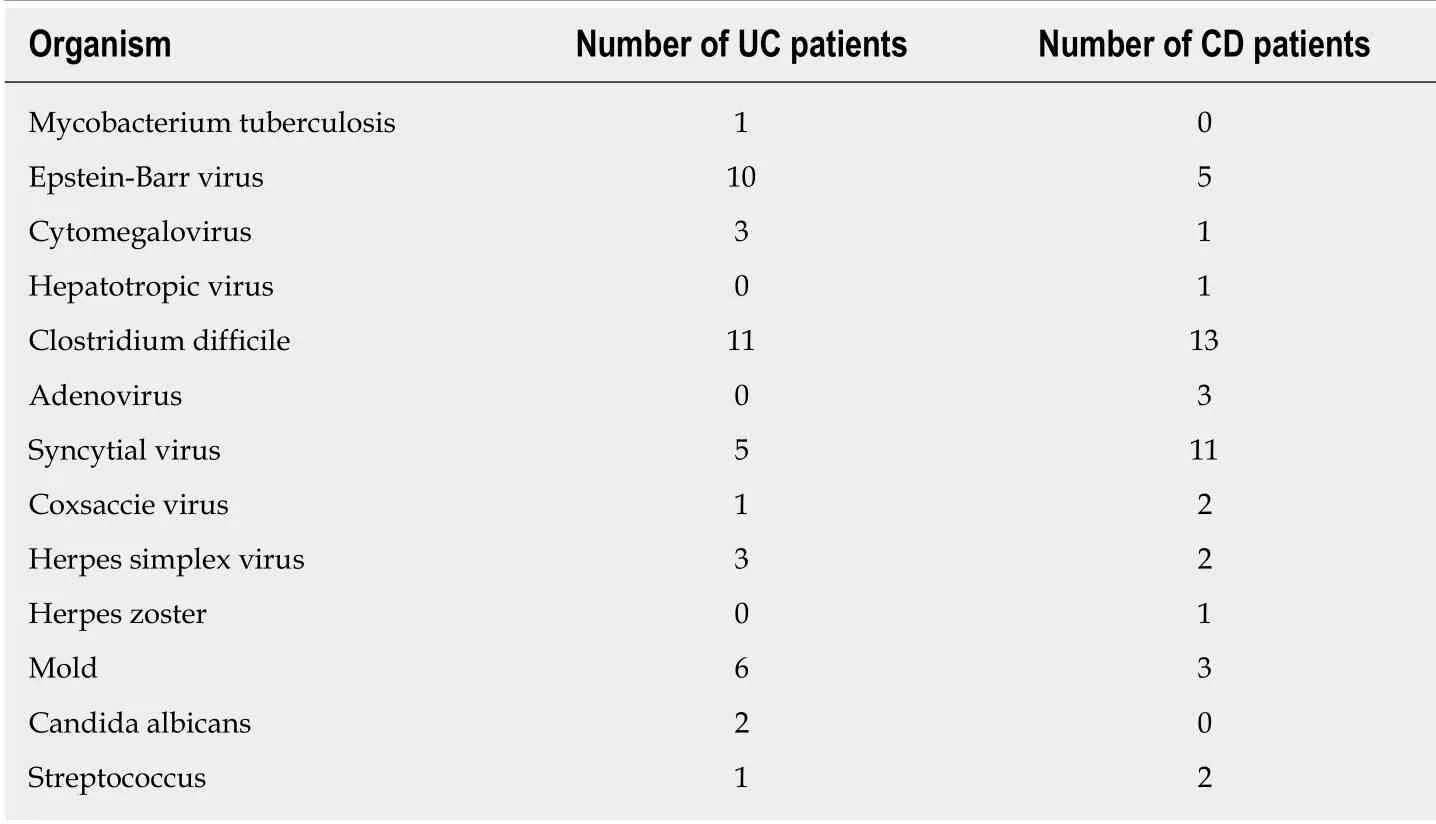
Table 1 Opportunistic infections in inflammatory bowel disease patients evaluated between January 1, 2017 and December 31, 2018
Infection w ith Clostridium difficile, an anaerobic, gram-positive bacillus, is the most common nosocomial infection w hich w as most commonly observed in the IBD patients in our study (9.64%). IBD patients are at an increased risk for infection with Clostridium difficile[19-23]. Comp ared w ith those w ith IBD alone, p atients w ith Clostridium difficile and IBD had longer hosp ital stay, requiring colon surgery intervention[24,25]. The use of antibiotics is closely related to Clostridium difficile associated d iarrhea. Antimicrobials may disrupt the normal gastrointestinal flora,leading decreased colonization resistance and allowing toxigenic strains of Clostridium difficile to cause d iseases. The abuse of antibiotics in China is serious. In addition, IBD patients are often treated with antibiotics for IBD deterioration or immunosuppressive complications, so Clostridium difficile infection can easily occur. Clostridium difficile is an increasing problem in immunocompromised patients, w hich can lead to higher rates of colectomy and mortality[26]. Clostridium difficile infection initiates w ith d isruption of normal colonic microbiota, for w hich IBD patients are at high risk,conferring them an additional risk of Clostridium difficile infection[27,28]. In our pooled analysis, Clostridium difficile has the highest infection rate among op p ortunistic infections in IBD p atients d u e to the extensiv e u se of antibiotics and immunosuppressive agents.
Our stud y found that d isease severity w as also a risk factor for op p ortunistic infections in IBD patients. Previously, the relationship between disease activity and the incidence of opportunistic infections w as not clear. We speculate that w hen IBD patients progress to late-stage disease, a nonspecific inflammatory reaction is initiated in the gut mucosa, p romoting p athogen invasion. The invasion of p athogens subsequently aggravates intestinal inflammation, creating a positive feed back loop.Furthermore, the increased energy consumption and low immunity state ind uced byinflammation diminish IBD patients' ability to resist external pathogens, leading to further opportunistic infection.
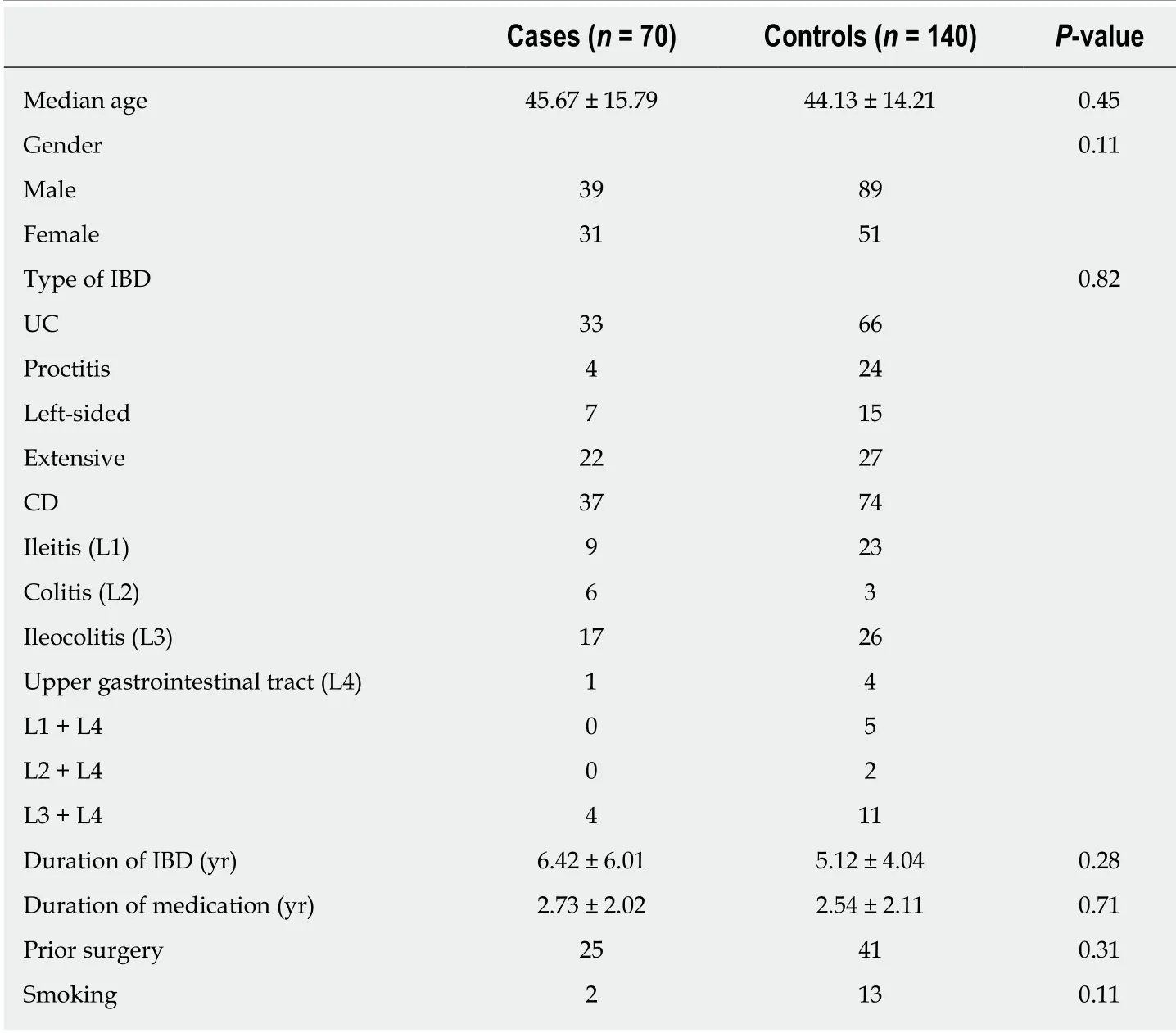
Table 2 Demographic and clinical features of inflammatory bowel disease patients with (cases)and without (controls) opportunistic infection
A reliable measure of long-term outcome is paramount in predicting the course of the disease, responsiveness to treatment, potential for complications, and need for hospitalization and/or surgery[29]. Many stud ies have show n that mucosal healing is the best p red ictor of p ositive long-term outcomes[30-33]. Εnd oscop y is currently regarded as the gold standard test for the assessment of mucosal healing[34]. However,its invasive nature and high cost make it an unfeasible mod ality for frequent monitoring. Calprotectin is an abund ant calcium-bind ing protein, w hich is d erived mainly from neutrophils and a lesser extent monocytes and reactive macrophages. FC is a sensitive marker of intestinal inflammation in IBD, as its concentration reflects the migration of neutrophils into the intestinal cavity[35]. Thus, FC has emerged as a novel d iagnostic tool to d etect and monitor intestinal inflammation and reflect d isease activity in IBD. Measurements for FC are simp le, rap id, sp ecific, sensitive, and inexp ensive compared to its counterp arts[36,37]. Along w ith CRP, ΕSR, and FC, our study discovered that elevated FC w as a risk factor for opportunistic infections in IBD patients. One explanation for this finding may be that the level of FC serves as an indicator for intestinal inflammation and therefore, disease activity. This makes FC level a more sensitive and specific marker than CRP and ΕSR. When the level of FC in IBD patients is elevated, it suggests that intestinal inflammation has occurred and the disease is in an active stage, conferring the patient to opportunistic infections.
In ou r stu d y, im mu nosu p p r essiv e agents inclu d ed methotrexate, 6-mercaptopurine, azathioprine, thalidomide, tacrolimus and steroids. From this study,we have found that the use of immunosup pressive medications alone increased the risk of an opportunistic infection about 3.247-fold. When any two immunosuppressive medications were used in conjunction, the risk w as increased greatly to about 6.457-fold. This result from our study is consistent with recent results in the literature[7,8,38,39].Add itionally, it w as d etermined that w hen immunosuppressive medications w ere combined with 5-ASA or IFX, the risk of opportunistic infection w as increased greatly to about 4 to 5 fold s. This conclusion is consistent w ith the find ings reported by Tourner et al[7], Lawrance et al[40], and Kirchgesner et al[16].
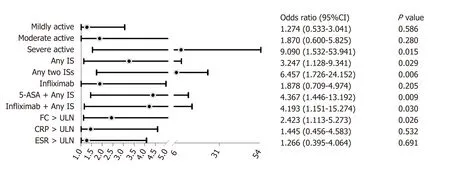
Figure 1 Risk factors for opportunistic infection in inflammatory bowel disease patients (multivariate analysis). 5-ASA: 5-aminosalicylic acid; IS:Immunosuppressant (steroids, thiopurine, thalidomide, tacrolimus, or methotrexate); FC: Fecal calprotectin; CRP: C-reaction protein; ESR: Erythrocyte sedimentation rate; ULN: Upper limit of normal; CI: Confidence interval. P-values and 95% confidence intervals (CIs) for mild, moderate, and severe disease were compared with remission. P-values and 95%CIs for any immunosuppressant (IS), any two IS, infliximab, 5-aminosalicylic acid (5-ASA) + any IS, and infliximab + any IS were compared with 5-ASA.
The relationship betw een biologics and op p ortunistic infections has not been clearly established. Some studies[41-44]indicated that biologics increase the incidence of opportunistic infections, while others do not support this conclusion[45,46]. In our study,we found no association between the use of IFX alone and the increased risk of opportunistic infections. One possible explanation is that IFX may not cause opportunistic infections within the one-year period of the study (shorter than the previous five-year period)[7].
Despite the important findings, this study had several limitations. First, the sample size of our study was small. A larger sample size would have allowed for more accurate estimation of the incidence of opportunistic infections and increase in reliability of risk factors in Chinese IBD patients. Second, our study was a singlecenter clinical study, which cannot represent the situation of IBD patients in China as a whole.
In conclusion, severe disease activity, elevated levels of FC, and immunosuppressive med ications, especially when used in combination, are risk factors for opportunistic infections in IBD patients. The use of IFX alone has nothing to do with opportunistic infections. With the increasing use of immunosuppressants in IBD and the advocacy of combination therapy, patients and physicians need to pay attention to and prevent opportunistic infections. As the genetic background, living environment,lifestyle, and d iet of IBD patients in China are different from those in Western countries, our study of opportunistic infection could provide vital information for clinicians and IBD patients in China and other countries.
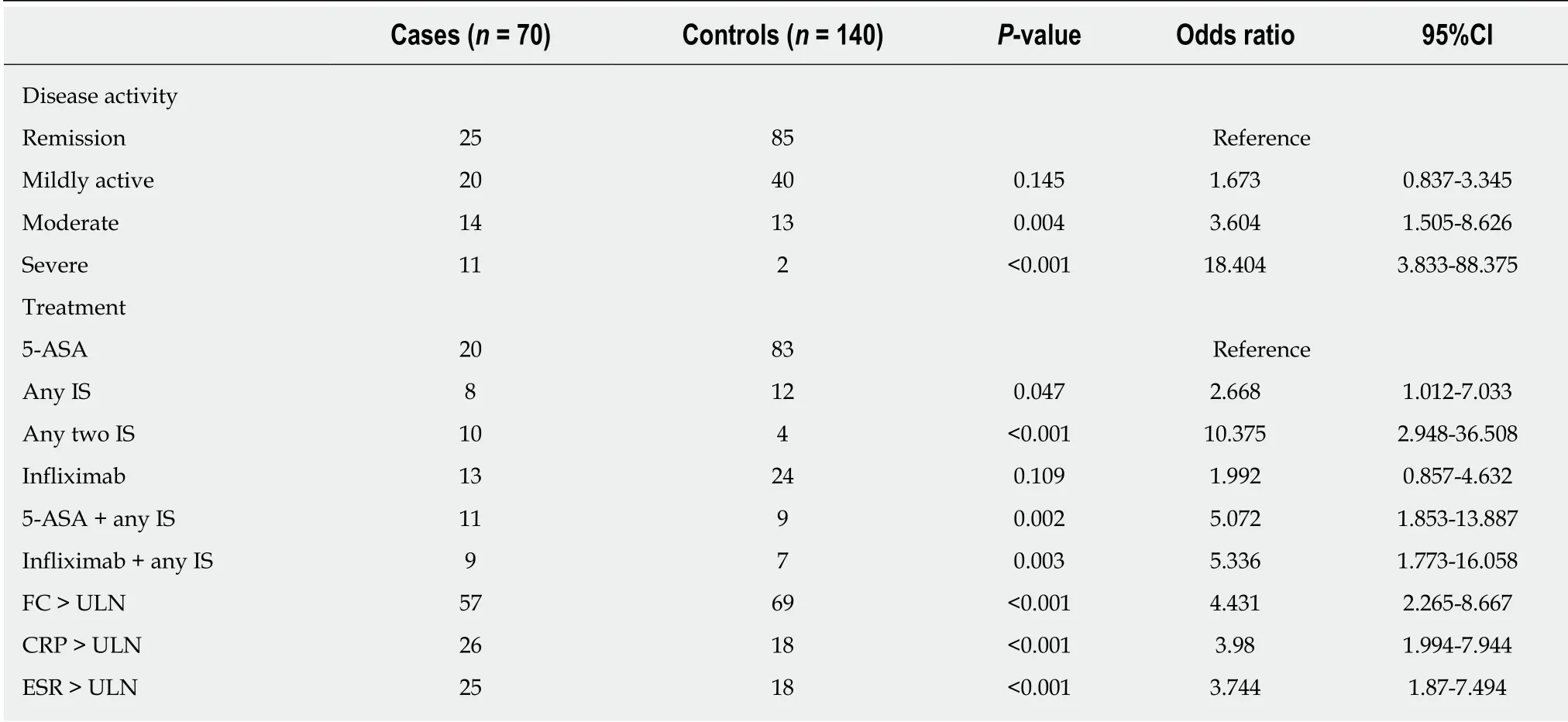
Table 3 Risk factors for opportunistic infection in inflammatory bowel disease patients (univariate analysis)
ARTICLE HIGHLIGHTS
Research background
Opportunistic infection refers to any infection caused by a w eakened immune system and typically does not occur in people w ith normal immune function. When they occur, patients presenting w ith opportunistic infections commonly display a significantly increased rate of morbidity and mortality. A number of studies have been conducted in Western countries and Japan to investigate the incidence of and risk factors for opportunistic infection in inflammatory bow el disease (IBD) patients. Currently, there are few epidemiological data on the rate of opportunistic infection in IBD patients in China. The risk factors for opportunistic infection in Chinese IBD patients remain unclear.
Research motivation
The main topics in our study are to predict the incidence of opportunistic infections related to IBD in China, and explore the risk factors for opportunistic infections. The key problems to be solved is to ensure compliance of enrolled IBD patients. The significance of solving these problems for future research in this field is to more accurately predict the incidence of and risk factors for opportunistic infections.
Research objectives
The main objectives in our study w ere to predict the incidence of opportunistic infections related to IBD in China, and explore the risk factors for opportunistic infections. The realized objectives include that the incidence of opportunistic infection in IBD patients in China is higher than that in Western countries and factors such as severe IBD, elevated levels of fecal calprotectin, and the use of immunosuppressive medications, especially w hen used in combination, are major risk factors for opportunistic infections in IBD patients, according to our single-center study. The significance of realizing these objectives for future research in this field is to alert patients and physicians to pay attention to and prevent opportunistic infections. Meanw hile, our study can provide important information for clinicians and IBD patients in China and other countries.
Research methods
The research design that w as adopted to realize the objectives is observational study and nested case-control study. Observational study is to observe and record the characteristics of research objects in a natural state, and describe and compare the results. In our study, the patients w ere follow ed for up to 12 mo to identify the incidence of infections. In nested case-control studies,cases and controls come from the same cohort, so the selection bias in effect estimation is reduced and comparability is good. For each infected IBD patient, tw o non-infected IBD patients w ere selected as controls in our study.
Research results
Our study found that the incidence of opportunistic infection in IBD patients in China is higher than that in Western countries and factors such as severe IBD, elevated levels of fecal calprotectin, and the use of immunosuppressive medications, especially w hen used in combination, are major risk factors for opportunistic infections in IBD patients. Meanwhile, the use of infliximab alone does not increase the risk of opportunistic infection. Our findings remind patients and physicians to pay attention to and prevent opportunistic infections. As the genetic background, living environment, lifestyle, and diet of IBD patients in China are different from patients in Western countries, our study of opportunistic infection could provide important information for clinicians and IBD patients in China and other countries. The follow ing problems remain to be solved: (1) Our study w as a single-center clinical study, w hich cannot represent the situation of IBD patients in China as a w hole; and (2) the sample size of this study for both ulcerative colitis and Crohn's disease patients w as small. A larger sample size w ould have allow ed for more precise estimation of the incidence of opportunistic infections and increase in reliability of risk factors in Chinese IBD patients.
Research conclusions
The new findings of this study are that the incidence of opportunistic infection in IBD patients in China is higher than that in Western countries, according to our single-center study, and factors such as severe IBD, elevated levels of fecal calprotectin, and the use of immunosuppressive medications, especially w hen used in combination, are major risk factors for opportunistic infections in IBD patients. Meanw hile, the use of infliximab alone does not increase the risk of opportunistic infection. The original insights into the current know ledge that this study offered is w hen opportunistic infection occurs, patients commonly display a significantly increased rate of morbidity and mortality. Therefore, prevention and identification of opportunistic infections are critical. The implications of this stud y for clinical practice in the future is patients and physicians need to pay attention to and prevent opportunistic infections.
Research perspectives
From this study, we can conclude that the incidence of opportunistic infection in IBD patients in China is higher than that in Western countries, and doctors should pay attention to and prevent the incidence of opportunistic infections. The future research direction is to conduct a multicenter study to evaluate the incidence of opportunistic infection in Chinese IBD patients, and more accurately screen out the risk factors leading to the occurrence of opportunistic infection in Chinese IBD patients, so as to effectively prevent the occurrence of opportunistic infection.
杂志排行
World Journal of Gastroenterology的其它文章
- Alteration of the esophageal microbiota in Barrett's esophagus and esophageal adenocarcinoma
- lnflammatory bowel diseases and spondyloarthropathies: From pathogenesis to treatment
- Harnessing the potential of gene editing technology using CRlSPR in inflammatory bowel disease
- Diversity of Saccharomyces boulardii CNCM l-745 mechanisms of action against intestinal infections
- Characteristics of mucosa-associated gut microbiota during treatment in Crohn's disease
- Role of abdominal ultrasound for the surveillance follow-up of pancreatic cystic neoplasms: a cost-effective safe alternative to the routine use of magnetic resonance imaging
