Comprehensive and innovative techniques for laparoscopic choledocholithotomy: A surgical guide to successfully accomplish this advanced manipulation
2019-04-20TomohideHori
Tomohide Hori
Abstract Surgeries for benign diseases of the extrahepatic bile duct (EHBD) are classified as lithotomy (i.e., choledocholithotomy) or diversion (i.e.,choledochojejunostomy). Because of technical challenges, laparoscopic approaches for these surgeries have not gained worldwide popularity. The right upper quadrant of the abdomen is advantageous for laparoscopic procedures,and laparoscopic choledochojejunostomy is safe and feasible. Herein, we summarize tips and pitfalls in the actual procedures of choledocholithotomy.Laparoscopic choledocholithotomy with primary closure of the transductal incision and transcystic C-tube drainage has excellent clinical outcomes;however, emergent biliary drainage without endoscopic sphincterotomy and preoperative removal of anesthetic risk factors are required. Elastic suture should never be ligated directly on the cystic duct. Interrupted suture placement is the first choice for hemostasis near the EHBD. To prevent progressive laceration of the EHBD, full-layer interrupted sutures are placed at the upper and lower edges of the transductal incision. Cholangioscopy has only two-way operation; using dedicated forceps to atraumatically grasp the cholangioscope is important for smart maneuvering. The duration of intraoperative stone clearance accounts for most of the operative time. Moreover, dedicated forceps are an important instrument for atraumatic grasping of the cholangioscope. Damage to the cholangioscope requires expensive repair. Laparoscopic approach for choledocholithotomy involves technical difficulties. I hope this document with the visual explanation and literature review will be informative for skillful surgeons.
Key words: Laparoscopic surgery; Choledocholithotomy; Bile duct; Laparoscopy; General surgery
INTRODUCTION
Laparoscopic surgery has been adopted in various fields[1-8]. Laparoscopic surgery has substantial advantages over open surgery, including less blood loss, less pain, lower morbidity rates, shorter time to a postoperative diet, shorter hospital stay, earlier social reintegration and modest cost savings[1,4,9-13]. Laparoscopic surgeries that do not require advanced techniques such as anastomotic reconstruction or lymphoid dissection (e.g., appendectomy, cholecystectomy, distal pancreatectomy and rectopexy)[3,5-7]have rapid learning curves[11]. Hence, laparoscopic surgeries are widely used worldwide for benign diseases[5,7].
Unfortunately, laparoscopic hepatobiliary and pancreatic (HBP) surgery has developed slowly because of technical challenges and a protracted learning curve[9,14],with the exception of laparoscopic cholecystectomy[15,16]. Acute cholangitis (choledocholithiasis) is itself a benign disease, but associated cholangiovenous reflux and subsequent sepsis can easily result in a life-threatening situation[17-19]. Surgical treatments for benign diseases of the extrahepatic bile duct (EHBD) are classified according to their therapeutic purpose as lithotomy (i.e., choledocholithotomy) or diversion (i.e., choledochojejunostomy)[20,21]. General surgeons do not perform these surgeries laparoscopically because they require advanced skills and anatomical precision[22-26], although a laparoscopic approach is safe and feasible for choledocholithotomy and choledochojejunostomy[22,25-31].
The basic skills required for open surgeries are clearly different from those used in laparoscopic procedures[7,8,14,32-34]. Notably, experience alone is not enough to ensure successful performance of laparoscopic surgeries[7,8,14,32-24]. We herein focus on laparoscopic approaches for choledocholithotomy, summarizing tips and pitfalls of this advanced surgery, on the basis of a review of important studies and our own experience. Also, important previous documents in this field are carefully reviewed.
ANATOMICAL RECOGNITION OF THE BILIARY SYSTEM
The anatomy of the biliary system is shown in Figure 1A. The common hepatic duct(CHD), common bile duct (CBD) and intra-pancreatic bile duct compose the EHBD.The cystic duct contains Heister's valves (spiral folds). The gallbladder infundibulum and cystic duct meet to form the infundibulum-cystic duct junction. The CHD, cystic duct and CBD together constitute the biliary confluence. Biliary drainage is physiologically regulated by Oddi's sphincter.
ACUTE OBSTRUCTIVE SUPPURATIVE CHOLANGITIS
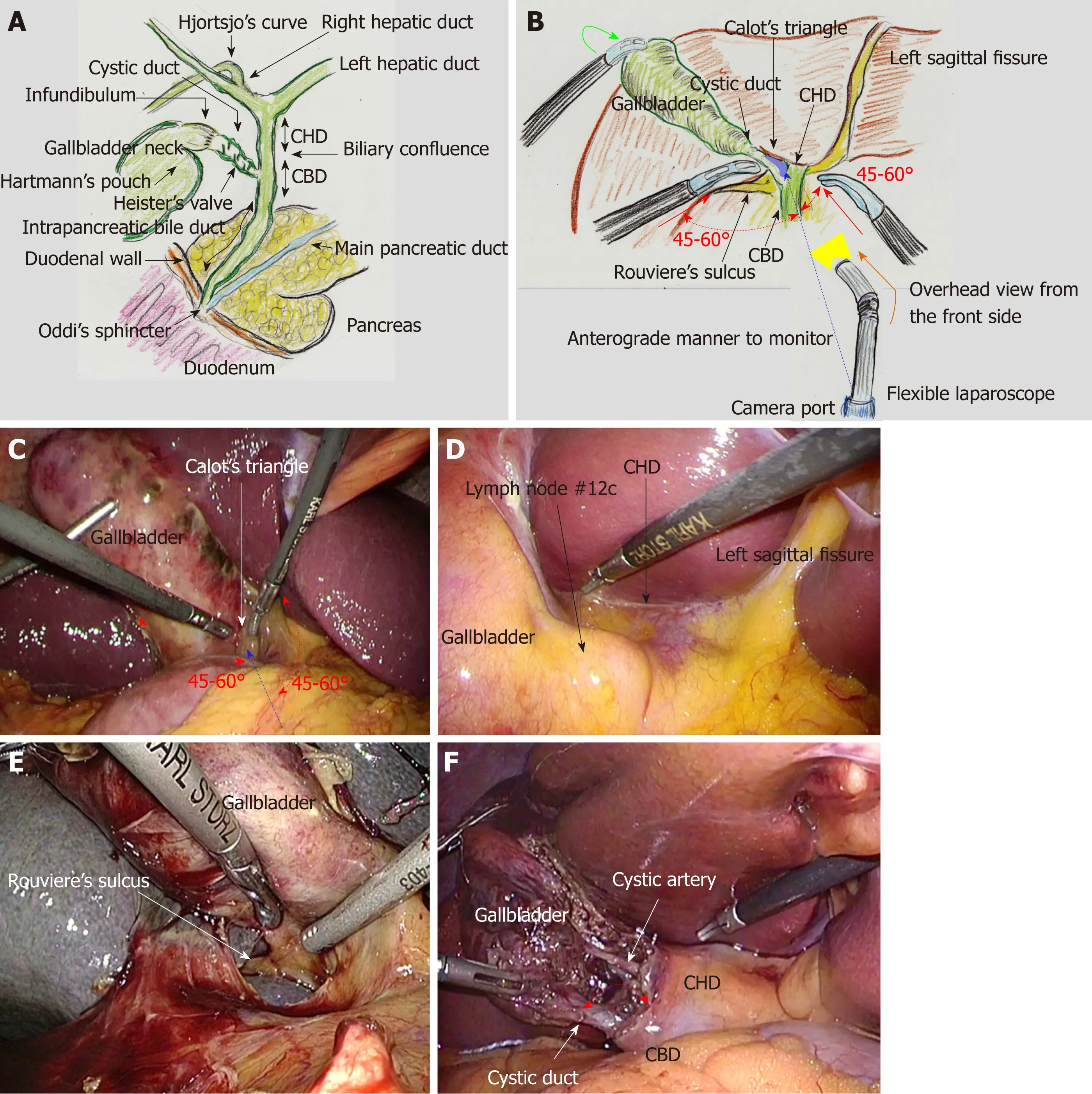
Figure 1 Biliary system and actual surgical procedures of laparoscopic choledocholithotomy.
Charcot first documented acute cholangitis in 1877[35]; Charcot's triad (upper abdominal pain, fever and jaundice) was proposed for diagnosis of acute cholangitis[36,37]. Biliary stagnation caused by obstruction [e.g., stone, tumor, liver failure or dysfunction of Oddi's sphincter (DOS)] or bacterial infection with increased biliary pressure easily result in cholangiovenous reflux and subsequent sepsis[17,18].Reynolds and Dargan classified a clinical syndrome characterized by Charcot's triad,lethargy (or mental confusion) and shock state as acute obstructive cholangitis in 1959[38]. Thereafter, these five symptoms were called Reynold's pentad[39]. Reynolds and Dargan suggested that the only way to treat this severe cholangitis was emergent surgery and biliary drainage[38]. Longmire first defined severe cholangitis fulfilling Reynold's pentad as acute obstructive suppurative cholangitis (AOSC) in 1971[40]. The high mortality rate of AOSC (8%-71%) has been do-cumented[41-44].
AOSC commonly occurs in elderly patients[42,44]; emergent biliary drainage is required in these patients[19]. Interventional endoscopists may choose endoscopic sphincterotomy (EST). EST destroys the physiological function of Oddi's sphincter,even in elderly patients with subtle DOS. This situation raises a simple question. Is EST the first choice for emergent biliary drainage, even in younger patients? EST alone is not required as initial treatment[45], and we should not forget that EST destroys the physiological function of Oddi's sphincter. Recovery of the physiological function of Oddi's sphincter is impossible after EST. To preserve physiological function, elective surgery has advantages over emergent EST; transpapillary biliary drainage without EST may be performed initially as emergent therapy[45].
ACUTE CHOLANGITIS AND BILE DUCT STONES
Initial management of acute cholangitis with bile duct stones has been documented[19,45]; biliary drainage should be performed as soon as possible in these patients[19]. The clinical indications and therapeutic techniques of biliary drainage for acute cholangitis have been clearly established[45]. Endoscopic transpapillary biliary drainage, whether via nasobiliary drainage or biliary stenting, should be selected as first-line therapy[45]. EST is not routinely recommended for biliary drainage alone because of concerns about bleeding[45].
DOS and anatomical abnormalities (e.g., periampullary diverticulum) result in acute biliary infection, and subsequently cause primary bile duct stones[46]. The etiology of bile duct stones should be recognized preoperatively. In patients with concomitant bile duct stones, stone removal can be performed via an endoscopic approach (e.g., EST, papillary dilation and balloon enteroscopy-assisted and/or ultrasonography-guided methods)[45]or with surgical treatment[47-49]. Laparoscopic choledocholithotomy is considered a safe and feasible therapeutic option[22,26-28,31]. As described above, AOSC frequently occurs in elderly patients[42,44]; laparoscopic surgery should be chosen even in this population.
In patients whose condition is stable before surgery, both emergent and elective laparoscopic surgeries are safe and feasible[50]. Perioperative analgesic agents are important; however, some analgesic agents (e.g., opioids or morphine) cause druginduced DOS[51,52]. Effective biliary drainage should be achieved preoperatively to avoid sepsis[19,45], as should compete removal of risk factors for general anesthesia (e.g.,unstable hemodynamic state, obstructive jaundice, sepsis and analgesic contraindications)[53-55].
BILE DUCT STONES AND ASSOCIATED CHOLANGITIS AFTER ABDOMINAL SURGERY
Acute cholangitis and bile duct stones are critical problems after abdominal surgery,especially in elderly patients[28,56,57]. Gastrectomy surgically alters the biliary system,because the inevitable dissection of lymph nodes and nerves results in physiological disorders (e.g., DOS, reduced bile secretion, atonic gallbladder and paralytic bowels)[7,58]. Hence, repeated cholangitis and bile duct stones easily occur after gastrectomy[57,59].
Severe adhesions and dense tissue are often intractable during reoperative surgery.Moreover, the location of important ducts and vessels may easily be shifted after gastrectomy because of digestive anastomosis and postoperative adhesions, especially in Billroth I reconstruction[7]. However, a laparoscopic approach is advantageous,even for re-operative choledocholithotomy[28,59], and is a safe, effective and feasible treatment even in elderly patients after complicated abdominal operations[56].Laparoscopic choledochoduodenostomy (not choledochojejunostomy) may be chosen as an alternative treatment, if gastrojejunostomy has been performed in the Roux-en-Y fashion[57,60]. Laparoscopic cholecystectomy should be the first choice for gallbladder stones and cholecystitis in patients with a history of abdominal surgery[7,8,61], although cholecystectomy after EST for biliary duct stones does not reduce the incidence of recurrent cholangitis[62].
HISTORY OF CHOLEDOCHOLITHOTOMY AND BILIARY DRAINAGE
Abbe first performed bile duct drainage after choledocholithotomy in 1892[63,64];Deaver reported use of a modified T-tube drain in 1904[63,64]. Kehr propounded the usefulness of T-tube drainage in 1909[63-67]; thereafter, transductal T-tube drainage after choledocholithotomy became commonly used worldwide. The material of the T-tube is important, because low reaction in either the EHBD or the peritoneal cavity results in a lack of tissue tract formation around the tube due to material inertness[63,64].Various vulcanized rubber products can be produced from natural rubber and sulfur.The degree of vulcanization influences the hardness and irritant nature of the resulting rubber[64]. Red rubber is the most irritant and silicone rubber is the least[63,64,68].Latex rubber tubes are preferred for long-term drainage, because they create a good tissue tract as a result of tissue reaction against the material irritant[63,64]. Silicone rubber T-tubes often fail to elicit tissue tract formation[63,64,68]. Red or latex rubber should be chosen as T-tube material[63,64,68].
Acute cholangitis can be managed with transpapillary biliary drainage, EST,transductal drainage (T-tube) or transcystic drainage (C-tube)[22]. Transductal T-tube drainage has higher rates of stone clearance and biliary leakage than other treatment options[22]. EST has a higher rate of procedural morbidities and serious consequences may occur[22]. Transcystic C-tube drainage is an accessible technique that simplifies surgical procedures and has a lower complication rate than other treatments[22]. The choice of choledocholithotomy via conventional open surgery with transductal T-tube drainage versus laparoscopic primary closure with transcystic C-tube drainage remains controversial[69]. Currently, laparoscopic choledocholithotomy with primary closure and transcystic C-tube drainage is superior to conventional open surgery with transductal T-tube drainage[69], which has inspired HBP surgeons to end the use of transductal T-tube drainage[47,49,70].
INTENTIONAL PRESERVATION OF PHYSIOLOGICAL FUNCTION OF ODDI'S SPINCTER
EST destroys the physiological function of Oddi's sphincter, and moreover, recovery of the physiological function of Oddi's sphincter is impossible after EST. Even though emergent EST is easier than elective laparoscopic surgery, transpapillary biliary drainage without EST is the initial treatment for acute cholangitis[45]. Completion of EST results in destruction of the physiological function of Oddi's sphincter. Illconsidered use of EST should be avoided[20], though many physicians may consider that the arguments against EST is really limited. To preserve sphincter function,emergent EST should be performed only in special situations (e.g., elderly patients with critical comorbidities, severe disease, prolonged jaundice, or severe DOS resulting from previous surgeries[20,71]. Paradoxically, EST may be permissive in patients who already have DOS. For example, elder or postoperative patients may have severe DOS[7,57-59].
RECURRENT STONES AND ASSOCIATED CHOLANGITIS
Recurrent stones (not remnant stones) in the bile duct after choledocholithotomy or EST is another critical matter[20,57,72]. Early stone recurrence after surgical or endoscopic treatment is a dreaded occurrence for physicians[20,57]. Though laparoscopic choledocholithotomy provides safe and feasible treatment for recurrent stones and associated cholangitis[28,30,56,59].
As described above, DOS, reduced bile secretion and paralytic bowels raise concerns about recurrent stones and associated cholangitis; elective laparoscopic cholecystectomy after complete removal of bile duct stones does not reduce the recurrence rate of repeat cholangitis[62]. The etiology of bile duct stones should be carefully evaluated and therapeutic strategies should be chosen according to definitive or suggested etiology. Though the arguments against endoscopic managements of bile duct stones may be really limited and laparoscopic choledocholithotomy is a safe and feasible treatment even for recurrent stones[28,30,56,59],laparoscopic choledochojejunostomy may be a possible therapeutic option to provide biliary diversion according to physiological disorders[20,30].
PREOPERATIVE EVALUATION OF BILE DUCT STONES
Stone clearance should be achieved without any remnant stones or debris[73].Specialized instruments, including endoscope and forceps, are crucial for successful surgical stone removal[74,75]. Clearance of some stones (e.g., impacted, multiple or intrahepatic stones) involves technical challenges[76]. Operative time is greatly affected by the duration of stone removal[73,74]; detailed preoperative imaging studies shorten operative time[77]. Removal of impacted and/or large stones is especially difficult[27,73],although even an impacted stone will float after preoperative biliary drainage[76].Preoperative evaluation with endoscopic retrograde cholangiography or cholangiography via drainage tube is strongly recommended[78]. The presence of a duodenal parapapillary diverticulum, which causes DOS and contraindicates EST,should also be ruled out preoperatively[79].
TECHNICAL DIFFICULTY OF LAPAROSCOPIC SURGERIES OF THE EHBD
Gallbladder stones with acute cholecystitis is an indication for surgery[7,8,80]; inflammatory severity may be an important risk factor in these cases[81,82]. Extrinsic compression of the EHBD, including Mirizzi syndrome and hidden cystic duct, make laparoscopic cholecystectomy technically difficult[81,83]. However, the concept of the critical view of safety (i.e., positive identification of the cystic duct and artery) has been established in 1995[34]. Compliance with this protocol makes laparoscopic cholecystectomy safe, even in severe cholecystitis[7,8]. The right upper quadrant provides a suitable location for the surgical field in laparoscopic procedures[7,30,84],which is one reason laparoscopic cholecystectomy has spread worldwide[15,16]. Reliable stability during laparoscopic cholecystectomy is indispensable for successful laparoscopic choledocholithotomy[7,8,32,34,81].
However, technical challenges have prevented laparoscopic surgeries for the EHBD(e.g., choledocholithotomy and choledochojejunostomy) from gaining worldwide popularity[22,23]. These advanced surgeries should be mastered by skillful HBP surgeons[24,25]. Although laparoscopic choledocholithotomy and choledochojejunostomy[22,25-31]are safe and feasible, technical challenges have prevented the worldwide dissemination of these advanced HBP surgeries[22-26].
ACTUAL SURGICAL PROCEDURES OF LAPAROSCOPIC CHOLEDOCHOLITHOTOMY
The patient is placed in a supine position. Carbon dioxide pneumo-peritoneum at 10 to 12 mmHg is achieved through an umbilical port. Transductal incision is accompanied by bile outflow, and cholangioscopy requires continuous saline flow for intraluminal observation. A saline irrigator and suction tip (StrykeFlow, Stryker Co.,Kalamazoo, MI, United States) are used. Frequent, continuous suction is needed during laparoscopic choledocholithotomy, though suction causes collapse of pneumoperitoneum. Pneumoperitoneum stability is very important to maintain the surgical field during laparoscopic surgery[85]. Therefore, we employ an automatically maintained pneumoperitoneum system (AirSeal Intelligent Flow System, Conmed Co., Utica, NY, United States). A flexible laparoscope with an adequate light source(Endoeye Flex, Olympus, Tokyo, Japan) is required; laparoscopic procedures are performed under various angled views.
A total of four working ports are placed in the upper abdomen. An assistant surgeon retracts the gall bladder fundus ventrally. The target site is Calot's triangle;both forceps of the main surgeon make adequate angles (approximately 45°-60°)relative to the axis from the camera port to Calot's triangle (Figure 1B and C). An excessively narrow or wide angle complicates laparoscopic procedures, including fully intracorporeal suture[7]. Moreover, a flexible laparoscope provides an overhead view from the upper anterior aspect, anterograde to the visual monitor (Figure 1B and C). Hence, the right upper quadrant is highly suitable for set-up of surgical procedures[7,30,84]. Surgeons should not hesitate to place additional ports if needed,because stab incisions are minimally invasive[7].
The liver is held cranially with a snake retractor located below the xiphoid process.The hepatoduodenal ligament is well stretched[7]. The hepatorenal fossa is widely dilated, and a working space is obtained. The bottom plateau of the U-shaped line from the left sagittal fissure to the gallbladder, which necessarily involves the CHD(Figure 1D), and Rouviere's sulcus, which always involves the right hepatic duct(Figure 1E), are routinely confirmed.
The whiter color change at the junction of the infundibulum and cystic duct is recognized[7](Figure 1F). The angle between the cystic duct and CHD is widened to prevent a tenting injury resulting from a parallel junction of these biliary ducts[7,32,34,81,86](Figure 1F). The critical view of safety is established on both the anterior (Figure 2A)and posterior aspects (Figure 2B)[33,87].
Pneumoperitoneum pressure caused by infiltration of carbon dioxide gas helps to create a dissectible layer. To avoid unexpected injuries, the dissectable layer should be traced as close to the gallbladder as possible[7]. Tissue dissection and membrane cutting should be extended from the visualized side of the correct layer, not from the unseen side[7]. The gallbladder is then removed from the liver bed.
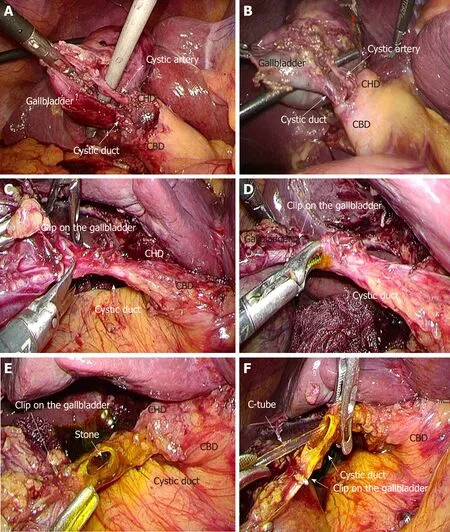
Figure 2 Actual surgical procedures of laparoscopic choledocholithotomy.
The cystic duct is straightened and a semicircular incision is made on the cystic duct near the gallbladder (Figure 2C). Full cutting with removal of the gallbladder disturbs further procedures. Heister's valves are carefully destroyed before transcystic placement of a C-tube into the EHBD (Figure 2D) and removal of stones from the cystic duct (Figure 2E). Careless stabbing procedures to destroy Heister's valves can easily result in severe injury to the posterior walls of the biliary confluence or EHBD.The golden brown bile flows from the EHBD, after which the C-tube is cannulated(Figure 2F). The C-tube can be used as a cholangiographic tube for intraoperative cholangiography. Elastic suture is not ligated directly to avoid overtightening of the C-tube; insufficient drainage will trigger postoperative complications. Optimal transcystic fixation of the C-tube is completed with elastic suture and clips[7](Figure 3A-C); the second clip prevents slippage of the first clip[7](Figure 3D).
During laparoscopic cholecystectomy, the CHD, biliary confluence and CBD should be recognized, but direct exposure of these structures should be avoided[7,8]. However,these biliary structures should be intentionally explored during laparoscopic choledocholithotomy (Figure 3E). Although blunt dissection is carefully completed to explore the wall of the EHBD, intentional dissection of the autonomic nerves for biliary malignancies is not required for benign biliary diseases[88,89]. Feeding and drainage vessels surrounding the EHBD should be preserved to prevent ductal necrosis and postoperative biliary leakage (Figure 3F)[7]. The EHBD is opened with sharp dissection (Figure 4A); energy devices should not be used, to avoid even mild thermal damage. Intra-corporeal suture placement and subsequent ligation at the bleeding point are the first choice for hemostasis near the bile duct wall (Figure 4B). If oozing is intractable at the anterior wall of the EHBD, a button-shaped electrode with suction used in conjunction with a soft-coagulation system (VIO, Erbe, Tübingen,Germany) is an effective tool for safe hemostasis. After opening of the EHBD, the inner cavity of the EHBD is sufficiently flushed to raise biliary stones (Figure 4C).Thereafter, all stones are completely removed[90](Figure 4D).
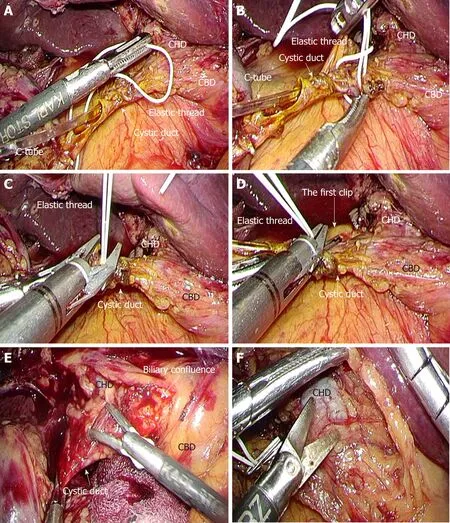
Figure 3 Actual surgical procedures of laparoscopic choledocholithotomy.
After transductal incision along the long axis, interrupted absorbable monofilament sutures (PDS II, 4-0, violet, SH-1, Ethicon Inc., Bridgewater, NJ, United States) are placed through all layers at the upper and lower edges of the incision to prevent progressive laceration resulting from subsequent procedures, including cholangioscope maneuvers (Figure 4E and F). Thereafter, extracorporeal sutures are placed bilaterally with absorbable monofilament suture (PDS II, 4-0, violet, SH-1, 90 cm, Ethicon Inc.) as fixation sutures to open the transductal orifice (Figure 5A and B).These fixation sutures are adequately set through the abdominal wall at different points from the laparoscopic trocars with a trocar site closure device (Endo Close;Medtronic, Dublin, Ireland) (Figure 5C).
Spilled stones and/or infected bile should be completely removed[90]. Intraoperative cholangioscopy through the laparoscopic trocar is essential for laparoscopic choledocholithotomy. Dedicated elastic forceps to adequately grasp the cholangioscope without damaging the special coating and to allow maneuvering of the cholangioscope for stone removal (A66070A, 10 mm, Olympus or CLICKline BERCI,K33531 PG, 10 mm; Karl Storz Endoskope, Tuttlingen, Germany) is a key tool for successful laparoscopic choledocholithotomy (Figure 5D). Direct grasping with conventional laparoscopic forceps results in irreparable damage to the endoscope surface and should be avoided. Intraluminal findings should be carefully observed via the cholangioscope. Bifurcation of the bilateral hepatic ducts at the CHD side (Figure 5E) and the characteristic findings (so-called ‘actinia') of the end of the intrapancreatic bile duct at the CBD side (Figure 5F) should be confirmed.
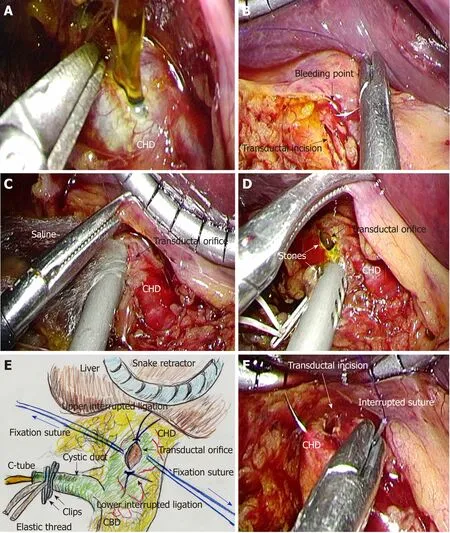
Figure 4 Actual surgical procedures of laparoscopic choledocholithotomy.
The diameter of the EHBD is generally > 10 mm[31]; the method of primary closure of the transductal incision is chosen according to the EHBD diameter[91-93]. Generally,both the transductal incision closure and subsequent primary closure are performed in the same direction along the long axis (Figure 6A). In cases of EHBD diameter less than 7 to 8 mm, primary closure is performed in the direction of the short axis to avoid postoperative stenosis (Figure 6B). The transductal incision is primarily closed with intra-corporeal ligation, with primary full-layer interrupted sutures of absorbable monofilament suture (PDS II, 5-0, violet, RB-1; Ethicon, Inc.).
Finally, real-time intraoperative cholangiography via C-tube is performed with contrast agent and atoxic dye (indigo carmine or indocyanine green). Remnant stones,biliary leakage and passage obstruction are carefully checked. Biliary passages,especially through the primary-closed portion and Oddi's sphincter, are evaluated during surgery. Intraperitoneal lavage and drain placement are usually performed;total bilirubin level in the drain discharge is monitored after surgery.
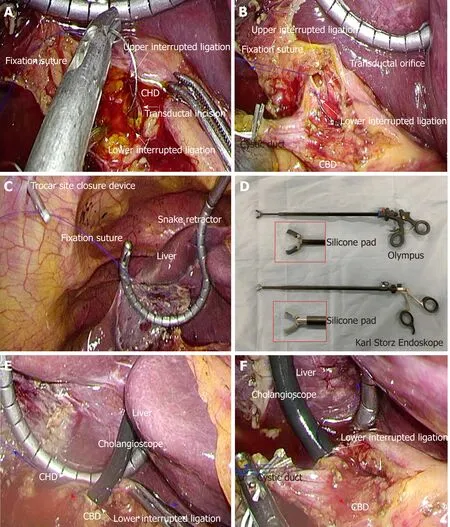
Figure 5 Actual surgical procedures of laparoscopic choledocholithotomy.
AVOIDANCE OF A MISIDENTIFICATION OF THE EHBD AND CYSTIC DUCT DURING LAPAROSCOPIC CHOLEDOCHOLITHOTOMY
In a patient who has a history of laparotomy, severe adhesions and dense tissue are often intractable (Figure 6C and D). Moreover, the location of important ducts and vessels may be shifted. Intraoperative recognition of a “second cystic duct” or an“accessory duct” strongly indicates misidentification of the cystic and CHD[32].Intraoperative cholangiography is the recommended solution to detect this misidentification[32]. Identification of Hjortsjo's curve is a helpful way to detect the branches from the right hepatic duct[7,70]. Although there is no evidence for routine cholangiography[34], laparoscopic surgeons should not hesitate to perform intraoperative cholangiography when indicated[94-98].
IMPORTANCE OF THE SPECIALIZED FORCEPS TO
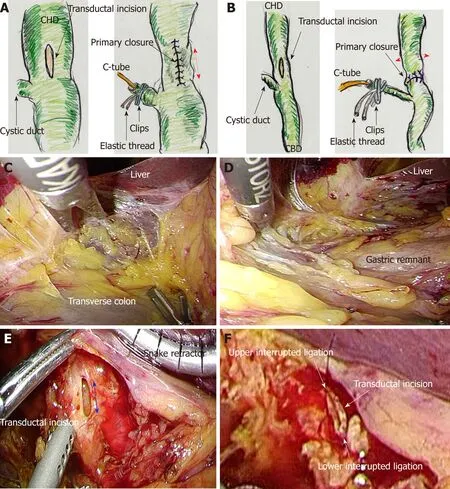
Figure 6 Laparoscopic choledocholithotomy.
ADEQUATELY OPERATE THE CHOLANGIOSCOPE DURING LAPAROSCOPIC CHOLEDOCHOLITHOTOMY
Intraoperative cholangioscopy is an important procedure for observing intraluminal findings and removing stones. Frustrating procedures should be avoided. The duration of intraoperative stone clearance accounts for most of the operative time.Cholangioscopy has only two-way operation. Hence, a dedicated forceps to atraumatically grasp the cholangioscope is a key tool for smart cholangioscope maneuvers and successful laparoscopic choledocholithotomy. Conventional laparoscopic forceps cause severe damage to the surface coating of the cholangioscope. Even mild damage requires very expensive repair, which may reach nearly 10000 USD. Olympus (Product standard number: A66070A) and Karl Storz Endoskope (Product standard number: K33531 PG) provide made-to-order forceps,respectively. Actual forceps we use are shown in Figure 5D. The transductal incision is made along the long axis (Figure 6E). Thereafter, full-layer interrupted sutures should be placed at the upper and lower edges of the transductal incision (Figure 6F),because cholangioscopic maneuvers can easily cause severe laceration of the EHBD along its long axis.
UNEXPECTED THERMAL DAMAGE AROUND THE BILE
DUCT
Cautery-induced injury results in necrotizing loss of ductal and/or perivascular tissues[32]. Cautery, laparoscopic coagulation shears and stronger devices may cause thermal necrosis of adjacent structures[32,99], and may subsequently cause delayed thermal injury[100]. This spread of thermal damage results in biliary complications after surgery[7]. Developed vessels on the surface of the EHBD should be carefully protected from thermal damage[7]. Minimized interrupted sutures and ligation are the first choice to achieve hemostasis near the biliary wall (Figure 4B). If safe hemostasis is not possible with additional suture, a button-shaped electrode with suction and a soft-coagulation system (VIO, Erbe) may be permissible for hemostasis near the EHBD.
CLINICAL MANAGEMENT AFTER LAPAROSCOPIC CHOLEDOCHOLITHOTOMY
An initial cholangiography is performed on postoperative day 4, with contrast agent adjustment according to the purpose of cholangiography. For intraoperative cholangiography, a full-concentration contrast agent with atoxic dye is used to detect even subtle leakage and stenosis. Half-concentration contrast agent without dye is used for postoperative cholangiography, because full concentration may hide small stones. The C-tube is thereafter removed based on the cholangiographic findings and need for ongoing biliary drainage[7]. Management of C-tube drainage is simple;transcystic drainage is easily replaced with transpapillary biliary drainage, using a socalled “rendezvous technique” that uses endoscopic cannulation via the guidewire through the C-tube[101-103]. In contrast, transductal T-tube drainage ineluctably requires drain placement for a period of at least 3 wk[65,66]; long-term drainage results in electrolyte abnormalities, disordered digestion, diarrhea and dehydration. Intake of autogenous bile (i.e., drained bile) is difficult even when bile is cut with cola or snowball syrup[104,105]. Moreover, the discharge with T-tube placement is burdensome.
DISCUSSION
Laparoscopic HBP surgery for benign diseases has several advantages, including excellent magnified visualization and an adequate surgical field located on the right anterior side of the body[7,30,84]. Laparoscopic surgeons should be proficient in a variety of techniques and devices[6,14]; laparoscopic choledocholithotomy requires skillful manipulation of the forceps[30]. This advanced surgery is feasible in the clinical setting[7,30,84]. Even when endoscopic transpapillary biliary drainage is emergently required in patients with acute cholangitis[19,45], subsequent laparoscopic HBP surgery for benign diseases of the EHBD have an excellent clinical course and acceptable outcomes[22,26-28,31].
Laparoscopic choledocholithotomy with transcystic C-tube drainage results in an excellent rate of stone clearance, less bile leakage, less blood loss, acceptable mortality and morbidity rates, shortened hospital stay, and earlier social reintegration than conventional open surgery with transductal T-tube drainage[22,27,69,106-109]. However, in a laparoscopic approach, operative time was prolonged and cost becomes more expensive[110,111]. Overall, we should never forget that laparoscopic choledocholithotomy with transcystic C-tube drainage is the first choice for biliary stones in the EHBD.
Severe acute cholangitis and AOSC easily result in sepsis[17,18]; the elderly population is a target of AOSC[42,44]. Emergent biliary drainage is critical for patients with life-threatening conditions[19]. To preserve the physiological function of Oddi's sphincter, ill-considered use of EST should be avoided[20]. HBP surgeons should make an effort to end conventional open surgery with transductal T-tube drainage[47,49,70].The right upper quadrant of the abdomen provides adequate space for laparoscopic HBP surgery[7,30,84]. One-stage laparoscopic choledocholithotomy has excellent clinical outcomes[22,26-28]and cost-effectiveness[112,113], even though emergent biliary drainage to prevent sepsis[19,45]and complete removal of risk factors for general anesthesia[53-55]are required.
Robotic surgery offers a promising frontier in the field of HBP surgery[114-116];however, laparoscopic approaches are safe and feasible for benign biliary diseases of the EHBD[22,25-30,84]. During recent decades, laparoscopic surgery has been well developed, especially in the field of HBP surgery. Biliary stone in the EHBD is a common disease, and laparoscopic choledocholithotomy is a routine surgery and is not so skill-demanded in many centers nowadays. However, especially in Japan,laparoscopic choledocholithotomy is not a routine surgery in spite of a cover of medical insurance[117,118], and many physicians condone an ill-considered use of EST for biliary stones[20]. Here, actual procedures of laparoscopic choledocholithotomy are described in detail, and also important documents for this advanced surgery are summarized in Table 1. We hope that our article with visual explanation and literature review will be informative for skillful HBP surgeons.
CONCLUSION
Laparoscopic choledocholithotomy is not rocket science. Safe laparoscopic HBP surgery is the recommended approach for benign diseases of the EHBD. I hope that this article results in benefits for these patients.

Table 1 lmportant documents for laparoscopic choledocholithotomy
ACKNOWLEDGEMENTS
All illustrations and schemas were originally drawn by T. Hori. I'm deeply grateful to Daiki Yasukawa (Shiga University of Medical Science, Otsu, Japan) and Yuki Aisu(Kyoto University Graduate School of Medicine, Kyoto, Japan), for their help to successfully perform this advanced surgery and to intensively assess important literatures in this field.
杂志排行
World Journal of Gastroenterology的其它文章
- Hepatocellular carcinoma surveillance: An evidence-based approach
- Cellular therapy: A promising tool in the future of colorectal surgery
- Characterization of hepatitis B virus X gene quasispecies complexity in mono-infection and hepatitis delta virus superinfection
- Plasma microRNAs as potential new biomarkers for early detection of early gastric cancer
- Comparison of Hemospray® and Endoclot™ for the treatment of gastrointestinal bleeding
- Performance of tacrolimus in hospitalized patients with steroidrefractory acute severe ulcerative colitis
