Transradial supra-aortic arteries interventions: a good option for elderly patients
2018-11-19GianlucaRigatelliMarcoZuinFabioDellAvvocataSaraGiattiRameshDaggubati
Gianluca Rigatelli, Marco Zuin, Fabio Dell’Avvocata, Sara Giatti, Ramesh Daggubati
1Section of Cardiovascular Diagnosis and Endoluminal Interventions, Rovigo General Hospital, Rovigo, Italy
2Department of Cardiology, Rovigo General Hospital, Rovigo, Italy
3Cardiac Catheterization Laboratories, Winthrop University Hospital Mineola, NY, United States
Keywords: Angioplastica; Arteries interventions; The elderly
1 Introduction
Peripheral arterial disease (PAD) is the consequence of atherosclerosis in the arteries of carotid, vertebral, abdominal mesenteric, renal, and extremity arteries with a prevalence increasing with. Carotid Occlusive disease is one of the most common site for atherosclerosis development: Endoatherectomy and Carotid artery stenting (CAS) have been shown to achieve similar outcomes and costs[1,2]especially in high-risk patients as very often elderly patients with multiple atherosclerotic localizations are. The performance of supraaortic diagnostic and interventional procedures via the radial artery(RA) is growing all over the world thanks to lower risk of access site complications, lower chance to embolizing debries by touching the aortic arch, lower costs, and increased patient comfort compared to the traditional transfemoral approach (TFA).[3,4]The aim of this paper is to describe the potentiality the TRA can offer in the peripheral interventions of supra-aortic arteries in the elderly.
2 Advantages of TRA for peripheral interventions
As RA is in superficial location, easy access, compressibility, easy control of bleeding, somewhat isolation from adjacent veins, and dual palmar blood supply; hence, the most vascular complications seen with the TFA, such as accesssite bleeding, pseudoaneurysms, arterio-venous fistulas, and limb ischemia are markedly decreased with the TRA.[5]There are also particular anatomic benefits of the TRA for peripheral interventions (TRPI). The ipsilateral TRA allows for excellent support during subclavian artery interventions.In situations where the left carotid artery arises from the innominate artery, the right RA should always be used, to avoid catheter- induced trauma during manipulation in the aortic arch. In the patient with common femoral artery disease, TRA avoids excessive manipulation of catheters in atherosclerotic aortas through a diseased femoral artery, and the potential complications at the TFA site. Finally, using TRA patient comfort is superior by the ability to sit up and ambulate early after the procedure that also reduce potential complications and expenses. Unthinkingly, patients undergoing peripheral vascular interventions would benefit even more from TRA than coronary patients. However, it has not yet been established with large randomized trials.
3 Disadvantages of TRA for peripheral interventions
Small RA size, arterial spasm, anatomic variants, and severe tortuosity at the level of the subclavian artery may make procedural challenges for advancement of guide catheter or long introducer sheath. Since the long sheaths that are often used to traverse the entire length of the upper extremity and the prolonged exposure of the RA may lead to significant spasm. Thus, patient must receive spasmolytic cocktails and well sedation during procedures. The size of the RA is of significant importance only when particular neuroprotection device should be used, such as the Mo. Ma device which is 8F.
4 Techniques
Access site is chosen based upon the vascular territory targeted. Most TRPI should be performed using the left RA,in order to avoid the tortuosity of the innominate artery and the manipulation of catheters in the aortic arch. The only interventions performed from the right RA are those for the right upper extremity, right vertebral artery, and bilateral carotid interventions. Also, poor or absent left radial pulse triggers access from the right RA.
The access is achieved in the regular fashion, and a short introducer sheath at usually 1 Fr smaller than or equal to the intended working size is placed into the RA. After vasodilators are infused locally, the diagnostic angiography is performed using 4-5 Fr diagnostic catheters. The 140-150 cm vertebral-shape catheters allow selective angiography. Occasionally, an Internal Mammary (IM) shape is required to direct the wire from the subclavian artery into the descending aorta. Once the anatomy has been defined, the desired length, size, and shape of the working sheath can be selected.A long, nonhydrophilic 0.035″ wire is typically left in position with the aid of the diagnostic catheter, and the selected working sheath can then be delivered to the target vessel.Moderate-to-deep sedation protocols are advisable throughout the procedure to prevent spasm.
4.1 The transradial approach for percutaneous interventions of supra-aortic arteries
4.1.1 Subclavian artery interventions
The TRA is effective, not only from the standpoint of fewer access site complications, but also as it relates to the stable guide support derived from positioning the introducer sheath in the very proximity of the stenosis (Figure 1). (1)access the RA with a short sheath and perform angiography with a 5 Fr, 100 cm Multipurpose catheter; (2) once the anatomy is established, a 45 cm-long, 6 Fr or 7 Fr introducer sheaths should be used for ipsilateral TRA, and advanced just distal to the distal end of the subclavian lesion;(3) cross the lesion with an 0.035 inch angled stiff, hydrophilic glidewire; (4) predilate the stenosis with an undersized balloon; (5) advance a 5 Fr Pigtail catheter into the transverse aorta to visualize the aorto-subclavian junction by aortography; and (6) complete the procedure in the usual fashion, using bony landmarks for positioning the stent.

Figure 1. Revascularization of chonic total occlusion (CTO) of the subclavian artery through the ipsilateral radial access. (A): Preoperative angiography; (B): recanalization by mean of coronary CTO equipment and angiography of the descending aorta; and (C) final angiography.
An additional advantage of TRA approach for subclavian artery stenosis is to control properly the origin of internal mammary artery in patients with Left internal mammary artery coronary bypass grafting, avoiding eventual pintching.
4.1.2 Carotid artery interventions
Carotid artery stenting is an accepted treatment modality as an alternative and even superior to carotid endarterectomy for revascularization of atherosclerotic internal carotid artery stenosis in patients who are at high risk for surgery.[6]
Traditionally, the femoral approach is usually used. The TRA is challenged due to the acute angle between the common carotid artery and subclavian artery. However,with the currently available equipment, the TRA for carotid stenting is recommended in two situations: stenting of the right carotid artery when the aortic arch is severely diseased;and stenting the left carotid artery when it arises from the innominate artery. (1) access the right RA with a 6 Fr, 90 cm Shuttle sheath and advance to the innominate artery; (2)use a 5 Fr Simmons-1 catheter (Terumo Corporation) is a main catheter to assess the common carotid artery. For contralateral TRA, the 5 Fr Tig-1 Optitorque catheter (Terumo Corporation) or a Simmons -2 or 3 are an alternative catheter; (3) advance a 0.035″ Terumo soft guidewire wire into the external carotid artery or deep in the common carotid artery away from the origin of the internal carotid artery,and advance the long-sheath/Simmons catheter until the common carotid artery is reached in a stable position slightly withdrawing the diagnostic Simmons (Figure 2). For the left carotid artery a larger Simmons should be used over a Terumo soft guidewire, in the same fashion as for the right carotid artery (Figure 3); and (4) the rest of the procedure is performed in the standard fashion. Bilateral CAS from the Right RA cab could be done in selected patients (Figure 4).

Figure 2. Right carotid artery stenting through the right radial artery. (A): Selective angiography with a Simmons diagnostic catheter;and (B): control angiography after successfull carotid artery stenting. The arrows indicate the tip of the catheter engaging the target vessel.
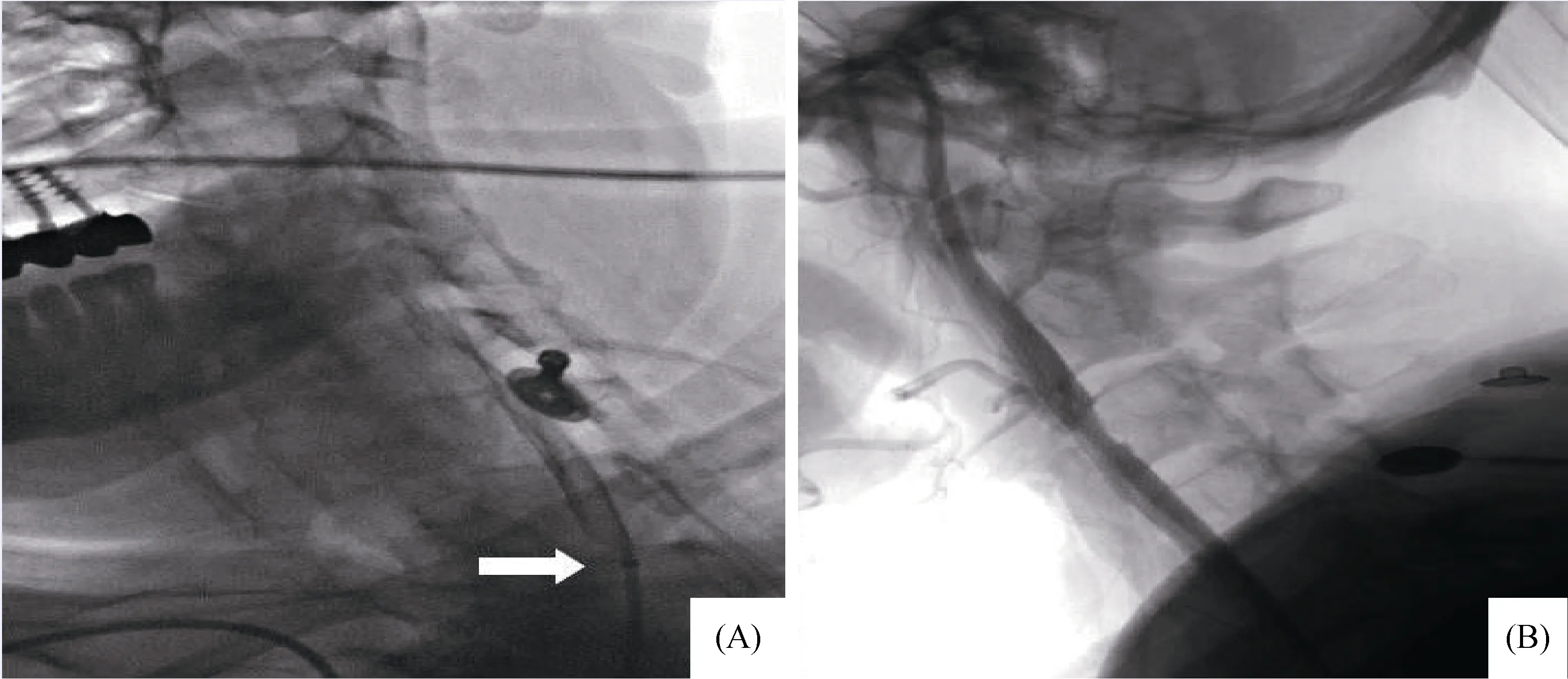
Figure 3. Left carotid artery stenting through the right radial artery. (A): Selective angiography with a Simmons diagnostic catheter;and (B): control angiography after successfull carotid artery stenting. The arrow indicates the tip of the catheter engaging the target vessel.
When the direct cannulation of the right or left common carotid artery is not feasible, and alternative technique including a loop of both diagnostic and long sheath into the aortic arch in order to cannulate indirectly the targeted vessel can be occasionally performed.[7-9]
4.1.3 Vertebral artery interventions
Angioplasty and stenting of the vertebral artery stenosis is a relatively new alternative modality of management. A recent study has documented the safety and efficacy of the TRA to this intervention.[10]Stenting of the vertebral artery is best achieved from ipsilateral TRA. (1) access the ipsilateral RA with a 4 or 5 Fr, 90 cm long introducer sheath; (2)position the tip of the sheath just distal to the take- off of the vertebral artery; and (3) regular PTCA guidewires, balloon catheters, and coronary stents should be used. Predilation of the lesion should be done with low pressure (between 4 atm and 6 atm). The stent should be deployed at low pressure(8–10 atm).
The procedure should be divided into two stages for intracranial vertebral or basilar artery occlusions. In the first stage, the lesion should be dilated using a 1.5 × 10 mm or 1.5 × 12 mm PTCA catheter at 4–6 atm in order to establish distal flow. In the second stage, the patient should be brought to the catheterization laboratory after 24 h and the lesion should be stented using a coronary stent at 8–10 atm.This strategy should be used to prevent hyperperfusion brain injury.

Figure 4. Bilateral carotid artery stenting uin the same session throught the rigth radial artery. (A): Rigth carotid artery angiography;(B): advancement of the guiding sheath; (C): final angiography after stenting, left carotid artery stenting through the rigth radial access; (D):preoperative angiography; (E): advancement of the guiding sheath; and (F): final angiography.
4.2 Potential caveat and benefits in elderly subjects
Elderly people usually have elongated tortuous vessels with a huge amount of calcium which all can increase the risck of cerebral embolization caused by catheter manipulation through the subclavian artery. Some tricks and tips,[11]usually can allow for proper vessel cannulation. Use of particular neuroprotection device such as the Mo. MA[12]or others should carefully planned because they need at least a radial artery size of a diameter of 2.5 mm to allocate a 8F sheath: the 8 in 7 sheath option can be used occasionally.Potential benefits may include: easy management of the puncture site; rapid mobilization, short term hospital stay,and a decrease of the risk of dislodge plaques debries caused usually by manipulation of the catheter to incannulate common carotid or subclavian vessels from the femoral approach, especially in hostile aortic arch.
5 Conclusions
Most peripheral interventions are easily accessible from the TRA offering several advantages, including the wellestablished lower risk of post-procedural bleeding, which is particularly harmful in elderly people.
Acknowledgment
There was no conflict of interests to be declared.
杂志排行
Journal of Geriatric Cardiology的其它文章
- Association between the level of CD4+ T lymphocyte microRNA-155 and coronary artery disease in patients with unstable angina pectoris
- Repeated measurement of growth-differentiation factor-15 in Chinese Han patients with post-myocardial infarction chronic heart failure
- Analyses of risk factors and prognosis for new-onset atrial fibrillation in elderly patients after dual-chamber pacemaker implantation
- Double-vessel very late stent thrombosis following Resolute Onyx zotarolimus eluting stents implantation in an octogenarian
- Orthostatic hypotension, an often-neglected problem in community-dwelling older people: discrepancies between studies and real life
- Successful capture of red thrombus in acute inferior ST-elevation myocardial infarction
