Anterior segment spectral-domain optical coherence tomography in patients with closed globe injury
2019-04-04
Department of Ophthalmology, Huizhou Municipal Central Hospital, Huizhou 516001, Guangdong Province, China
Abstract
INTRODUCTION
Traumatic eye injury is a common cause of ocular morbidity. Eye injuries can be divided into closed and open eye injuries[1-2]. The potential consequences of closed globe injury include hyphema, angle recession, iris root mutilation and lens subluxation. Hyphema is the presence of blood in the anterior chamber of the eye, and is a common manifestation of ocular trauma[3-5]. In most cases, the blood clears from the anterior chamber without significant sequelae. However, permanent damage can occur in some cases when high intraocular pressure (IOP) or corneal blood staining accompanies a hyphema. It is therefore essential to identify whether there are additional injury features associated with traumatic hyphema, such as Descement’s membrane detachment, angle recession, iris root mutilation, or lens subluxation, all of which can be seen with closed globe injuries[6-10]. Identifying whether these features are present may help clinicians to make treatment decisions and plan appropriate surgical intervention if indicated[1-2].
Gonioscopic examination is contraindicated in cases of ocular trauma with hyphema due to increased risk of re-bleeding[11]. In these cases, slit lamp biomicroscopy is the most widely used tool to evaluate the anterior segment in clinic. However, the architectural changes of the corneal endothelium, iris, angle and lens cannot be observed clearly by slit lamp biomicroscopy when there is corneal edema and hyphema. Ultrasound biomicroscopy is a useful tool for anterior segment imaging[12-14]. However, it requires contact with the eye and cannot be used in cases with acute traumatic hyphema. Spectral-domain optical coherence tomography (SD-OCT) with anterior segment scanning software is a noncontact, noninvasive instrument with quick image acquisition and high resolution. SD-OCT may be suitable for anterior segment imaging in patients with closed globe injury.
Our study aimed to evaluate whether SD-OCT can be used as a complementary modality for anterior segment examination in patients with closed globe injuries.
SUBJECTS AND METHODS
This is an observational, cross-sectional study. This study had been approved by the Ethics Committee of Huizhou Municipal Central Hospital. The study proposal had been submitted to the Ethics Committee of Huizhou Municipal Central Hospital before it began. Then the Ethics Committee members would discuss and proved the study proposal and inform consent was obtained.
Sixteen patients with closed globe injury were recruited consecutively between January 2010 and July 2015 at the Huizhou Municipal Central Hospital in Guangdong, China. Only eyes with hyphema filling at least one third of the anterior chamber volume were recruited. The study was conducted in accordance with the Ethical Standards Stated in the 1964 Declaration of Helsinki with informed consent obtained. Two patients had bilateral injuries. All subjects underwent complete ophthalmic examination to measure visual acuity and non-contact tonometry to measure IOP. Patients underwent slit lamp biomicroscopy on the affected eye. The anterior segment architectures were imaged with SD-OCT anterior segment scan software mode by the same doctor (Deng RD). SD-OCT images were recorded and compared with slit lamp biomicroscopy examination.
AnteriorSegmentExaminationwithOpticalCoherenceTomographySD-OCT imaging was performed using Cirrus HD-OCT (software version 5.1.1; Carl Zeiss Meditec). The acquisition rate of the Cirrus HD-OCT was 27, 000 A-scans per second; the transverse and axial resolutions were 15 μm and 5 μm, respectively. An anterior segment scan mode (Anterior Segment cube) allowing for 512×128 axial scans with a scan area of 6×6 mm2was integrated into the machine.
Table1Demographiccharacteristicsandcausesofinjuryfor16patientswithclosedglobeinjury
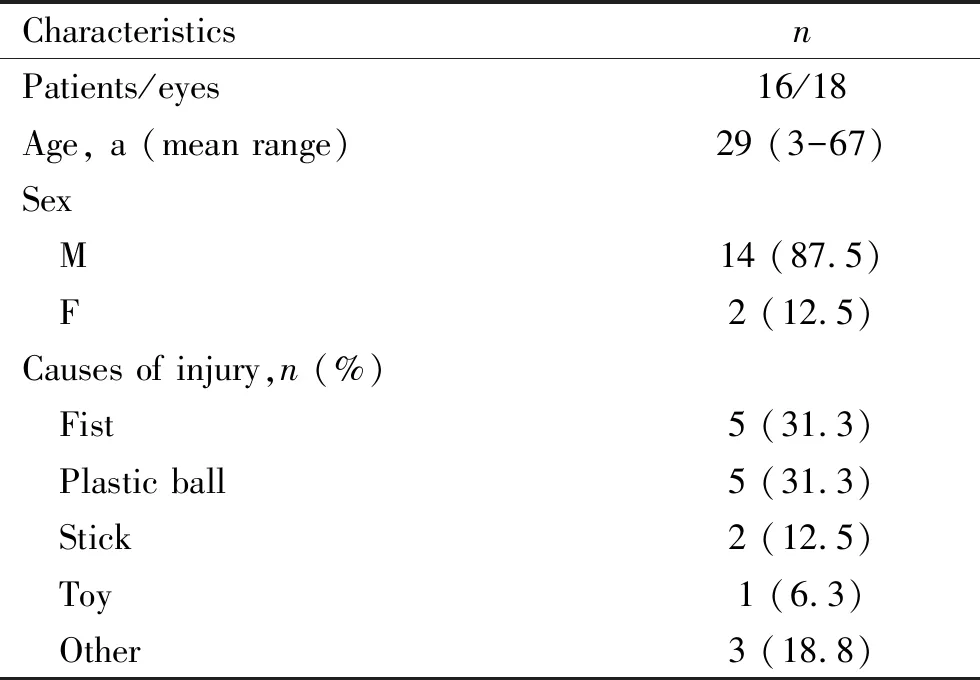
CharacteristicsnPatients/eyes16/18Age, a (mean range)29 (3-67)Sex M14 (87.5) F2 (12.5)Causes of injury,n (%) Fist5 (31.3) Plastic ball5 (31.3) Stick2 (12.5) Toy1 (6.3) Other3 (18.8)
RESULTS
We examined 18 eyes in 16 patients with closed globe injury. The average age of the patients was 29 (range: 3-67) years. The most common etiologies for closed globe trauma included injury by fists (n=5), a plastic ball (n=5) and a stick (n=2). Demographic characteristics are shown in Table 1.
The anterior segment architectures were recorded for all 16 patients with traumatic hyphema in all 18 involved eyes (Figure 1). Corneal endothelial damage is detected on OCT images as a high reflective line. Descemet membrane folding or tearing is seen as a clear, reflective line (Figure 1A, white arrow) emanating from the cornea. In cases with hyphema, it shows scattered moderate signal (Figure 1B, white arrow) on OCT images whereas a blood clot gives a high bolus signal inside the anterior angle or pupillary area (Figure 1C, white arrow). In angle recession, the ciliary body annuliform muscle is separated from the longitudinal muscle. In ocular trauma cases with angle recession, a deep anterior chamber, and a wide, round and blunt angle (Figure 1D, white arrow) can be seen on OCT images. Iris root mutilation has discontinuation low reflective signal (Figure 1E, white arrow). The lens has mild to high reflective signal in the anterior chamber (Figure 1F, white arrow). Anterior vitreous opacity is detected as a high, punctiform or girdle-shaped reflective signal behind the iris (Figure 1G, white arrow).
All 18 eyes had hyphema filling at least one-third of the anterior chamber volume detected by both OCT and slit lamp examinations. Sixteen eyes (88.9%) had corneal edema and corneal abrasion detected on both slit lamp biomicroscopy and OCT examination. Among the eyes with corneal edema and abrasion, 7 eyes had a Descemet membrane tear only detectable with OCT and 6 eyes had angle recession detected with OCT alone. Additionally, there were cases of lens dislocation (n=3), traumatic cataract (n=2), iris root break (n=3) and anterior vitreous hemorrhage (n=2) that were detectable with OCT but were not seen with slit lamp biomicroscopy due to obscuration by the present hyphema. The OCT findings are summarized in Table 2.
Positive findings with OCT examination would significantly guide the clinical management. Traumatic eyes with Descemet membrane tear only detectable with OCT were monitored more closely on corneal edema, anterior chamber bubble injection would be recommended when necessary. IOP monitoring was necessary for whose traumatic eyes with angle recession only detected with OCT. For those with lens dislocation, traumatic cataract, iris root break and anterior vitreous hemorrhage detected with OCT would be observed closely and further surgeon management would be performed on those patients.
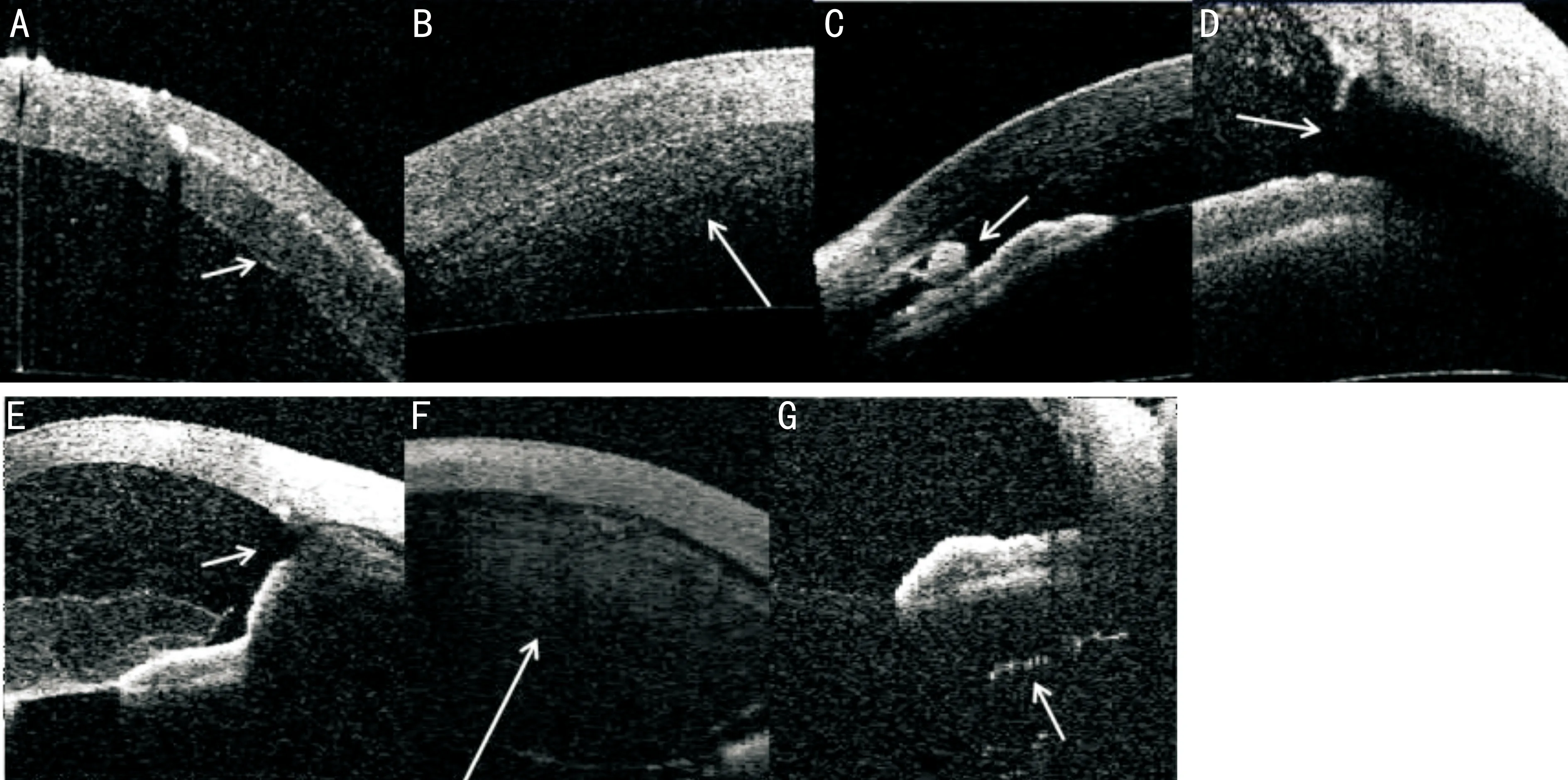
Figure1AnteriorsegmentarchitecturalchangesonOCTimagesincaseswithtraumatichyphema
A: Descemet membrane folding or tearing; B: Fresh blood in the anterior chamber; C: A blood clot inside the anterior angle or pupillary area; D: Angle recession; E: Iris root mutilation; F: The lens; G: anterior vitreous opacity.
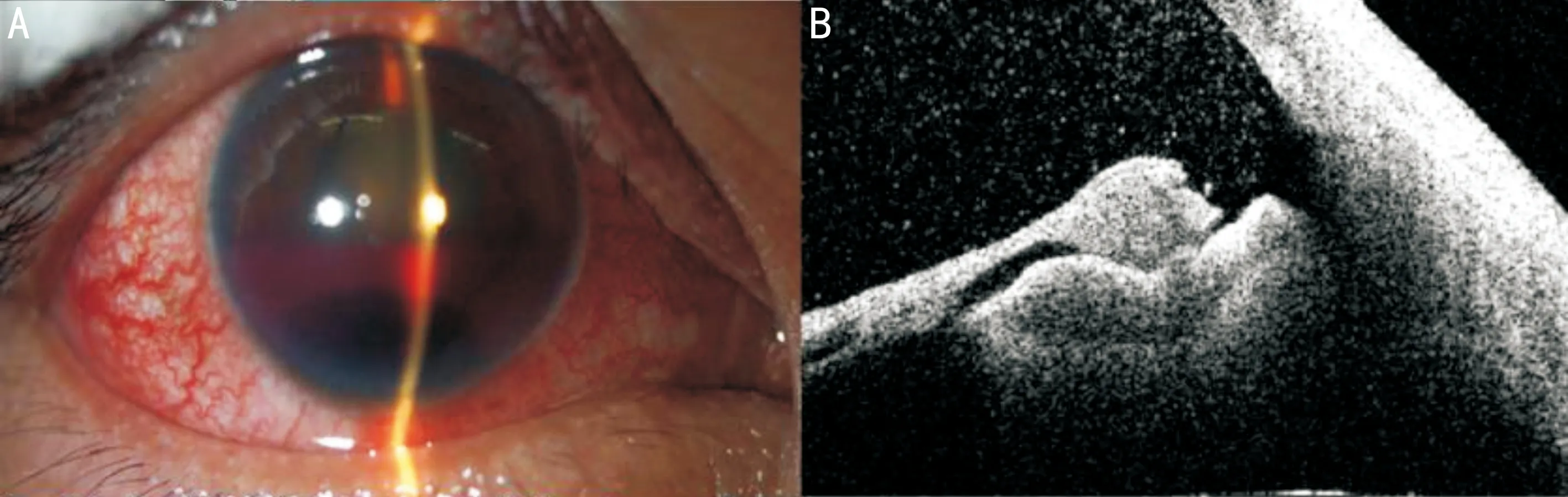
Figure2IllustratesslitlampbiomicroscopyandOCTimagesina47-yearoldmalepatientwithclosedglobeinjuryandtraumatichyphemacausedbycontactwithafist
A: Slit lamp biomicroscopy examination showed corneal edema and hyphema; B: OCT imaging showed angle recess in the inferior quadrant, which could not be detected on the slit lamp biomicroscopy examination.
Table2ComparisonoftheclinicalfeaturesoftheanteriorsegmentassessedbySD-OCTandslitlampbiomicroscopywithSD-OCTasthegoldstandard
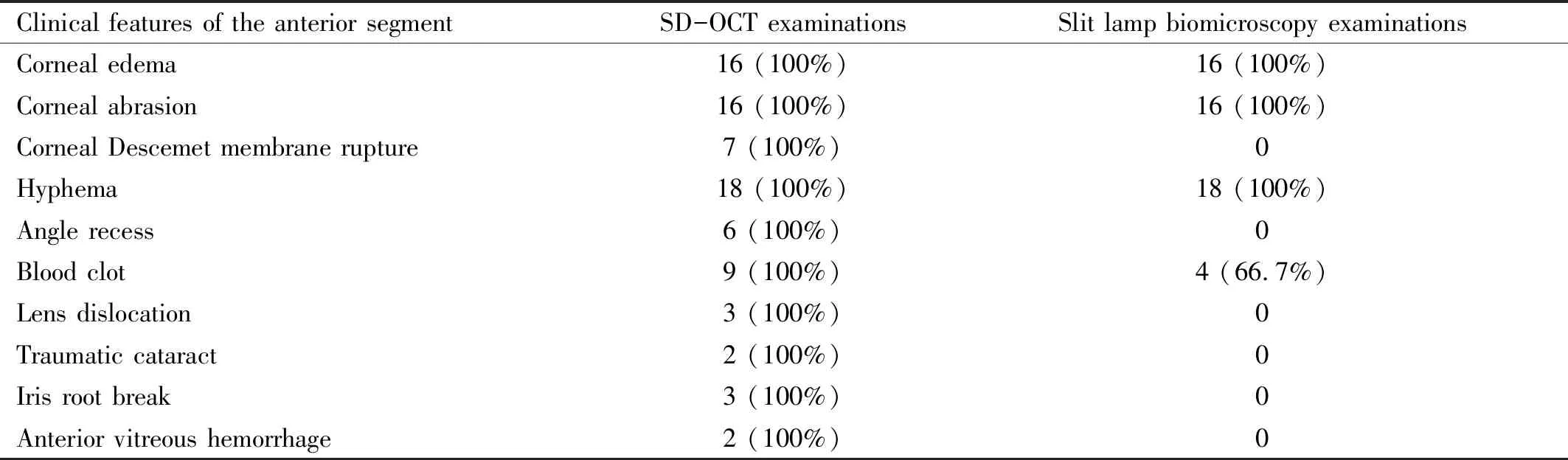
n(%)
SD-OCT: Spectral-domain optical coherence tomography.
ExampleA 47-year old male patient suffered from closed globe injury and traumatic hyphema caused by contact with a fist. Slit lamp biomicroscopy examination showed cornea edema and hyphema (Figure 2A), whereas OCT imaging showed angle recess in the inferior quadrant (Figure 2B), which could not be detected on the slit lamp biomicroscopy examination.
DISCUSSION
Closed globe injury is a common cause of ocular injury seen in the clinical setting[2]. Changes to the architecture of the anterior segment in patients with closed globe injury include corneal damage, hyphema, angle recession and lens dislocation. Our study recruited 16 patients with closed globe injury from a single institution to compare the ability of OCT and slit lamp biomicroscopy to detect the complications that sometimes accompany hyphema. Our results suggest that OCT is superior to slit lamp biomicroscopy for detecting anterior segment architectural changes, especially in the presence of media opacities.
Corneal abrasion, endothelial damage, and tears to the Descemet membrane are common features in patients with a closed globe injury[15-16]. However, patients with ocular trauma may also have significant corneal edema and corneal opacity, making it difficult to detect these potential complications. In our study, 16 eyes had corneal damage detected by both OCT and slit lamp biomicroscopy. Corneal Descemet membrane tear was seen in 7 eyes, but was only detectable with OCT and was not seen by slit lamp biomicroscopy. In the presence of corneal edema, slit lamp biomicroscopy was unable to identify Descemet’s membrane tear, iris and angle damage, and lens dislocation. On OCT, normal corneal epithelium and endothelium are seen as highly reflective signal lines, whereas the corneal stroma produces mid to low reflective signal. The complications that sometimes accompany hyphema after closed globe injury are much easier to detect with OCT. Additionally, OCT is a non-contact device, and its use does not require topical anesthesia, making it suitable for cases involving ocular trauma.
Post-traumatic hyphema is due to a break in the iris blood vessels. Micro-hyphema may be absorbed spontaneously after 3d to 7d with ocular rest. Hyphema occupying more than 50% of the anterior chamber volume does not absorb spontaneously[17]. Corneal blood staining resulting from hyphema occurs more frequently in eyes with corneal endothelial dysfunction[17]. Blood clotting can obstruct the pupil and angle, and may lead to elevated IOP and secondary glaucoma. Patients with angle recess and secondary glaucoma have the same symptom with chronic glaucoma without early symptoms or pain, visual acuity would not be affected until advance glaucoma, so regular following up and monitoring IOP is very necessary. In our study, all affected eyes had hyphema occupying at least one-third of the anterior chamber. Five eyes in 5 patients were performed irrigation of anterior chamber during the follow-up. Cirrus OCT was superior to slit lamp examination in the detection of associated anterior segment injuries in the eyes of patients with hyphema. In our study, angle recession, traumatic cataract, iris root break and anterior vitreous hemorrhage were also detected with OCT but not with slit lamp because of the hyphema.
Ultrasound biomicroscopy is an useful tool to examine the anterior segment in post-traumatic eyes. It can provide high-resolution images regardless of media opacity. However, local anesthesia and water irrigation is needed during the examination[18-19]. On the other hand, Cirrus OCT is a fast, non-contact device that can capture high-resolution images. Iris root mutilation and angle recess could be seen clearly with OCT in our study. Previous studies have reported that approximately 67% patients with closed globe injury and hyphema have accompanying angle recession and about 10% of these patients developed angle recess glaucoma during long-term follow-up[20-21]. Therefore, early identification of angle recess following blunt trauma is essential. To our knowledge, this is the first case series using Cirrus OCT to examine closed globe injury. Previous studies have focused on using ultrasound to examine the anterior segment in eyes following ocular trauma[6].
In eyes with closed globe injuries, Cirrus OCT was superior to slit lamp biomicroscopy in detecting changes to the anterior segment architecture, especially in eyes with media opacities.
