Superior sinus venosus atrial septal defect
2018-11-19KonstantinosTheodoropoulosAlexandrosPapachristidisGiovanniMasoeroMichaelPapitsasValentinaCospiteFulyaAvciDemirDanielSadoMarkMonaghan
Konstantinos C Theodoropoulos, Alexandros Papachristidis, Giovanni Masoero, Michael Papitsas,Valentina Cospite, , Fulya Avci Demir, Daniel M. Sado, Mark J. Monaghan
1Department of Cardiology, King’s College Hospital, King’s College London, London, UK
2Department of Cardiology, St Thomas' Hospital, London, UK
Keywords: Atrial septal defect; Cardiovascular magnetic resonance; Sinus venosus defect; Transesophageal echocardiography
Atrial septal defect (ASD) is the third commonest congenital heart disease in adults. The most common type of ASD is the ostium secundum accounting for 75%-80% of all ASDs. Less common are the ostium primum (accounting for 15% of all ASDs), the sinus venosus defect (5%-10%)and the coronary sinus defect (less than 1%).[1,2]
A 72-year-old female with medical history of coeliac disease had surgery for breast cancer and Paget’s disease of the nipple. After surgery she commenced chemotherapy with paclitaxel and trastuzumab (Herceptin), and she was monitored for drug-induced cardiotoxicity with thransthoracic echocardiogram (TTE) every three months. The first two TTEs showed normal left ventricular (LV) systolic function(EF: 55%-60%) and mild aortic regurgitation (AR). The third TTE, showed worsening of the AR at the level of moderate and three months later a new TTE showed low normal LV systolic function (EF:53%) with normal LV size,moderate AR and right heart chambers dilatation (Figure 1).The right ventricular systolic pressure was normal in all the studies. The patient was asymptomatic. The mild deterioration of LV systolic function could be attributed to chemotherapy (which was stopped at this point), and a transesophageal echocardiogram (TEE) was organised to further assess the severity of AR and its possible impact on LV function. The TEE confirmed the presence of moderate AR(Figure 2) and mild to moderate dilatation of the right atrium and right ventricle. Interestingly, a superior sinus venosus atrial septal defect was detected with an associated left to right shunt (Figures 3 and 4). Not all pulmonary veins could be visualised, and a cardiovascular magnetic resonance (CMR) was performed to clarify the pulmonary venous drainage. The CMR showed both left pulmonary veins draining into the left atrium (LA), however on the right side,two veins (from the basal and mid right lung) were draining into the LA, and the superior vein was draining into the superior vena cava (Figure 5). The pulmonic to systemic blood flow ratio (Qp/Qs) was calculated as 1.5. CMR also showed normal LV systolic function, mild right atrial dilatation and moderately dilated right ventricular cavity (EDVi:132 mL/m2) with normal systolic function. The patient was referred to adult congenital heart disease service for review,where conservative management was decided with annual clinical follow up. With regards to aortic regurgitation, annual clinical follow up and two-yearly TTE surveillance was arranged.

Figure 1. Right heart chambers dilatation. (A): Transthoracic echocardiogram, apical four chambers view in end-diastole, showing the dilatation of the right ventricle; and (B): TTE, apical four chambers view in end-systole, showing the dilatation of the right atrium. RA: right atrium; RV: right ventricle.
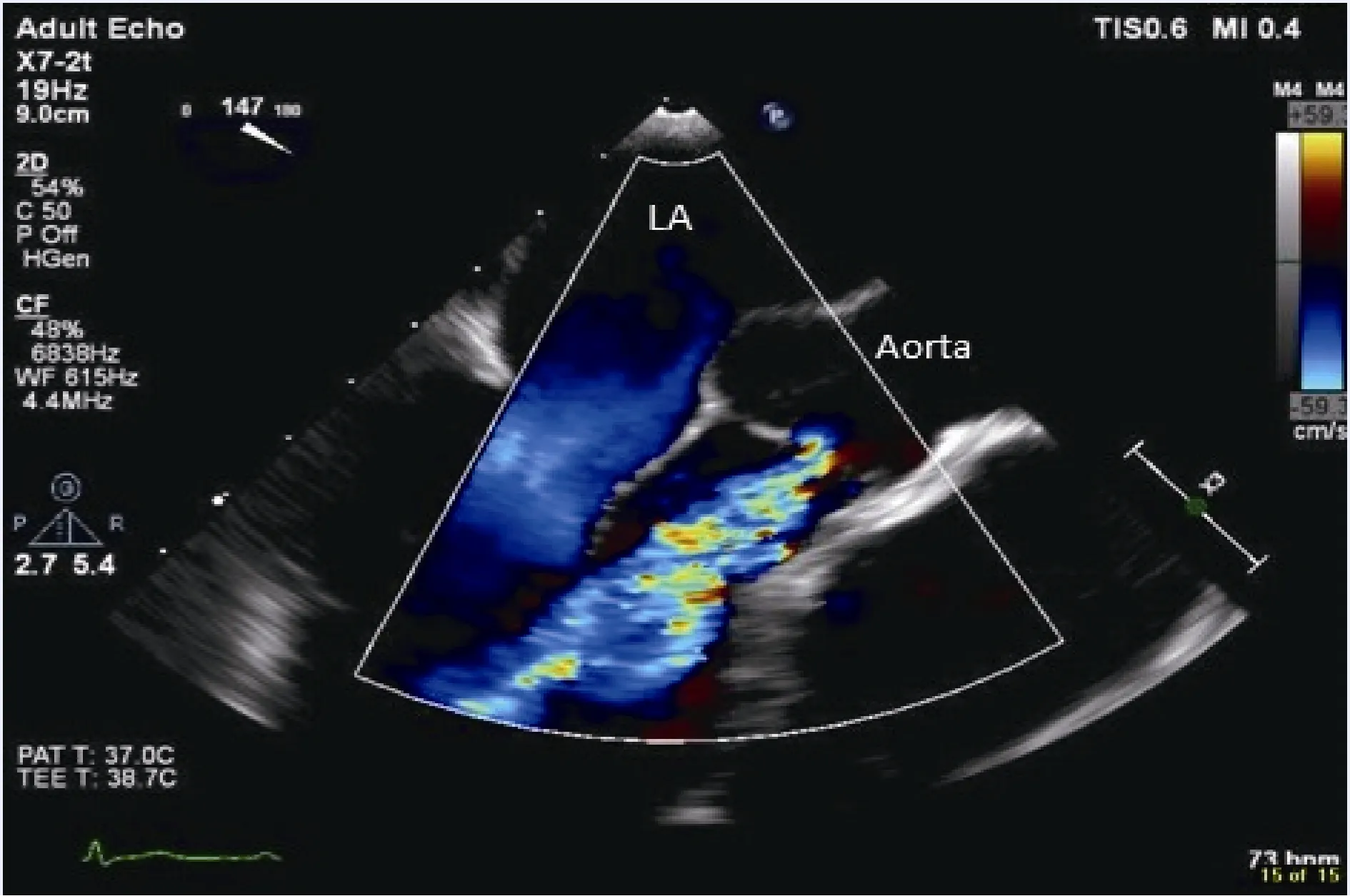
Figure 2. Aortic regurgitation. Transesophageal echocardiogram, midesophageal aortic valve long-axis view with colour Doppler, showing moderate aortic regurgitation (Vena Contracta: 0.45 cm). LA: left atrium.
Sinus venosus atrial septal defects (SVASDs) are rare congenital cardiac abnormalities (5%-10% of all ASDs)that occur at the posterior aspect of the interatrial septum,close to the junction of the superior or inferior vena cava with the right atrium. They involve the portion of the atrial wall that derives from the sinus venosus and they are often associated with partial anomalous pulmonary venous drainage from the right lung. SVASDs result in a left to right shunt at the atrial level, since the left atrial pressure is greater than the right. They may not cause symptoms in childhood, however patients may become symptomatic with ageing. SVASDs have nonspecific clinical manifestations such as exertional dyspnea, arrhythmias, paradoxical embolism or, very rarely, they may cause inadvertent passage of pacing leads/catheters to the left chambers during interventions.[3]The long term haemodynamic effect is volume overload of the right heart, as a result of the shunt, which can cause pulmonary hypertension if the shunt is significant.Furthermore, the frequently coexistent anomalous pulmonary venous drainage (in around 90% of SVASDs) contributes to additional left-to-right shunting, thus, the development of Eisenmenger physiology can occur earlier compared to an isolated ASD.[4]SVASDs can be misdiagnosed as primary pulmonary hypertension, thus they should al ways be suspected in case of unexplained right heart chambers dilatation.[5]Transthoracic echocardiography has low sensitivity for the detection of SVASDs (10% approximately) due to their posterior location.[6]Other imaging modalities like TEE, CMR and ECG gated multidetector cardiac computed tomography (CT) can reveal the presence of SVASDs and coexistent anomalous pulmonary venous drainage. Repair of an ASD is indicated when the defect is large, there is right heart dilatation with pulmonary hypertension and Qp/Qs > 1.5. However, the repair is contraindicated in case of severe irreversible pulmonary hypertension with bidirectional or right-to-left shunt (Eisenmenger physiology), as closure would provoke acute decompensation of the right ventricle.[2]The treatment of choice for SVASD is surgical repair of both SVASD and possible coexistent abnormal pulmonary venous drainage. Percutaneous closure of the defect with a device is technically difficult, because of the lack of adequate rim and the need of redirecting the abnormal pulmonary veins. However, cases of percutaneous closure of an SVASD have been previously described.[7]
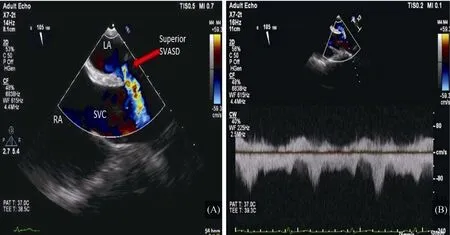
Figure 3. Sinus venosus atrial septal defect. (A): Transthoracic echocardiogram, bicaval view with colour Doppler, showing the superior sinus venosus atrial septal defect (red arrow); and (B): TEE, bicaval view with continuous wave Doppler showing the left to right shunt. LA:left atrium; RA: right atrium; SVC: superior vena cava.

Figure 4. Sinus venosus atrial septal defect. Transthoracic echocardiogram, bicaval view with colour 3D zoom showing the blood flow from the left atrium to the superior vena cava. LA: left atrium; SVC: superior vena cava.

Figure 5. Partial anomalous pulmonary venous return. (A): CMR showing the two left pulmonary veins and the right inferior and right middle pulmonary veins (blue arrows) draining in the left atrium; and (B) CMR, showing the right superior pulmonary vein draining in the superior vena cava (red arrow). LA: left atrium; CMR: cardiovascular magnetic resonance; SVC: superior vena cava.
In conclusion, an SVASD was found incidentally in a 72-year old female during a TEE, which was performed for aortic regurgitation assessment. Even though our patient had dilated right heart chambers, she had no pulmonary hyper-tension and remained asymptomatic. The lack of symptoms in combination with Qp/Qs of 1.5 was reassuring and conservative management with annual clinical follow up was decided. Sinus venosus defects should always be ruled out with other imaging modalities (TEE, CMR or CT), when an obvious cause of right heart chambers dilatation cannot be found with transthoracic echocardiography and special attention should be paid to identify the drainage of all pulmonary veins.
Acknowledgment
The author declare that there is no conflict of interest.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Association between the level of CD4+ T lymphocyte microRNA-155 and coronary artery disease in patients with unstable angina pectoris
- Repeated measurement of growth-differentiation factor-15 in Chinese Han patients with post-myocardial infarction chronic heart failure
- Analyses of risk factors and prognosis for new-onset atrial fibrillation in elderly patients after dual-chamber pacemaker implantation
- Transradial supra-aortic arteries interventions: a good option for elderly patients
- Double-vessel very late stent thrombosis following Resolute Onyx zotarolimus eluting stents implantation in an octogenarian
- Orthostatic hypotension, an often-neglected problem in community-dwelling older people: discrepancies between studies and real life
