Hydroxyurea-induced cutaneous squamous cell carcinoma:A case report
2019-04-22YanXuJianLiu
Yan Xu, Jian Liu
Yan Xu, Jian Liu, Department of Surgical Oncology, The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou 310003, Zhejiang Province, China
Abstract
Key words: Hydroxyurea; Squamous cell carcinoma; Primary Myelofibrosis; Case report
INTRODUCTION
Hydroxyurea (HU) is a non-alkylating antineoplastic agent first synthesized in 1869 by Dressler and Stein.It is currently used to treat leukemia, sickle cell anemia,psoriasis, and chronic myeloproliferative disorders[1].Following a large-scale drug screen, it has also been used as an anti-tumor agent for the management of head and neck cancers, malignant melanoma, and brain tumors.Moreover, HU is listed as an“essential medicine” by the World Health Organization[2].
HU is a well-established inhibitor of DNA synthesis.It is mainly active in the Sphase of the cell cycle by suppressing ribonucleoside reductase, which plays a vital role in catalyzing the synthesis of deoxyribonucleotides from ribonucleotides[1].Inactivation of ribonucleoside reductase can slow the movement of DNA polymerase at replication forks and decreases deoxyribonucleotide triphosphate levels[3].Hence,HU depletes intracellular deoxynucleotide pools, which leads to impairment of DNA synthesis and repair.
There have been numerous reports of cutaneous complications during long-term maintenance therapy with HU.Common cutaneous side effects include hyperpigmentation, xerosis, alopecia, atrophy of the skin, nail changes, facial and acral erythema, palmar or plantar keratoderma, and leg ulcers[4].However, to date,fewer than 20 cases of HU-related cutaneous squamous cell carcinoma (cSCC) have been reported.Early diagnosis and evaluation are critical for determining optimal treatment regimens.Herein, we describe an additional case of cSCC associated with long-term HU therapy.
CASE PRESENTATION
Chief complaints
A 67-year-old Asian woman with a history of primary myelofibrosis presented with a painful non-healing chronic ulcer on her left ankle of 2 years duration.
History of present illness
The patient had primary myelofibrosis for 20 years and was initially treated with HU at a dose of 1 g/d.
History of past illness
Appendectomy was performed 10 years ago.
Personal and family history
The patient had no significant family history.
Physical examination upon admission
There was extensive photodamage and atrophy on the dorsal hands.The lesions on the hands consisted of multiple scabs, the largest scab on the right hand measured 1 cm × 2 cm (Figure 1).The irregularly shaped ulcer on the left ankle was 9 cm × 7 cm in size with an ill-defined margin (Figure 2).
Laboratory diagnosis
Laboratory investigations showed that the patient had marked leukocytosis (84.5 ×109/L), a raised neutrophil count (60.8 × 109/L) and platelet count (488 × 109/L), and a low erythrocyte count (2.1 × 1012/L).

Figure 1 Skin lesions on both hands.
FINAL DIAGNOSIS
A pathological examination of the surgical specimen revealed a well-differentiated squamous cell carcinoma with evidence of abundant cytoplasmic keratin pearls(Figure 3).
TREATMENT
Although surgeons considered performing resection of cSCC on her left foot and coverage with skin grafts, the operation was deemed too risky due to the high likelihood of failure and incomplete excision.Thus, the patient underwent a successful below-the-knee amputation followed by preventive right groin nodal dissection.
OUTCOME AND FOLLOW-UP
The postoperative course was uneventful with no recurrence after 12 mo of follow-up.Dermatologic changes on both hands secondary to HU therapy were extensively treated.
DISCUSSION
Long-term HU therapy is a rare cause of cSCC.In total, only 18 cases, including our patient, have been reported in the literature (Table 1).Disdieret al[5]first reported a patient with cSCC after HU treatment in 1991.In these reports, four primary diseases(primary myelofibrosis, polycythemia vera, essential thrombocythemia, and chronic myelocytic leukemia) and a wide age range (from 45 to 81 years) were presented.There was no significant sex difference in these cases (10 of 18 cases were men).Lesions were commonly located on the scalp, face, and extremities.Most patients had no history of precursor lesions or skin cancers, which rendered HU as the most likely culprit.Patients with HU-related cSCC typically showed symptoms after a latency period of approximately 2 to 13 years.HU treatment withdrawal, Mohs surgery,multiple debridements, and ablation were usually necessary to heal leg ulcers, but in five cases, the above therapies did not result in wound closure.It is suggested that the skin toxicity of HU is a long-term cumulative process and will persist after drug withdrawal, which could be defined as late toxicity.However, the mechanisms underlying the occurrence of HU-related cSCC are mostly unknown, but two pathogenic mechanisms have been proposed to explain this association.
Ultraviolet (UV) irradiation is most likely the primary factor leading to the development of cSCC.In vitro, HU inhibits natural DNA repair in UV-irradiated human skin fibroblasts and directly induces chromosome damage, which further interferes with cell replication in the basal layer of the epidermis[6,7].In vivo, HU transforms free radical nitrogen oxides that may produce high oxidative stress in patients’ epithelial tissues and cooperates with UV in DNA damage, peroxidation of membrane lipids, and signal transduction pathway changes[8].The synergistic effect of HU and UV radiation provides an ideal environment for the formation of cSCC.In addition, HU can markedly elevate p53 levels in basal layer keratinocytes, which increases the risk of skin cancers[9].This pathogenic mechanism could explain the occurrence of cSCC in photoexposed skin.
A chronic wound environment characterized by prolonged inflammation undoubtedly plays another critical role in HU-associated cSCC[9].Lower limb ulceration is a significant adverse reaction caused by long-term administration of HU.Several pathogenetic hypotheses (DNA inhibition theory, tarombokinesis, and microcirculation rheology theory) could explain the formation of lower limb ulcers.It is well-known that chronic skin damage, including ulcers, burn sites, and scars, is associated with an increased incidence of skin cancer[10].In addition to the case reported here, 11 articles refer to the presence of cSCC on extremities, which are different from the light exposure area.Hence, chronic inflammation may be another main cause of cSCC in these patients.

Figure 2 Skin lesions on left ankle.
CONCLUSION
Taken together, these findings indicate that long-term HU administration can lead to the development of cSCC, probably through synergistic effects with UV or chronic inflammation.Hence, patients should be informed of the potential cutaneous toxicities of HU treatment in advance.Closer dermatologic follow-up is advisable,particularly in patients with continuous HU therapy and a long history of sun exposure.Moreover, regular protection against UV rays should be emphasized.When cSCC is identified, HU treatment withdrawal is necessary, and we recommend prompt replacement therapy as required.The skin toxicity of HU is considered late toxicity, and patients should be monitored for many years after HU discontinuation.

Table 1 Hydroxyurea-related cutaneous squamous cell carcinoma

HU:Hydroxyurea; PMF:Primary myelofibrosis; PV:Polycythemia vera; ET:Essential thrombocythemia; CML:Chronic myelocytic leukemia; CR:Complete remission; PR:Partial response; cSCC:Cutaneous squamous cell carcinoma.
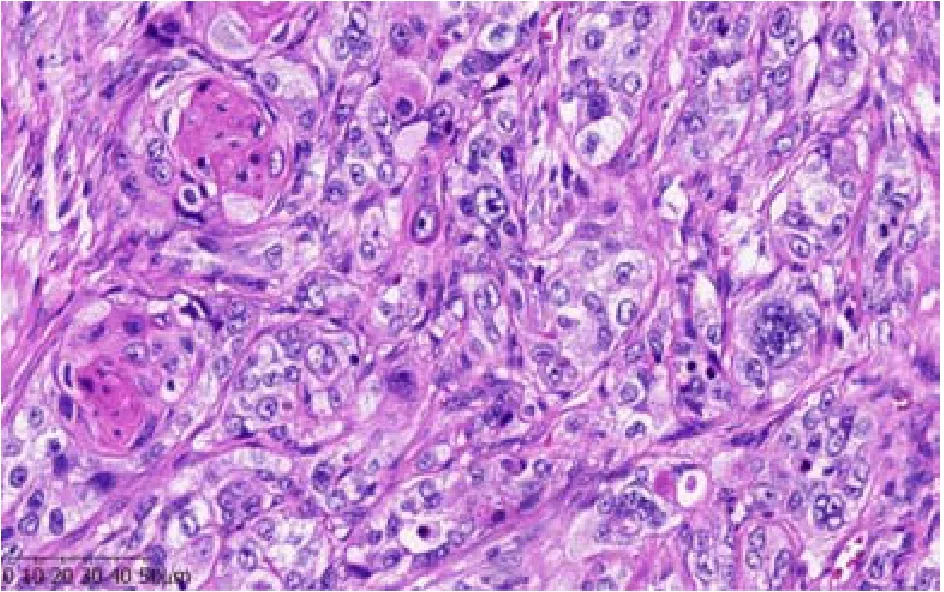
Figure 3 Pathologic findings indicating pure, well-differentiated squamous cell carcinoma with evidence of abundant cytoplasmic keratin pearls.
ACKNOWLEDGEMENTS
The authors thank all the treatment groups of the Department of Surgical Oncology,The First Affiliated Hospital, College of Medicine, Zhejiang University, Hangzhou,China.
杂志排行
World Journal of Clinical Cases的其它文章
- Overview of organic anion transporters and organic anion transporter polypeptides and their roles in the liver
- Value of early diagnosis of sepsis complicated with acute kidney injury by renal contrast-enhanced ultrasound
- Value of elastography point quantification in improving the diagnostic accuracy of early diabetic kidney disease
- Resection of recurrent third branchial cleft fistulas assisted by flexible pharyngotomy
- Therapeutic efficacy of acupuncture combined with neuromuscular joint facilitation in treatment of hemiplegic shoulder pain
- Comparison of intra-articular injection of parecoxib vs oral administration of celecoxib for the clinical efficacy in the treatment of early knee osteoarthritis
